1. Background
The use of CT scans has grown rapidly worldwide in recent decades (1-7). In 2005, about 8.2 million CT scans were performed in Germany, with a child CT ratio of about 1% (8). In 2011, about 85 million CT scans were performed in the United States, of which 5 - 11% belonged to children (6, 9, 10). In 1982, the average annual dose of ionizing radiation from medical diagnostic exposures was about 0.5 mSv per person in the United States, up to 3 mSv in 2006 (11).
Benefits of CT scan are not hidden from anyone and it is a valuable tool for diagnosis of diseases. This modality, compared to MRI, requires less time to perform without the need for anesthesia (12, 13). Despite the widespread use of this modality, it is important to note that CT scan is one of the sources that provide the highest level of radiation exposure from diagnostic medical examinations (12-15). High doses of radiation may potentially increase the risk of cancer in children, as children are more sensitive to radiation because of rapid growth and high mitotic activity as well as longer life expectancy, which make children much more vulnerable to post-radiation cancers than adults (2, 15-17). In addition, a comparison of the dose received between infants and adults during CT scan of the brain with equal parameters between the two groups shows a 4-fold dose received in infants (18). This issue has become a major concern for the medical community (2, 14-16, 19). According to a US CT scan report; it is estimated that 500 cases of cancer are caused by exposure to CT in early childhood, which is responsible for an increased risk of about 0.35% (20). Predictive models have suggested that 2% of all future neoplasms in the general population in the United States could be linked to CT scans (6). Using CT in an under 15-year-old child to receive a cumulative dose of 50 mG may triple the risk of leukemia, and a dose of about 60 mG may triple the risk of brain tumors. Because these cancers are relatively rare, the full cumulative risk is small. Within 10 years of receiving the first CT scan in patients younger than 10 years, one case is estimated to be leukemia and one case to be brain tumor per 10,000 CT scans of the head (16). One case of leukemia may result from 5,250 brain CTs under five years and one from 21,160 scans in the age range between 10 - 14 (21). Cancers of the breast, thyroid, lung, and also leukemia were responsible for 68% of cancers in CT exposed girls and the cancers of the brain, lungs, colon, and also leukemia were responsible for 51% of future cancers in boys (21). Pearce et al. found a positive correlation between CT dose induced by CT and leukemia and brain tumors. The relative risk of leukemia for patients receiving a cumulative dose of at least 30 mG was 3.18 and the relative risk of brain cancer for patients receiving a cumulative dose of 50 - 74 mG was 2.82 (16). On the other hand, a high dose of radiation in the brain may influence pituitary function in the future, especially children under two years old. This issue leads to main complications such as decreased secretion of growth hormone, thyroid, and sex hormones, resulting in reduced growth, fertility problems, and even micropenis in boys (22).
2. Objectives
Based on the fact that children under 10 years of age are several times more sensitive to ionizing radiation than adults, it is very important to detect the absolute indication for this type of imaging and, if necessary, select other diagnostic modalities with no ionizing radiation.
It is estimated that up to 30% of imaging studies, including CT is questionable; it can be replaced by another modality without ionizing radiation (18). CT scans cover up to 60% of the total radiation dose, but only about 6% of radiological procedures. Due to the fact that children are more sensitive to radiation, this study was designed to determine the current status of radiation exposure from CT scans in children for intervention planning to reduce the risks of radiation in children.
3. Methods
This study is a retrospective cross-sectional descriptive survey. The inclusion criteria were all children admitted to Educational and Medical pediatric Taleghani hospital during the years 2018 to 2019 who underwent CT scan. The exclusion criteria included those with incomplete data.
Based on the study of Brady et al. (12) at a 95% confidence level and 5%accuracy at least 323 scan samples were required.
After approving this study, data of patients who underwent CT scans, according to the physician discretion were analyzed, and the checklist of variables was completed.
Required information, including demographic data, anatomical location of the scan, diagnostic findings from the CT scan report, final diagnosis, number of scans performed during hospitalization, and length of hospital stay were analyzed.
