1. Background
Discharge against medical advice (DAMA) is a complex problem with a multifactorial cause. It is particularly more common in developing countries, like Nigeria, where it is increasingly becoming a major problem in health care delivery (1, 2). DAMA in the pediatric age group is peculiar because the children are usually not involved in decision-making regarding their care. Being minors, decisions relevant to their well-being, including DAMA, are usually taken by their parents or guardians against the background of their own understanding, interests, and welfare (3). It is possible that some of these children involved in DAMA would have opposed such decisions if they had the capacity to do so.
Problems linked to DAMA in both adults and pediatric patients include discomfort for the parents/caregivers and socioeconomic factors (1, 3-8). Previous studies conducted in Nigeria in the past 15 years have reported prevalence of DAMA among the pediatric population to range from 1.2% to 7.5% (1, 4, 5, 9-11). Some of the factors identified as contributors to DAMA included financial constraints, dissatisfaction with care, perceived improvement of clinical condition, high cost of hospital services, inconvenience of hospitalization, desire to seek alternative/complementary medicine, and lack of noticeable improvement in clinical condition (1, 4, 5, 9-11). When DAMA occurs, it often leads to prolonged morbidity and increased risk of mortality (1, 3, 4, 6-8). It is also associated with high readmission rates (12-14), increased cost of care, as well as increased burden on the hospital facilities.
The decline in the socioeconomic status of many Nigerians in recent years and lack of sustainable social support schemes for children’s health care have made them socially and financially vulnerable. Although some studies on DAMA among pediatric patients in Nigeria have been carried out (1, 3-6, 9-11), it is pertinent to study the profile of pediatric DAMA in Ekiti State University Teaching Hospital (EKSUTH), Ado-Ekiti, and by extension Ekiti State, considering the political and economic changes being experienced across most states of the federation in recent times. Furthermore, there is no previous study on pediatric DAMA in Ekiti State. The results can be used to plan evidence-based interventions to reduce the burden of this problem among the pediatric population and to plan pediatric health care delivery in our state and some developing countries like Nigeria.
2. Methods
A cross-sectional descriptive study was conducted at the pediatric unit of EKSUTH, Ado-Ekiti. This center is a state government-owned hospital that changed to a tertiary and referral center in April 2008 for the secondary and primary tiers of health facilities in Ekiti State, Nigeria, which is a geopolitical region with a population of about 2.5 million people. The hospital also receives patients from the neighboring Ondo, Kogi, Kwara, and Osun States within a catchment area of 150 km radius. The hospital has four major (medical, surgery, gynecology/obstetrics, and pediatrics) wards with 300 beds. The pediatric unit manages about 1,000 in-patients and 5,000 outpatients yearly.
The study was conducted at the children emergency ward (CEW) and the special care baby unit (SCBU). The CEW is the unit where children aged between one month and 17 years are admitted while children aged less than 1 month are admitted to the SCBU. These wards are the entry points for in-patients’ pediatric care. The study participants were pediatric patients aged less than 18 years. We obtained all the DAMA cases in the wards between January 2012 and December 2018 from the respective registers, and their case notes were retrieved manually by medical record officers, after which relevant information was extracted by residents in the units using a standardized study proforma. For the purpose of the study, we defined DAMA as a situation in which a patient’s parent(s), caregiver, or guardian chooses to leave the hospital before the attending physician recommends a discharge. The information extracted from the case notes included sociodemographic characteristics, parents’ highest level of formal education and occupation, clinical diagnosis, duration of admission, DAMA signatories, mode of payment for health care, reasons for DAMA, and final outcome. Social class was determined according to the Oyedeji social classification system, which uses parental occupation and the highest level of formal education (15). Data regarding clinical diagnosis were dichotomized into infectious conditions (such as malaria, respiratory tract infections, gastroenteritis, sepsis, and tuberculosis, etc.) and non-infectious conditions (such as perinatal asphyxia, neonatal jaundice, injuries including burns, and nephrotic syndrome). The possible roles of age, religion, parents’ marital status, social class, and health insurance on the type of clinical diagnosis (i.e., whether infectious or non-infectious) were determined.
