1. Introduction
Chronic abdominal pain is a medical condition that persists for more than two to three months. It is thought to be the cause of 2 - 4% of pediatric ward admissions (1). Chronic abdominal pain in pediatric patients is mostly functional, but in the presence of alarm symptoms (e.g., involuntary weight loss, deceleration of linear growth, gastrointestinal blood loss, significant vomiting, chronic diarrhea, and persistent upper or lower right quadrant pain) organic etiologies should be considered (2).
Reaching a diagnosis concerning the organic causes of chronic abdominal pain not only requires paraclinical investigations, but also it appears that sometimes a high index of suspicion is required. Concerning the higher prevalence of organic etiologies of chronic abdominal pain in patients admitted to pediatric gastroenterology wards in comparison with the general population (3), it is necessary to seek for diagnostic procedures to help us find the underlying causes of the pain with lower expenses and in a shorter time (4). Accordingly, when the routine laboratory and radiologic tests are inconclusive, gallbladder (GB) dysmotility could be considered as a diagnosis of exclusion, although it is a very rare cause of persistent abdominal pain in children (5). One of the diagnostic tests that can help practitioners to reach a diagnosis in patients suffering from hepatobiliary tract disorders is hepatobiliary scintigraphy (6). Previous studies approved the efficacy of hepatobiliary scintigraphy in the management of chronic abdominal pain in children (7, 8). Moreover, to the best of our knowledge, no studies have been conducted in the developing countries to assess the effectiveness of hepatobiliary scintigraphy in the diagnosis of the etiology of chronic abdominal pain in children.
In this study, we report a series of pediatric patients visiting Mofid Children’s Hospital affiliated to Shahid Beheshti University of Medical Sciences due to chronic refractory abdominal pain and nonspecific gastrointestinal symptoms. After thorough medical and psychological examinations, hepatobiliary scintigraphy after fatty meal ingestion using positive 99mtechnetium (Tc)- labelled bile salts revealed GB dysmotility.
2. Case Presentation
2.1. Case 1