On the other hand, the total amount of radiation received by calculating the patient was estimated by the recorded amount for each patient who underwent this procedure as it was available in the Picture Archiving and Communication System (PACs) of the University of Medical Sciences. We entered the data in the checklist for each sample.
The number of scan locations were as follows: brain 155, abdominal and pelvic 36, chest 105, paranasal sinus 34, neck 9, facial 3 and limb 2. Data were entered using SPSS software version 23 and described with descriptive statistics (frequency, frequency percentage, and mean and standard deviation).
4. Results
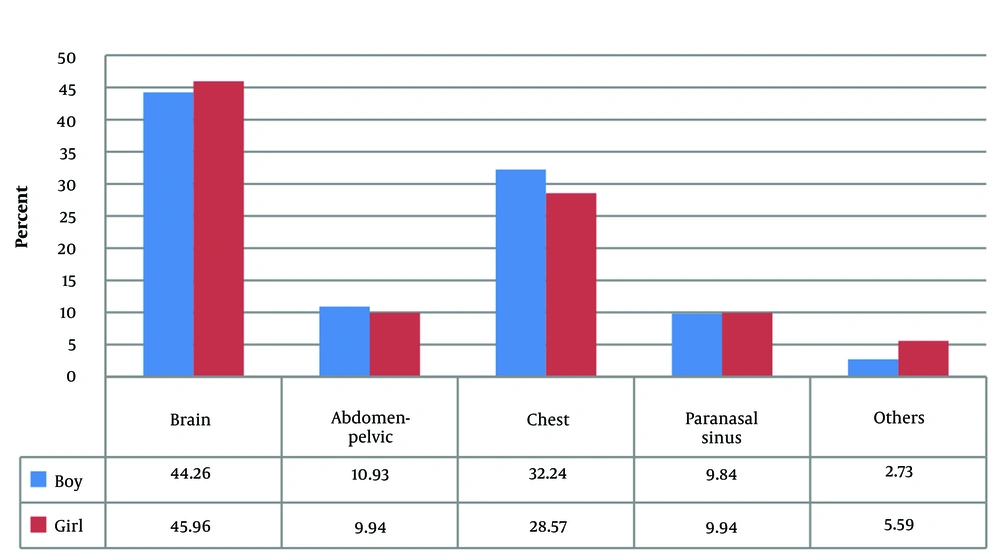
In this study, 280 cases were reviewed. Out of 280 patients, 222 patients underwent scan from one location, 55 patients from two locations, and four patients from three different anatomical locations, so 344 scans were analyzed. The cases included 146 boys (52.1%) with a mean age of 57.7 ± 55.8 months and 134 girls (47.9%) with a mean age of 54.7 ± 48.6 months. The number (%) of patients in under six months was 26 (9.4), 6 - 12 months was 36 (12.9), 1 - 5 years was 108 (38.5), 5 - 10 years was 62 (22.1) and 10 - 18 years was 48 (17.1). Anatomical location of CT scan requested by sex is shown in Figure 1.
In 344 scans that were performed from a total of 280 patients, brain with 155 scans (43.6%) and chest with 105 scans (30.52%) underwent the highest number of scans, respectively. CT scans were performed on 26 cases (9.4%) under six months, of which 14 cases belonged to the brain, 9 cases to the chest, 2 cases to the abdominal and pelvic areas, and one case concerned facial bones. Anatomical location of CT scan requested by age is shown in Table 1.