2.1. Statistical Analysis
Data was entered into the checklist designed for the study and analyzed using the statistical package for social sciences (SPSS) version 23. Categorical variables were summarized using frequencies and percentages, while quantitative variables were summarized using mean mode and median as appropriate. Chi square test was used to assess the relationship between categorical variables. P-values < 0.05 was considered as statistically significant.
2.2. Ethical Consideration
Ethical approval was obtained from the Ethics and Research Committee (EKSUTH/A67/2013/05/05) of the Ekiti State University Teaching Hospital. Ado-Ekiti, Nigeria.
3. Results
A total of 10,483 children were admitted to the CEW (n = 7,015) and special care baby unit (SCBU) (n = 3,468) of EKSUTH during the study period. Overall, 402 patients took DAMA, giving an overall prevalence of pediatric DAMA of 3.8%, out of which 61 were at the SCBU and 341 at the CEW. The prevalence of DAMA at the SCBU and CEW was 1.8% and 4.9%, respectively. We analyzed 233 patients’ case records (127 (54.5%) males vs. 106 (45.5%) females; Male: Female ratio of 1.2: 1). Also, 28 (12.0%) patients were neonates, and majority (75.1%) of them were under five years old (Table 1). The median age of DAMA patients at the CEW was 30.0 months (interquartile range (IQR);12 - 72 months), while that of newborn DAMA was 1 day (IQR; 0.13 - 3.8 days). A higher proportion of the pediatric DAMA patients were Yoruba by ethnicity, and 83.7% of them were Christians by religion. Only 1 (0.4%) patient was enrolled under the National Health Insurance Scheme (NHIS). Majority (94.4%) of the patients had parents that were married (Table 1).
| Characteristics | No. (%), N = 233 |
|---|---|
| Age (mo) | |
| < 1 | |
| Males | 16 (57.1) |
| Females | 12 (42.9) |
| 1 - 12 | |
| Males | 34 (54.8) |
| Females | 28 (45.2) |
| 13 - 60 | |
| Males | 49 (57.6) |
| Females | 36 (42.4) |
| > 60 | |
| Males | 28 (48.3) |
| Females | 30 (51.7) |
| Total | |
| Males | 127 (54.5) |
| Females | 106 (45.5) |
| Religion | |
| Christianity | 195 (83.7) |
| Islam | 38 (16.3) |
| Parents marital status | |
| Married | 220 (94.4) |
| Not married | 13 (5.6) |
| Tribe/ethnicity | |
| Yoruba | 187 (80.3) |
| Igbo | 15 (6.4) |
| Ebira | 15 (6.4) |
| Hausa | 5 (2.2) |
| Others | 11 (4.7) |
| Social class | |
| High | 28 (12.0) |
| Middle | 144 (61.8) |
| Low | 61 (26.2) |
| Patient is on health insurance | |
| Yes | 1 (0.4) |
| No | 232 (99.6) |
3.1. DAMA Signatories
A total of 129 (55%) pediatric DAMA patients had the DAMA form signed by their fathers, 80 (34.3%) by their mothers, 5 (2.1%) by both parents, and 19 (8.2%) by other family members such as aunts, uncles, brothers, and sisters.
3.2. Reasons for DAMA
The reasons for DAMA were not documented in the case notes of 164 (70.4%) patients who took DAMA. Financial constraint was the reason in 43 (18.5%) cases; in 12 (5.2%) patients, caregivers felt the patients had improved; in 12 (5.2%) other cases, the caregivers desired to try alternative care; and in one case, the caregivers discharged the wards against medical advice because they felt they had stayed too long in the hospital and observed no significant improvement. While the final outcome of patients after DAMA was not known in most 218 (93.6%) cases, 11 (4.7%) patients who returned for follow-up fully recovered, 2 (0.8%) recovered with disability, 1 (0.4%) was readmitted, and 1(0.4%) died.
