1. Background
Infant mortality is one of the most important health indicators that affect the level of health and development of countries (1). Infant mortality is a death that occurs before the age of one, and the infant mortality rate is the number of deaths among infants that occur in every 1,000 live births (2). Reducing child mortality, especially infant mortality in the whole world, is one of the millennium development goals (3). According to the World Health Organization (WHO) reports in 2017, 4.1 million (75% of all under-five mortality) occurred within the first year of life. African region had the highest risk of child death under the age of one (51 per 1,000 live births), while the European region showed eight deaths per 1,000 live births. Thus child death in the African region was six times higher than European region (4). According to the reports by CDC in 2016, infant mortality rates per 1,000 live births by race and ethnicity were: 11.4 None-Hispanic black, 9.4 American-Indian/Alaska native, 7.4 native Hawaiian or other Pacific Islander, 4.9 None-Hispanic whites, and 3.6 Asians (2). Globally, in 2017, the infant mortality rate decreased from 65 in 1990 to 29 deaths per 1,000 live births; in the United States, the infant mortality rate was 5.9 per 1000 live births in 2016 (2, 4). In Iran, the infant mortality rate has been decreased from 44 per 1,000 live births in 1990 to 13 in 2017 (5), with the highest rate in neonates (6). According to the report by WHO in 2008, the main cause of death in infants were prenatal causes, diarrheal diseases, lower respiratory infections, Malaria, congenital anomalies, Pertussis, HIV/AIDS, Tetanus, Meningitis, Measles, protein-energy malnutrition, Syphilis, endocrine disorders, Tuberculosis, and upper respiratory infections (7). Preterm birth, low birth weight, sudden infant death syndrome, maternal pregnancy complications, injuries and suffocation are among the causes of infant mortality reported by CDC (2). It is trivial that all of these causes may be changed due to demographic transition, socio-economic, political, and health status of countries during the time (8).
In this study, we used data mining techniques to extract hidden information from a large volume of data and to predict risk factors related to infant mortality (9). Machine learning or data mining is defined as enabling computers to produce evidence for successful decision-making based on past experiences. In recent years, a rapid increase in storage capacity and processing power helped machine learning to exhibit an impressive development (10). Advances in data analysis methods contributed to machine learning enables computers to make an accurate and reliable prediction using even a very small sample size (11). Machine learning techniques such as Decision Trees (DT), Support Vector Machines (SVM), K-Nearest Neighbors (KNN), Naïve Bayes, and Artificial Neural Network (ANN) have been used for classification and prediction about detection, treatment, morbidity, and mortality among patients or population (12).
2. Objectives
As infant mortality is preventable and most of the risk factors are controllable by health policymaking in the community, we performed a study to identify the risk factors and determinants of infant mortality using data mining techniques for prediction, prevention, and promotion of mothers and especially children's health.
3. Methods
This population-based case-control study was conducted in eight provinces of Iran, including Fars, Golestan, Hormozgan, Kohgiluyeh, and Boyer-Ahmad, South Khorasan Kermanshah, Hamedan, and Yazd in 2017. In a stratified cluster random sampling, eight out of 31 provinces from North, East, West, South, and center of Iran were selected. Then five districts were chosen again from North, East, West, South, and Center of each selected province. Thereafter, we randomly selected one urban and one rural health center from each sampled district. According to literature review, considering mother’s education < 5 years as a risk factor (P0 = 0.58, P1 = 0.68, Z0.95 = 1.96, Z(1-β) = 0.90, design effect = 2) and using sample size formula for comparison of proportions, the sample size was estimated as 508 for each of case and control groups. By taking design effect = 2 into account, the sample size for each group reached 1,016. We added some more samples to replace the probable incomplete data. The final sample size was 2,386 (1,076 cases and 1,310 controls). The case group included mothers who had lost an under one-year-old child due to disease or congenital disorder. The control group included mothers who had at least a live child with the age of less than one and had not experienced infant death. Subjects in case and control groups were randomly selected from mothers who were referred to the chosen health centers. Data were collected using researcher-made checklists from mother’s health records. Participants with poor reading or writing skills were interviewed face to face by a trained interviewer to complete the checklist. Checklists included data of demographic status and diseases or disorders as well as the history of mothers and their children.