| Age (y) | Anatomical Location, Frequency (%) | Total, Frequency (%) | ||||
|---|---|---|---|---|---|---|
| Brain | Abdomen Pelvic | Chest | Paranasal Sinus | Others | ||
| 0 - 1 | 35 (22.6) | 6 (16.7) | 24 (22.9) | 0 (0) | 3 (21.4) | 68 (19.8) |
| 1 - 3 | 41 (26.4) | 8 (22.2) | 29 (27.6) | 4 (11.8) | 5 (35.8) | 87 (25.3) |
| 3 - 5 | 28 (18.1) | 3 (8.3) | 8 (7.6) | 2 (5.8) | 1 (7.1) | 42 (12.2) |
| 5 - 8 | 13 (8.4) | 4 (11.1) | 15 (14.3) | 10 (29.4) | 2 (14.3) | 44 (12.8) |
| 8 - 10 | 22 (14.2) | 9 (25) | 16 (15.2) | 10 (29.4) | 1 (7.1) | 58 (16.9) |
| ≥ 10 | 16 (10.3) | 6 (16.7) | 13 (12.4) | 8 (23.6) | 2 (14.3) | 45 (13) |
| Total | 155 (100) | 36 (100) | 105 (100) | 34 (100) | 14 (100) | 344 (100) |
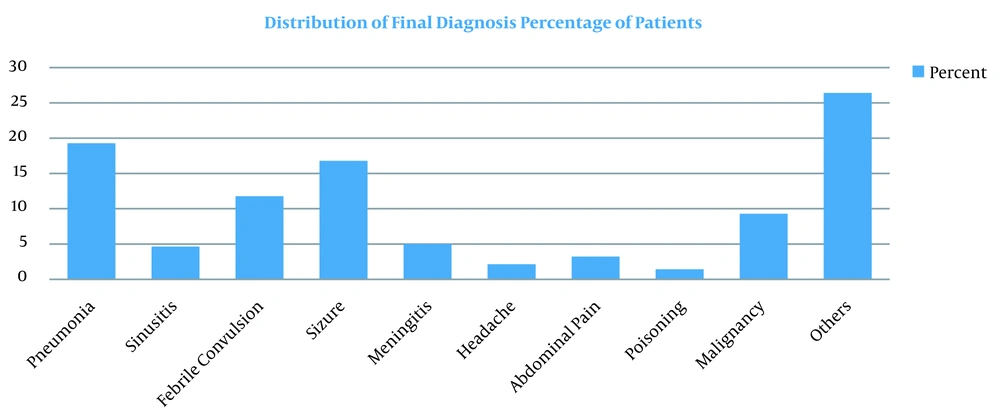
Fever and seizures with 41 cases (14.64%), cough with 36 cases (12.85%), and seizures with 33 cases (11.78%) were the most common primary complaints. Pneumonia was the most common final clinical diagnosis among patients (19%) followed by convulsions (17%) and febrile seizure (12%), respectively (Figure 2). The duration of hospitalization in this study was from one to 31 days with an average of 6.13 days among which 24 patients (8.57%) were hospitalized for one day, 77 patients (27.5%) for two or three days. Out of 155 brain CT scans reviewed, 115 scans (74.19%) were normal and without significant findings.
Abnormality in ventricles and cerebral cisterns (14%) was the most common finding in brain CT scan. Abnormality in lung tissue ventilation (66.8%) was the most common finding in chest scans. The presence of Paraaortic lymphadenopathy was the most common finding (33.4%) in abdomen-pelvic scans (Table 2). Brain scans with mean radiation of 358.66 mGy.cm, as well as a maximum radiation of 995.30 mGy.cm, had the highest amount of absorption radiation in the patients in this study. Paranasal sinus, neck, chest, and abdominopelvic CT scans had 70 ± 51.76, 73.67 ± 29.73, 45.78 ± 31.93, 120.25 ± 84.35 mGy.cm, respectively (Table 3).