3.3. Duration of Admission
The median duration of admission of the newborn DAMA before DAMA at the SCBU was 3.5 days. Also, one-half (50%) of the patients took DAMA within 3 days of admission. At the CEW, the median duration of admission before DAMA was 24 hours, and the majority (71.7%) of cases took DAMA during 24 - 72 hours of admission (Table 2).
| Duration of Admission | No. (%) |
|---|---|
| SCBU (n = 28) | |
| 0 - 3 days | 14 (50.0) |
| 4 - 7 days | 8 (28.6) |
| > 7 days | 6 (21.4) |
| Median = 3.5 days, IQR = 2-6.5 days | |
| CEW (n = 205) | |
| < 24 hours | 27 (13.2) |
| 24 - 72 hours | 147 (71.7) |
| > 72 hours | 31 (15.1) |
| Median = 24 hours, IQR = 24 - 72 hours | |
3.4. Major Diagnosis of Pediatric DAMA
Severe malaria (27.3%) was the most common diagnosis among DAMA cases at the CEW, while it was severe perinatal asphyxia (25.0%) and neonatal sepsis (25.0%) at the SCBU. Other common diagnoses at the SCBU were neonatal jaundice 6 (21.4%), prematurity 4 (14.3%), neonatal seizures 3 (10.7%), intestinal obstruction 2 (7.1%), aspiration pneumonitis 2 (7.1%); other diagnoses including neonatal anemia, low birth weight, very low birth weight, neonatal tetanus, and multiple congenital anomalies had a prevalence of 3.6% (n = 1 for each).
3.5. Relationship Between Clinical Diagnosis and DAMA by Age Group at CEW
As shown in Table 3, most DAMA cases among the under-fives were due to infectious diseases compared to the older age group where non-infectious conditions predominated (χ2 = 51.94, df= 12, P < 0.0001) (Table 3).
| Clinical Diagnosis | Under-Five Years, N = 147 | Older than Five Years, N = 58 | Chi-Square, Df | P-Value |
|---|---|---|---|---|
| Severe malaria | 43 (29.3) | 13 (22.4) | 51.94, 12 | < 0.0001 |
| Sepsis | 28 (19.0) | 5 (8.6) | ||
| Acute respiratory infection | 20 (13.6) | 1 (1.7) | ||
| Musculoskeletal injuries from crash | 7 (4.8) | 16 (27.6) | ||
| Acute gastroenteritis | 14 (9.5) | 2 (3.4) | ||
| Head injuries | 6 (4.0) | 4 (6.9) | ||
| Febrile seizures | 9 (6.1) | 0 (0.0) | ||
| Sickle cell anemia | 3 (2.0) | 1 (1.7) | ||
| Meningitis | 4 (2.7) | 0 (0.0) | ||
| Burns | 1 (0.7) | 1 (1.7) | ||
| Nephrotic syndrome | 1 (0.7) | 1 (1.7) | ||
| Tuberculosis | 0 (0.0) | 2 (3.4) | ||
| Othersb | 11 (7.50 | 12 (20.6) |
aValues are expressed as No. (%) unless otherwise indicated.
bIntussusception, Snake bite, kerosene poisoning, cerebral palsy, epistaxis, peptic ulcer disease, congenital heart disease, intra-abdominal malignancy, urinary tract infection, rabies, gunshot injury, and epistaxis.
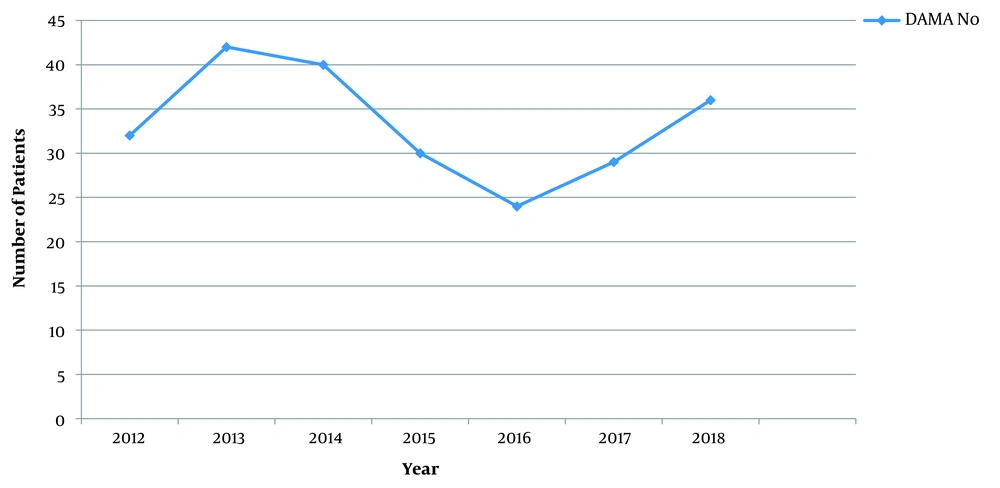