3.1. Statistical Analysis
Data accuracy and disparities were evaluated. In this study, the outcome variable was considered vital status of infant, while predictor variables included demographic status of mother, history of diseases, events during pregnancy, violence or trauma on mother, and medical records of mothers and their infants such as sex, birth weight, and so on. We employed several data mining algorithms such as AdaBoost classifier, Support Vector Machine (SVM), Artificial Neural Networks (ANN), Random Forests (RF), K-Nearest Neighborhood, and Naïve Bayes to recognize the important predictors of infant death. Sensitivity, specificity, classification accuracy, and F1 score with the following formulas were used for measuring and comparing the performance of the classification methods.
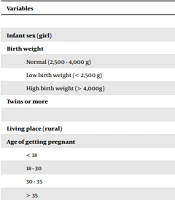
Here TP, TN, FP, and FN stands for true positive, true negative, false positive, and false negative values, respectively (13). Afterward, we used six data mining algorithms to indicate important variables related to infant mortality. Thus factors like mother age at pregnancy, living place, mother literacy and job, consanguineous marriage, gap of pregnancy, worst life event, smoking during pregnancy, child sex, twins, dental disorders, psychological syndrome, gestational diabetes, high blood pressure, and anemia during pregnancy were selected as predictor factors. Among them, 16 variables gained acceptable important scores according to the results of data mining models.
After recognition of important predictors, the binary logistic regression model was used to clarify the role of each selected predictor. Area under receiver operating characteristic curve (ROC AUC) and Hosmer-Lemeshow test were used to measure the calibration and discrimination ability of models.
Data analyses were carried out using STATA-Version 14 and Python 2.7. IDLE software, and the significance level was considered P < 0.05.
4. Results
Of 2,386 studied mothers (1,076 cases and 1,310 controls), 58.7% of the cases and 54.9% of the controls were living in rural areas.
In the case group, 14.2% of mothers were over 35 years old at the time of pregnancy compared to 8.8% in the control group. A total of 52.4% of dead infants were boys. Consanguineous marriage among subjects who had experienced infant death (33.6%) was more prevalent than subjects who had no such experience (25.6%). A total of 4.82% of mothers reported smoking during their pregnancy, and a total of 25.4% of them reported a history of diseases such as anemia, and 5.4% of them had diabetes during their pregnancy. The characteristics of the study subjects in case and control groups are shown in Table 1. After running six data mining algorithms, variables that gained an acceptable importance score were identified.
| Variables | Cases (N = 1,076) | Controls (N = 1,310) |
|---|---|---|
| Child | ||
| Infant sex (girl) | 478 (44.4) | 615 (46.9) |
| Birth weight | ||
| Normal (2,500 - 4,000 g) | 599 (55.7) | 1169 (89.2) |
| Low birth weight (< 2,500 g) | 463 (43.0) | 122 (9.3) |
| High birth weight (> 4,000g) | 14 (1.3) | 19 (1.5) |
| Twins or more | 86 (8.0) | 45 (3.4) |
| Mother | ||
| Living place (rural) | 632 (58.7) | 719 (54.9) |
| Age of getting pregnant | ||
| < 18 | 30 (2.80) | 28 (2.1) |
| 18 - 30 | 681 (63.3) | 859 (65.6) |
| 30 - 35 | 212 (19.7) | 308 (23.5) |
| > 35 | 153 (14.2) | 115 (8.8) |
| Job | ||
| Clerk | 39 (3.6) | 108 (8.2) |
| Housewife | 1008 (93.7) | 1174 (89.6) |
| Labor | 29 (2.7) | 28 (2.1) |
| Literacy | ||
| Illiterate | 71 (6.6) | 53 (4.0) |
| Elementary school | 277 (25.7) | 252 (19.2) |
| Middle school | 271 (25.2) | 272 (20.8) |
| High school | 369 (34.3) | 551 (42.1) |
| University degree | 88 (8.2) | 182 (13.9) |
| Consanguineous marriage | 362 (33.6) | 336 (25.6) |