| Anatomical Locations of CT Scans and Description of Observations | Normal, Frequency (%) | Abnormal, Frequency (%) |
|---|---|---|
| Brain (N = 155) | ||
| Spatial lesion in the supratentorial and infratentorial areas | 98 (152) | 3 (2) |
| Ventricles and cisterns | 133 (85.8) | 22 (14.2) |
| Brain tissue density | 141 (91) | 14 (9) |
| Calvary view | 152 (98) | 3 (2) |
| Other findings | 145 (93,5) | 10 (6.5) |
| Paranasal sinus (N = 34) | ||
| Clear paranasal sinuses | 5 (14.7) | 29 (85.3) |
| Spatial lesion in the nasal cavity and osteomeatal complex | 33 (97) | 1 (3) |
| Nasal septum in the midline | 28 (82.3) | 6 (17.7) |
| Pathology in the bones | 32 (94.1) | 2 (5.9) |
| Chest (N = 105) | ||
| Ventilation of lung tissue | 36 (34.2) | 69 (66.8) |
| The trachea and main bronchi | 99 (94.2) | 6 (5.8) |
| Consolidation in the lung tissue | 68 (64.7) | 37 (35.3) |
| Nodule or pulmonary mass | 93 (88.5) | 12 (11.5) |
| Pleural thickness | 102 (97.1) | 3 (2.9) |
| Pleural effusion | 97 (92.3) | 8 (7.7) |
| Pathological mediastinal lymphadenopathy | 79 (75.2) | 28 (24.8) |
| Heart size | 102 (97.1) | 3 (2.9) |
| Thoracic skeleton | 104 (99) | 1 (1) |
| Mosaic Attenuation | 80 (76.1) | 25 (23.9) |
| Ground Glass Opacification | 75 (54.2) | 30 (45.8) |
| Air Broncogram | 98 (93.3) | 16 (6.7) |
| Peribronchial Cuffing | 90 (85.7) | 25 (14.3) |
| Atelectasis | 85 (80.9) | 20 (19.1) |
| Others | 94 (89.5) | 11 (10.5) |
| Abdomen-pelvic (N = 36) | ||
| Liver size | 29 (80.5) | 7 (19.5) |
| Liver density | 31 (13.9) | 5 (13.9) |
| Spatial lesion in the liver | 32 (88.8) | 4 (11.2) |
| Spleen Size | 35 (97.2) | 1 (2.8) |
| Spatial lesion in the spleen | 35 (97.2) | 1 (2.8) |
| Paraaortic and hepatic lymphadenopathy | 24 (66.6) | 12 (33.4) |
| Dilatation of the intestines | 35 (97.2) | 1 (2.8) |
| The thickness of the intestinal wall | 35 (97.2) | 1 (2.8) |
| Kidneys sizes | 35 (97.2) | 1 (2.8) |
| Bladder wall thickness | 35 (97.2) | 1 (2.8) |
| Stone or mass in the bladder | 36 (100) | 0 (0) |
| Free fluid in the abdominal cavity | 30 (83.3) | 6 (16.7) |
| Lesion in bone tissue | 36 (100) | 0 (0) |
| Intraperitoneal lymphadenopathy | 33 (91.6) | 3 (8.4) |
| Other findings | 18 (50) | 18 (50) |
| Anatomical Location of the Scan | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| Brain | 358.66 ± 166.81 | 131.24 | 995.3 |
| Paranasal sinuses | 70 ± 51.76 | 28.54 | 207.36 |
| Neck | 73.67 ± 29.73 | 27.95 | 111.2 |
| Chest | 45.78 ± 31.93 | 12.64 | 164.82 |
| Abdomen-pelvic | 120.25 ± 84.35 | 19.22 | 355.2 |
| More than one region | 217.4 ± 151.31 | 63.24 | 605.73 |
5. Discussion
In this study, we analyzed the CT scans requested in pediatrics hospital. According to our data, brain (43.6%) and chest (30.52%) scans were on the top list of requested CT scans, respectively. In addition, the ratio of under 5-year-old children who underwent CT scans in both sexes was considerable. On the other hand, there was no evidence of a pathologic report in 74.19% and 33.2% of brain and chest scans, respectively.
In comparison to other studies, if we added paranasal sinus scans, the ratio of head and neck scans would be 54.9%; whereas, in other studies, it was 60.1 to 83.64% (23-25). It should be noted we did not include the brain CT scans requested for head trauma, because our hospital did not admit traumatic patients, otherwise this survey showed a higher frequency of brain CT scans than that was mentioned in our study. It is recommended that the reasons for any requested CT scans should be completely clarified and if a safer modality exists, it should be replaced.
As mentioned above, in this survey 19.8 % of children exposed to the radiation were in infancy period and 57.3% were under five years old. In the survey in Catalonia, 26% of pediatric CT scans were performed in fewer than 5-year old children (13). Although we could not compare our data with this EPI study, our data demonstrated that the ratio of requested CT in infancy and early childhood is considerable. We must do some immediate intervention for reducing these numbers by implementing some protocols and rules.