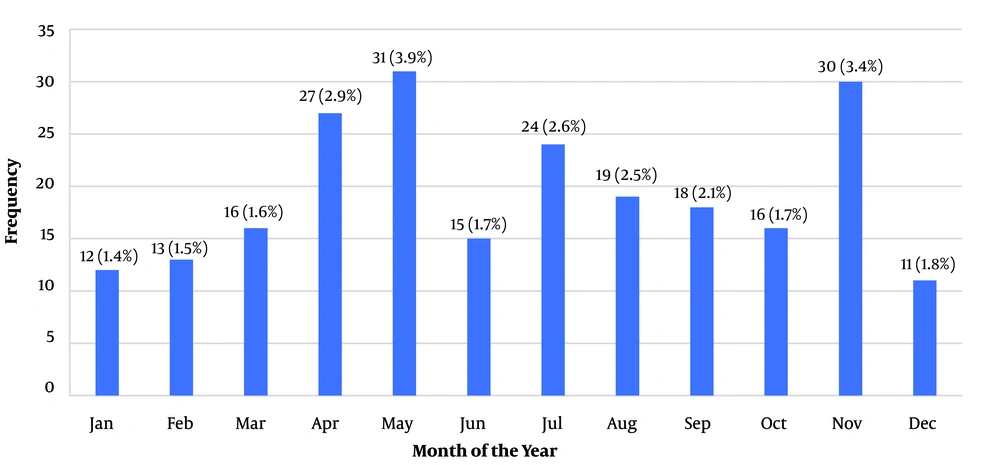
3.6. DAMA Proportion by Year (2012-2018) and Month
The highest number of DAMA cases (n = 40) was in 2013, and the lowest one (n = 24) was in 2016 (Figure 1). Regarding the months of the year, the highest DAMA cases occurred on May 31/793 (3.9%), November 30/881 (3.4%), and April 27/930 (2.9%); the lowest DAMA rate occurred on January 12/885 (1.4%) (Figure 2).
3.7. Relationship Between Clinical Diagnosis and DAMA by Sex, Social Class, Marital Status, and Religion Among All Participants
As shown in Table 4, when data from both the CEW and SCBU were combined and jointly analyzed, only the social class had significant relationship with the type of clinical diagnosis (i.e., whether infectious or non-infectious) as it was found that children from lower socioeconomic class significantly had infectious diseases (P = 0.02).
| Variables | Infectious Disease | Non-Infectious Conditions | Chi-Square, Df | P-Value |
|---|---|---|---|---|
| Sex | 1.71, 1 | 0.19 | ||
| Male | 17 | 50 | ||
| Female | 73 | 33 | ||
| Social class | 8.07, 2 | 0.02 | ||
| Upper | 18 | 7 | ||
| Middle | 76 | 29 | ||
| Lower | 56 | 47 | ||
| Parents marital status | 0.58, 1 | 0.44 | ||
| Yes | 138 | 79 | ||
| No | 11 | 4 | ||
| Religion | 2.27, 1 | 0.13 | ||
| Christianity | 132 | 67 | ||
| Islam | 18 | 16 |
4. Discussion
When DAMA occurs among pediatric patients, the pediatricians are usually disturbed because of the ethical dilemmas involved. The pediatricians are under obligations to act in the best interest of their patients, who are at many times not involved in the decision-making process regarding their care because they are minors. The overall DAMA prevalence rate of 3.8% reported in this study is comparable with the findings of Ndu et al. (9) (3.1%), Eke and Opara (16) (3.8%), and Olasinde et al. (17) (4.1%) in Enugu, Port Harcourt, and Ogbomoso, respectively. However, it is higher than the 2.2% reported by Mohseni Saravi et al. (12) from Iran. The differences may be attributed to the level of social and financial security available for health care in Nigeria and Iran. Nevertheless, some earlier studies (5, 10, 11, 18, 19) have reported higher rates. The difference in the prevalence rates may also be due to the fact that the earlier reports looked at the phenomenon over a shorter period (2 years and below), whereas our study was over a seven-year period. Also, most of their study participants were from the low socioeconomic class (5, 10, 11) as against our study where the majority of patients were in the middle socioeconomic class.