A 16-year-old boy presented to the hospital with the chief complaint of persistent supraumbilical abdominal pain started five months prior to his admission. The pain was worsened by eating and was associated with headache, nausea, and vomiting. Physical examinations were unremarkable. Endoscopic and histopathologic evaluations demonstrated esophagitis, antral gastritis, and a small hiatal hernia. High-dose oral proton pump inhibitor (PPI) trial decreased his symptoms, but after tapering the medication, his symptoms aggravated. Radiological studies (including spiral abdominal CT scan, abdominal and pelvis ultrasonography, and barium upper gastrointestinal [GI] series) and laboratory investigations were unremarkable, except for the total bilirubin of 2.8 and a direct bilirubin of 0.5, suggesting Gilbert's syndrome (Table 1).
| Amylase (IU/L) | Lipase (IU/L) | AST (IU/L) | ALT (IU/L) | ALKP (IU/L) | Bili total (mg/dL) | Bili direct (mg/dL) | Anti-tTG | EMA | Helicobacter pylori Ag | IgA Serum | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 46 | 18 | 28 | 39 | 178 | 2.8 | 0.48 | negative | negative | negative | normal |
| Case 2 | 63 | 24 | 35 | 41 | 189 | 0.65 | 0.16 | negative | negative | negative | normal |
| Case 3 | 58 | 20 | 52 | 52 | 210 | 0.73 | 0.21 | negative | negative | negative | normal |
| Case 4 | 49 | 22 | 21 | 12 | 276 | 0.30 | 0.13 | negative | negative | negative | normal |
Other Laboratory Tests
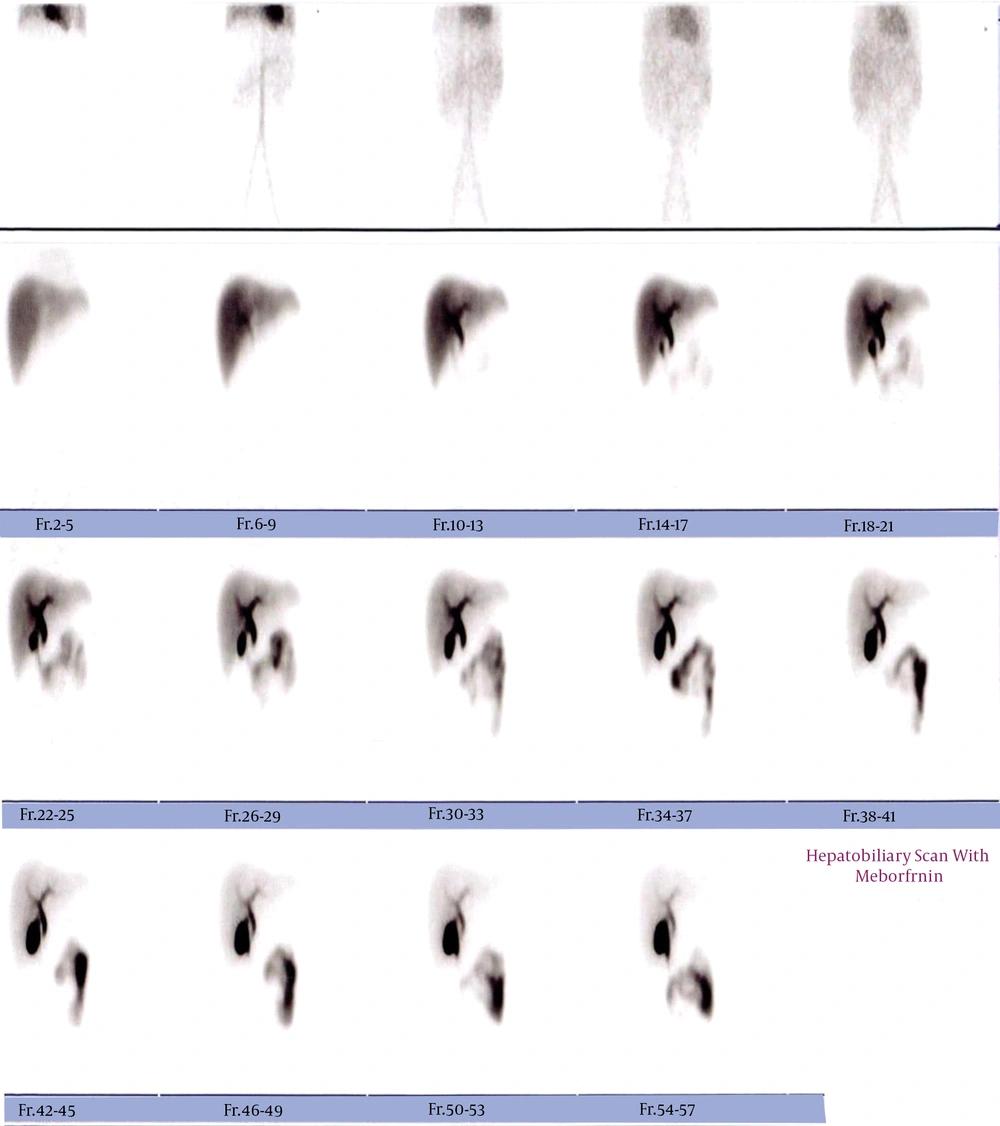
Neurological evaluations and psychiatric consultation were done to assess the patient’s mental status and recognize the potential sources of stress, and evaluate the patient for the diagnosis of functional abdominal pain syndromes. To detect biliary tract abnormalities, hepatobiliary scintigraphy was requested. Hepatobiliary scintigraphy reported a gallbladder ejection fraction (GBEF) of 15% with acceptable hepatocellular function, indicating gallbladder dyskinesia (GBD, Figure 1). Laparoscopic cholecystectomy was conducted, and his pain was completely resolved after the surgery. In one-year follow-up, he was symptom-free.
Hepatobiliary scintigraphy 30 minutes after fatty meal ingestion of Case 1. Gallbladder appeared 10 minutes of study and about 30 minutes after the ingestion, significant retention of tracer in gallbladder is still noticed (EF = 15%). Four hours later, activity retention in the gallbladder is still perceived.