Top of the final diagnosis in this survey was convulsion that included febrile convulsion (29%). No evidence of pathology was reported in 74.19% of brain CT scans. As our data showed, in the study of Fallah et al., 74% of normal results were reported in patients who presented due to seizures (26), but in a study conducted in Tehran in 2013, the rate of abnormal findings of CT scans was 14.3%, which was higher than our survey (27). Brain scans with mean radiation of 358.66 mGy.cm and also a maximum radiation of 995.30 mGy.cm had the highest amount of absorption radiation in the patients in this study. Since solid cancer risk for brain CT scans of children under five years was 1.1 - 2.4 cancers per 10,000 CT and the relative risk of leukemia for brain CT scans was the highest in children under 10 years of age, more attention is needed to request CT, especially for infants and younger children and protocols should be written for protection of our patient from hazardous radians.
In this survey, the frequency of abnormal findings in abdominal and pelvic scan was 10.46%, whereas it was 7.32 to 19.9% (24, 25) in other studies. One of the most reasons for requesting abdominopelvic CT scan is for appendicitis. Although CT-scan is the gold standard for diagnosing appendicitis, early exposure to radiation is a concern of this technique. CT scans have certainly saved a significant number of children from an unnecessary appendectomy, but have caused unnecessary exposure to radiation (28). The risk of solid cancers is higher for abdominal and pelvic scans is 25.8 - 33.9 cases per 10,000 CT scans which is higher in girls compared to 13.1 - 14.8 cases per 10,000 scans of boys. Solid cancers due to radiation are seen for every 300-390 CTs of the abdomen and pelvis in girls and every 670 - 760 CTs in boys (21). Another study showed that about 29,000 future cancers might be related to CT in 2007, with the largest share belonging to in the abdomen and pelvis CTs (10). As our data demonstrated, more than 89% of abdominal and pelvic scan had normal reports. According to the results mentioned, we should reevaluate the indication of abdominal CT in our hospital and use substitute diagnostic modalities to save our patient from unnecessary radiations.
However, for each child alone, the health risk of a CT scan may seem small and the individual benefits should outweigh the risks for the procedure to perform due to the fact that the dose of radiation from CT scans is relatively higher compared to most conventional X-rays (13) and the resulting risk of developing cancer due to this modality requires care and attention. It is important that pediatric CT scans are properly requested and the doses received are carefully monitored (13). CT scans should be limited to situations where there is a clear clinical indication, and any CT scan should include minimal use of radiation (19). A 25% reduction in the maximum radiation between the age group and the location of the medium dose can prevent 43% of cancers compared to a 33% reduction in future cancers if one-third is reduced. The combination of these two strategies can prevent 62% of these cancers (21). Most radiologists are now aware of the dangers, and with the use of advances in technology can reduce the dose of CT scans over the past decade (19). Applying available radiation dose reduction strategies in combination with limiting unnecessary imaging can dramatically reduce CT radiation-induced cancer in children. It is recommended that physicians consider that overuse of these modalities not only increases the treatment cost but also is unethical. Because of the side effects of these modalities, the best way to prevent misuse or overuse in the patients as is also true for inappropriate use of antibiotics, is to use guidelines and review the indications for using CT scans as a diagnostic modality (29) and also to evaluate the risks versus the benefits for each patient.
This study can be considered a baseline study to review the current situation in the frequency of CT scans performed in children and may help in the planning for more rational use of CT scans to improve the health of children.
5.1. Limitation
Since the present study was a cross-sectional and retrospective descriptive study, the main limitation of the file registration problems was that some files were distorted, or inaccessible, as well as some files were incomplete and so on, which led to the loss of part of the data during the study. On the other hand, the number of previous CT scans for each patient before admission was not available in the file.
5.2. Conclusions
The findings of the present study showed that the rate of normal CT scans performed was relatively high and the range of rays available for each modality was significantly wide. The ratio of infancy and early childhood CT scans is considerable. More studies should be done to clarify the situation and effective interventions must be made in this regard.