The concept of shared decision-making may help reduce the prevalence of DAMA and protect the pediatricians to a certain extent from ethical dilemmas arising from DAMA (20, 21). Shared decision-making involves physicians and patients making healthcare decisions together by combining the patients' values and preferences for care with the physicians' expertise and knowledge of medical evidence (22). Pediatricians and health care providers involved in children’s care may need to promote this concept in child care practice.
The median age of pediatric DAMA patients at CEW was 30 months, and the average birth interval for most women was 2 years. Therefore, most women often had young infants they were caring for at about the age the older sibling was 30 months; this may be a cause of divided attention. However, our finding is inconsistent with the report by Mohseni Saravi et al. (12), who reported a mean age of four years in their study conducted in Iran. The median birth interval in Nigeria is 30.9 months (23). Women with young and sick infants often try to avoid further stressors, and this may make them decide for DAMA for a sick child once they notice slight improvement in their child's condition (24). Debono et al. (13) in Yeovil, England noted two age peaks for pediatric DAMA in their study, one of which was age less than 2 years; similar to the Nigerian situation (23, 24), they mentioned that parents of children within this age group are likely to have other young children at home, who they need to care for (13). This suggests that pediatricians need to consider family-centered care and the uniqueness of each family setting when managing children as these may have roles in reducing the rate of pediatric DAMA. The median age of DAMA in the newborn unit was 1 day. Having an average number of newborn DAMA at 1 day of age may be related to a cultural belief in the community that a child who will live long will not start his or her life with illnesses or by bringing trouble to the family. This is related to the concept of 'abiku' and ‘ogbanje’ (born to die/born for premature death) among the Yorubas of southwestern and Igbos of the southeastern Nigeria, respectively. Hence, many of such parents often want to take the child home and leave such children for fate to decide or seek alternative (spiritual) care (25). This probably underscores the importance of continuous counseling and detailed information for parents and/or caregivers to understand their children’s clinical condition and the management process. This will help in disabusing their myths and cultural beliefs.
Only one of the study participants was enrolled in the NHIS. This implies that the majority of patients had to pay ‘out of pocket’, which often hinder access to and utilization of health care services. Although only about one-fifth of our study participants stated financial constraints as their reason for DAMA, possibly this was the problem among the majority that did not have any reason(s) stated in their case note as the cause of the DAMA. Financial constraint was not an important reason for DAMA in a study conducted by Roodpeyma et al. (19) in Iran as about 84% of their study participants were on health insurance scheme. Having only one of this study participants enrolled in health insurance scheme reflects the initial poor coverage of the scheme as the study was conducted at least seven years (2012 - 2018) after the commencement of the scheme. The low health insurance enrollment has also been documented by other Nigerian studies. For example, Ndu et al. (9) in Enugu, Nigeria, reported that two (out of 114) participants had health insurance in a study conducted between 2013 and 2015. Increasing the coverage of the health insurance scheme may help reduce pediatric DAMA rate.
In this study, more than 50% of those that signed the DAMA forms were fathers of the patients, a finding similar to reports from other studies (5, 9, 13, 17, 26, 27). This is not surprising because in the study locality just like most African communities, the father is the head of the family, the economic provider, implementer of most family decisions, and most of the times, the sole decision maker (28, 29). Adequate counseling and involvement of the fathers in the care of their children prior to and during the process of hospitalization may play a role in reducing pediatric DAMA (30). Also, an educated and empowered woman/mother has an increased probability of being involved in the decision-making process involving her children as she may be able to contribute to the family resources to reduce the financial burden on the husband/father. This suggests that promoting female education and empowerment may have a role in reducing pediatric DAMA.
Severe malaria was the most common diagnosis of the pediatric DAMA at the CEW, while perinatal asphyxia and neonatal sepsis were the most common at the SCBU in our study. Previous studies have reported similar observations (9-11, 17, 27, 31, 32) although in different orders of frequency. Duru et al. (11) in Bayelsa, Nigeria reported respiratory tract infections as the most common among older children, and Okechukwu (10) in Abuja reported neonatal jaundice as the most common diagnosis among the newborns in their studies. This pattern is probably a reflection of the pattern of pediatric admissions in our facility and other facilities across Nigeria (10, 11). Infectious diseases and perinatal asphyxia remain the leading reasons for hospital admissions among the pediatric age group in Nigeria (33-36). It is possible that measures to reduce the prevalence and burden of these disease conditions might ultimately help in reducing DAMA rate.