| Pregnancy gap (y) | ||
| > 3 | 305 (28.3) | 467 (35.6) |
| 1 - 3 | 305 (28.3) | 357 (27.3) |
| < 1 | 78 (7.2) | 46 (3.5) |
| First pregnancy | 388 (36.1) | 440 (33.6) |
| Events During Pregnancy | ||
| Smoking | 60 (5.6) | 55 (4.2) |
| Worst life event | ||
| Experience of family loss | 439 (40.8) | 413 (31.5) |
| High blood pressure | 103 (9.6) | 62 (4.7) |
| Diabetes | 58 (5.4) | 70 (5.3) |
| Anemia | 255 (23.7) | 350 (26.7) |
| Dental disorders | 222 (20.6) | 130 (9.9) |
| Psychological syndromes | 26 (2.4) | 15 (1.1) |
Demographic Characteristics of Subjects in Case and Control Groupsa
For better comparison, we used seven statistical models (logistic regression and six data mining models) for the prediction of outcome using all 16 important predictor variables. The results of model effectiveness shown in Table 2 represent that Naïve Bayes and Random Forest had the highest AUC, F1-score, precision, and sensitivity among data mining algorithms, respectively. These algorithms had high power in predictions of related factors among data mining models (Table 2). The impact value and Odds ratio of each variable using univariate and multivariate regression models are represented in Table 3. Logistic regression model showed the adjusted Odds ratio of consanguineous marriage as 1.44 (95% CI: 1.18-1.76), short pregnancy gap or first pregnancy, worst life event as 1.65 (95% CI: 1.36-2.00), dental disorders as 2.49 (95% CI: 1.90-3.27) and high blood pressure during pregnancy as 1.62 (95% CI: 1.11-2.38) and neonatal weight of under 2500g as 8.13 (95% CI: 6.34-10.42) significantly increased the risk of infant mortality. On the other hand, maternal age of 18-30 and 30-35 years old and mother’s literacy (high school and university degree) all acted as protective factors for infant mortality (Table 3).
| Classifier | AUC | F1-Score | Precision | Sensitivity (Recall) |
|---|---|---|---|---|
| Adaboost classifier | 0.749 | 0.696 | 0.696 | 0.697 |
| Support vector machine | 0.699 | 0.633 | 0.642 | 0.632 |
| Neural networks | 0.754 | 0.697 | 0.696 | 0.697 |
| Random forests | 0.777 | 0.721 | 0.723 | 0.723 |
| K-nearest neighbor | 0.738 | 0.682 | 0.692 | 0.689 |
| Naïve bayes | 0.785 | 0.720 | 0.728 | 0.725 |
| Logistic regression | 0.788 | 0.722 | 0.727 | 0.725 |
F1-Score, Precision, Sensitivity, and Area Under ROC Curve (AUC) of Logistic Regression and Six Data Mining Algorithms
| Variables | Crude OR (95% CI) | P - Value | Adjusted OR (95% CI) | P - Value |
|---|---|---|---|---|
| Living place (rural) | 1.17 (0.99 - 1.37) | 0.05 | 1.18 (0.96 - 1.44) | 0.10 |
| Maternal age | ||||
| < 18 | 0.80 (0.45 - 1.42) | 0.45 | 0.63 (0.32 - 1.24) | 0.18 |
| 18 - 30 | 0.59 (0.45 - 0.77) | < 0.001 | 0.60 (0.43 - 0.84) | 0.003 |
| 30 - 35 | 0.51 (0.38 - 0.69) | < 0.001 | 0.60 (0.43 - 0.85) | 0.005 |
| > 35 | Ref | - | Ref | - |
| Mother’s job | ||||
| Clerk | 0.42 (0.28 - 0.61) | < 0.001 | 0.67 (0.42 - 1.06) | 0.09 |
| Labor | 1.20 (0.71 - 2.04) | 0.48 | 1.25 (0.68 - 2.29) | 0.46 |
| Housewife | Ref | - | Ref | - |
| Consanguineous marriage | 1.46 (1.23 - 1.75) | < 0.001 | 1.44 (1.18 - 1.76) | < 0.001 |
| Gap of pregnancy (y) | ||||
| 1 - 3 | 1.30 (1.06 - 1.61) | 0.01 | 1.42 (1.11 - 1.82) | 0.005 |
| < 1 | 2.56 (1.75 - 3.84) | < 0.001 | 2.70 (1.72 - 4.23) | < 0.001 |
| First pregnancy | 1.35 (1.10 - 1.64) | 0.003 | 1.53 (1.19 - 1.98) | 0.001 |
| > 3 | Ref | - | Ref | - |
| Child sex (girl) | 0.90 (0.76 - 1.06) | 0.21 | 0.92 (0.77 - 1.11) | 0.42 |
| Smoking during pregnancy (yes) | 1.34 (0.92 - 1.96) | 0.11 | 1.11 (0.72 - 1.72) | 0.61 |
| Mother education | ||||
| Elementary school | 0.82 (0.55 - 1.21) | 0.32 | 0.89 (0.56 - 1.39) | 0.60 |
| Middle school | 0.74 (0.50 - 1.10) | 0.14 | 0.71 (0.45 - 1.13) | 0.15 |
| High school | 0.49 (0.34 - 0.73) | < 0.001 | 0.44 (0.28 - 0.69) | < 0.001 |