2.2. Case 2
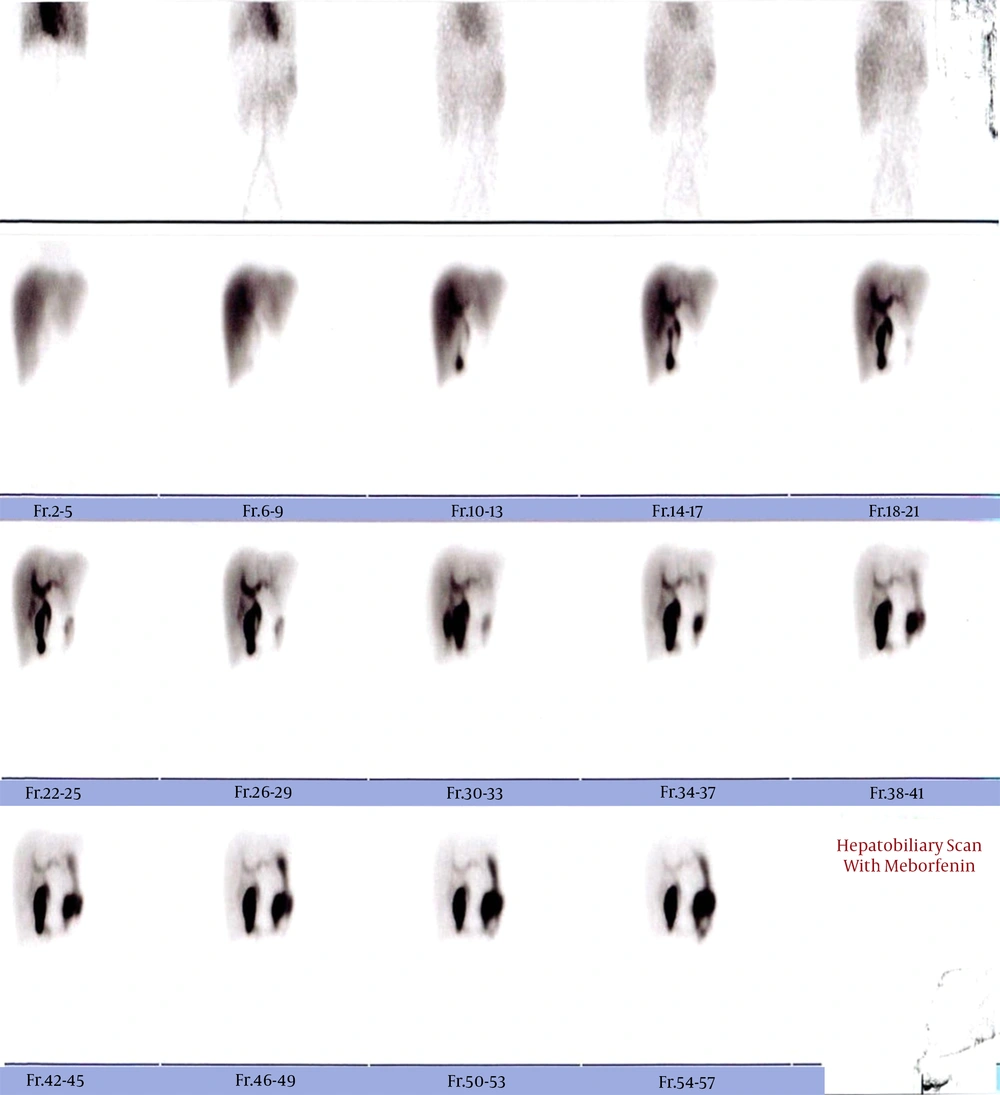
A 12-year-old girl was referred to our hospital because of nausea, vomiting, and oral food intolerance, which had been suddenly started two months before. She experienced a 10-kg weight loss along with abdominal pain, anorexia, and headache. Three months before, during her previous hospitalization with a similar complaint, endoscopy, and histopathological evaluations had demonstrated sliding hiatal hernia along with class A esophagitis and active chronic gastritis with the presence of Helicobacter pylori. This time, due to unresolved symptoms after proper treatments, the patient was hospitalized for further evaluations. Her paraclinical studies were unremarkable (Table 1). Re-endoscopy showed non-significant mucosal erythema in the gastric body with negative rapid urease test for Helicobacter pylori. Just like the first case, to identify other probable underlying etiologies present with biliary symptoms, she underwent hepatobiliary scintigraphy and marked biliary duodeno-gastric reflux and noticeable gallbladder distension with an elongated shape GB suggested GBD (Figure 2). Moreover, the patient could not tolerate fatty meals. Laparoscopic cholecystectomy was performed to excise the gallbladder, and the patient was discharged with dissolved symptoms and no surgical complications.
2.3. Case 3
A 14-year-old girl who was suffering from intermittent abdominal pain radiating to her back and epigastria, which had started six months before and worsened from two months before was admitted to the hospital. The pain was localized in the upper right quadrant (RUQ), worsened by eating, and improved with leaning forward. The pain was associated with nausea and vomiting following oral food consumption. Physical examinations were unremarkable. Abdominal CT scan and hepatobiliary ultrasonography showed no abnormalities. Psychiatric consultation was done to recognize any potential sources of stress. After two months of receiving treatment for IBS, her symptoms did not subside. Laboratory, endoscopic, and histopathological evaluation of the upper gastrointestinal (GI) tract and the upper GI series were unremarkable (Table 1). Similar to the previous cases, hepatobiliary scintigraphy was requested to determine if any biliary tract abnormality is responsible for the patient’s biliary-like pain. Severe stenosis of the common bile duct and/or Oddi sphincter dysfunction was reported in scintigraphy. She underwent laparotomy, and intraoperative cholangiography demonstrated enlarged gallbladder with the severe stenosis of cystic duct at the junction of the cystic duct with the common bile duct. Laparoscopic cholecystectomy was performed. The patient was discharged with resolved symptoms.