Only 1 (0.4%) of our pediatric DAMA was readmitted to our facility; Ndu et al. (9) and Olasinde et al. (17) in Enugu and Ogbomoso, respectively, reported a similar observation. However, our finding (0.4%) is very much lower than the 14% re-admission reported by Onyiriuka (5) in Benin, Nigeria. This low re-admission rates after DAMA may be due to the wrongful belief by patients’ relatives that the patient will not be attended to after DAMA. Also, some healthcare workers believe that they are under no obligation to attend patients re-presenting after DAMA. There is a need to remind healthcare workers that patients (or their legal guardians) are at liberty to give or withdraw their consent for treatment or procedures (37, 38). The obligation of managing patients include giving them adequate information regarding their treatment or procedure and to document their records. Only 5% of our DAMA cases came back for follow-up after their recovery. The outcome of over 90% of DAMA cases was not known. This suggests the need for home visitation/follow-up on phone after DAMA as it may help reduce negative consequences of DAMA and also afford clinicians the opportunity to know the outcomes of these cases. Home visitation is an intervention strategy which has been found to be associated with improvement in health outcomes (39, 40). Hence, home visitation programs/follow-up on phone should be instituted or strengthened in pediatric health care services.
The median duration of admission of pediatric DAMA patients at SCBU was 3.5 days, which is consistent with the report from Enugu, Nigeria; but it is slightly lower than the mean duration of admission reported by Jalo et al. in Gombe, Nigeria (9, 31). More than 75% of the newborn DAMA left within the first 7 days of admission. This finding is similar to previous reports (9, 11, 16, 26, 31, 32), and it may be due to the culture of naming the child at home, usually on the seventh day in most Nigerian tribes. Inconsistent with the report of Okechukwu (10) in Abuja, Nigeria, about 70% of our pediatric DAMA left the hospital between 24 - 72 h of admission. In a study from Kuwait, 56% of pediatric DAMA cases happened within 24 hours, which is in contrast with our observation where about 14% of patients left within less than 24 h (18). This may suggest that many of the patients who took DAMA at the CEW were not prepared to have their wards admitted to the hospital and as soon as they felt their wards had improved decided for DAMA. This probably supports the importance of adequate counseling and communication between patients/caregivers/parents and health care providers.
In our study, the highest pediatric DAMA rate was seen in months May, November, and April and years 2013 and 2014. The years 2013 and 2014 corresponded to some period of global economic meltdown. Both months of April and May represent the planting season and peak of agricultural activities, while November is a peak harvesting period for farmers; hence, the higher rates of DAMA during these periods may be due to the fact that most caregivers would not want to miss their agricultural activities because the study location is an agrarian community. Also, previous reports have documented high malaria admissions during this period of the year (33). Interestingly, malaria was the commonest diagnosis of our pediatric DAMA cases. The association of infectious diseases with both under-five age and lower social status is not surprising as these conditions are two mutual situations that could predispose to many heath conditions, including infectious diseases.
4.1. Limitation of the Study
The main limitation of the study was that it was a retrospective study, and medical records were retrieved manually. This may account for our inability to retrieve some case notes. Moreover, documentation was incomplete in some case notes. Also, the few number of DAMA with complete information for analysis in SCBU could not allow for any inferential statistics. However, despite these limitations, the study provides information on the profile of pediatric DAMA in the study locality for the first time. Furthermore, possible factors fuelling the occurrence of pediatric DAMA were highlighted for appropriate actions by policy makers.
4.2. Conclusions
Pediatric DAMA remains a challenge in pediatric health care services in Ado-Ekiti, Nigeria. Infectious diseases were the predominant conditions among under-fives and children from lower social class. Fathers were the most signatories of the DAMA, and inadequate finance was one of the reasons for DAMA. Accordingly, promoting female education and empowerment, improving family social status through empowerment programs, increasing the coverage of health insurance scheme, as well as practicing family centered care and home visitation/follow-up on phone may play a role in reducing pediatric DAMA.