| University degree | 0.36 (0.23 - 0.55) | < 0.001 | 0.40 (0.23 - 0.69) | 0.001 |
| Worst life event experienced during pregnancy | ||||
| Loss of family member | 1.49 (1.26 - 1.77) | < 0.001 | 1.65 (1.36 - 2.00) | < 0.001 |
| Birth weight | ||||
| Low birth weight (< 2500 g) | 7.40 (5.92 - 9.25) | < 0.001 | 8.13 (6.34 - 10.42) | < 0.001 |
| High birth weight (> 4000 g) | 1.43 (0.71 - 2.88) | 0.30 | 1.28 (0.60 - 2.69) | 0.51 |
| Normal (2500 – 4000 g) | Ref | - | Ref | - |
| Twins or more | 2.44 (1.68 - 3.53) | < 0.001 | 0.84 (0.54 - 1.31) | 0.45 |
| Psychological symptoms during pregnancy | 2.13 (1.12 - 4.05) | 0.02 | 1.42 (0.67 - 3.00) | 0.35 |
| Diabetes during Pregnancy | 1.18 (0.82 - 1.71) | 0.35 | 1.19 (0.77 - 1.83) | 0.41 |
| Anemia during pregnancy | 0.85 (0.70 - 1.02) | 0.09 | 0.90 (0.73 - 1.12) | 0.37 |
| Dental disorders during pregnancy | 2.35 (1.86 - 2.98) | < 0.001 | 2.49 (1.90 - 3.27) | < 0.001 |
| High blood pressure during pregnancy | 2.13 (1.53 - 2.95) | < 0.001 | 1.62 (1.11 - 2.38) | 0.01 |
Crude and Adjusted Odd Ratio for Infant Mortality: Logistic Regression Model
5. Discussion
In our study, we indicated important variables that were related to infant mortality using data mining algorithms and a logistic regression model. Based on the results, Naïve Bayes among data mining algorithms had better performance in terms of precision, AUC, F1-score, and sensitivity compared to other algorithms; also, the results of logistic regression were similar to data mining algorithms. So we can say, even in studies with a large sample size, traditional models (logistic regression) are similar to modern models (data mining), which have high potency to release accurate and fit models to predict important related factors. In similar studies, the results of comparing modern and traditional modeling showed that data mining methods did not have any advantage over logistic regression for prediction. The results of logistic regression and data mining (value of AUC and Precision) were close together, but in some cases, logistic regression had a better performance (14, 15); however, some articles reported that data mining models (Naïve Bayes Network and Artificial Neural Network) were more accurate and efficient compared to logistic regression model (16, 17). In the present study, the results of data mining models showed that important factors related to infant mortality were mother’s age of pregnancy, place of living, mother’s literacy, mother’s job, consanguineous marriage, gap of pregnancy, worst life event, smoking during pregnancy, sex of child, twins, dental disorders, psychological syndrome, high blood pressure during pregnancy, gestational diabetes, and anemia during pregnancy, respectively. Therefore, infant mortality among mothers with normal age during pregnancy (18 - 35 years) was 40% lower than the mothers with age 35 years old and over. Pregnancy in < 18 years old due to biological and psychological insufficiency of mothers and chance of low birth weight and pregnancy in > 35 years due to high probability of born with cognitional disorders can increase the stillbirth and infant mortality; so normal range of mother’s age in pregnancy can be a protective factor for infant mortality (18, 19). Another important factor was consanguineous marriage; in other words, consanguineous marriage among parents increased the chance of infant mortality to 44% compared to non-consanguineous marriage. Similar studies reported that consanguineous marriage is responsible for congenital disorders and genetic diseases like Down syndrome, thalassemia, asthma, mental disorders, heart diseases, gastrointestinal disorders, and hearing deficiency that influence the health and survival of infants and children (20, 21). Gap of pregnancy was significantly associated with infant mortality so that short intervals between pregnancies (< 3 years) can increase the risk of infant mortality. In other words, inadequate maternal recovery time and its complication like anemia, adverse psychological effect of delivery, inadequate mother care for infants, cessation of breastfeeding, and spreading infectious diseases among individuals are consequences of short birth interval which affect infant mortality (22). Also, in this study, we found that first pregnancy increased the chance of infant mortality to 53% that can be due to low maternal experience in infant care. Mother education can be a protective factor for infant mortality. Because university education and high school education reduced infant mortality to 60% and 56%, respectively; education can increase connections of mothers with resources for infant health, awareness of healthy behaviors, and access to health services (23). History of the worst life events like loss of parents during pregnancy among mothers was significantly associated with infant mortality, and 65% increased the chance of infant mortality. Psychological traumatic events such as loss of parents affect physical and mental health, loneliness, and infant poor care, which all can affect infant mortality (24, 25). The results showed that mortality among infants with low birth weight (< 2500 g) was 8.13 more than the infants with normal birth weight (2500 – 4000 g); it is due to the vulnerability of infants to various diseases and death (26). Finally, a significant relation was found between a history of diseases during pregnancy like dental disorders and high blood pressure with infant mortality. As a result, infant mortality among mothers with a history of dental disorders and with high blood pressure during pregnancy were 2.49 and 1.62, respectively, more than mothers without this complication. Similar studies reported that periodontal disease and low oral health can indirectly influence low birthweight; thus, dental disorders like periodontal disease in pregnant women with reservoir of microorganisms can be a risk factor for adverse outcomes like low birth weight and, finally, neonatal and infant mortality (27, 28). Also, high blood pressure during pregnancy (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg) affects a mother’s health and her infant. High blood pressure is responsible for preeclampsia, stroke among mothers, and preterm delivery that lead to infant mortality or stillbirth (29).
Finally, variables like infant's sex, twins, smoking during pregnancy, gestational diabetes, gestational anemia, living place (urban or rural), mother's job, and psychological symptoms during pregnancy were all indicated as important factors related to infant mortality, but in the logistic regression model, a significant relation was not found considering these factors. Missing data due to incomplete checklist and response bias and underestimation due to unwillingness of participants to report factors with strong social stigma among women such as smoking were the limitation of the study.
5.1. Conclusions
Infant mortality is a multifactorial outcome, which includes infants, mothers, and events during pregnancy. Events during pregnancy such as dental disorders, high blood pressure, and loss of parents, factors related to infants such as low birth weight (< 2500 g), factors related to mothers like consanguineous marriage, and gap of pregnancy (< 3 years) were risk factors, while the age of pregnancy (18 - 35 year) and a high degree of education were protective factors. Thus due to the high accuracy and potency of modern modeling similar to traditional modeling (logistic regression models), we can use machine learning for indicating related factors to infant mortality; consequently, these factors can be prevented.