2.4. Case 4
The fourth patient was a 6-year-old boy who was admitted because of a three-year history of nausea, vomiting, anorexia, early satiety, and abdominal pain, especially in the periumbilical and epigastric regions, which had worsened from five months before. The pain was exacerbated after meals and relived with fasting. Physical examinations were unremarkable. Abdominal ultrasonography showed biliary sludge with normal GB wall thickness. Liver, pancreas, spleen, and both kidneys were normal. Also, paraclinical investigations were unremarkable (Table 1). The patient was treated for functional abdominal pain and IBS with famotidine for eight weeks without any significant responses. He underwent diagnostic upper gastrointestinal (UGI) endoscopy and colonoscopy. These endoscopic and histopathological investigations were unremarkable. Hepatobiliary scintigraphy revealed acceptable hepatocellular function with the retention of tracer in the gall bladder (GB) and an obvious delay in excretion. GBEF 30 min after fatty meal was about 22%. He underwent laparoscopic cholecystectomy and was symptom-free at discharge.
2.5. Follow up
All the patients were followed up until one year after cholecystectomy. During their follow-ups, all the patients were symptom-free. They are doing well without any postoperative complications. No episode of prolonged abdominal pain or prolonged vomiting was reported in this 12-month period.
3. Discussion
Finding what is causing chronic abdominal pain in pediatric patients with alarm symptoms may be challenging, both for patients and pediatricians. Proper diagnostic studies should be implemented to reach an accurate diagnosis in shorter periods. It is important to consider hepatobiliary tract disorders as a probable cause of abdominal pain in pediatric patients. Hepatobiliary scintigraphy could help in detecting the abnormalities of the biliary system. There are some occasions where organic etiologies of chronic abdominal pain could not be distinguished from functional etiologies. This may often occur in children, especially those with lower ages that are not able to properly localize pain; thus, the diagnosis of such dysfunctions may be more difficult and lead to longer periods of work-up and delayed diagnosis (9). Additionally, studies suggest that some abnormalities that are being diagnosed and assumed to trigger the symptoms may not be the main reason behind the presented symptoms (4); therefore, proper evaluations to find the underlying cause(s) of the pain are essential.
In this case presentation, all of the evaluated patients were suffering from diseases which could cause symptoms similar to each other, including gastritis, GB dysmotility, and functional abdominal pain syndrome. Although appropriate diagnostic procedures and therapeutic approaches to diagnose and treat the patients’ symptoms were implemented, they did not subside. Concerning the nature of the symptoms which could be caused by biliary tract issues, such as biliary pain and vomiting triggered by eating, to evaluate the functional and anatomical status of the biliary tract and motility of gallbladder in patients with intermittent abdominal pain, hepatic iminodiacetic acid (HIDA) scintigraphy with fatty meal consumption using positive 99mtechnetium (Tc)-labeled bile salts was considered and demonstrated to be of great value for the diagnosis of GBD and other abnormalities of the biliary tree.
Previous studies approved hepatobiliary scintigraphy to be a standard way to detect GBD in pediatric patients with biliary pain, which was compatible with the results of the current case series (10-12). Gallbladder dyskinesia is diagnosed by GBEF lower than 35% (13), after CCK provocation or eating a fatty meal; moreover, the appropriate criteria for implementing hepatobiliary scan suggest using it for functional biliary pain syndrome in pediatric patients, chronic upper abdominal pain, and functional biliary pain caused by chronic acalculous biliary disease (6, 14). However, one study considered hepatobiliary scan as a test with poor diagnostic value in pediatric patients suspected of biliary dyskinesia (10). Unfortunately, the reliability and validity of these biliary functional surveys in pediatric patients have not been evaluated, and future studies should aim to fill the gap and recommend a standard method to perform HIDA scan since studies implement a variety of techniques regarding the dose of labeled bile salt, time of imaging, use of CCK, fatty meal or egg yolk for provocation (15).
Gallbladder dyskinesia is a motility dysfunction of the gallbladder, which is either caused by gallbladder wall dysmotility or sphincter dyskinesia (4). As a result, gallbladder cannot properly release its contents. The pain caused by this disorder is thought to be related to abnormal gallbladder wall stretch (16) and its distension and inflammation that can trigger mechanoreceptors of gallbladder wall, leading to afferent neural stimulation (17, 18). Due to a pathophysiology similar to cholecystitis and evidence supporting gallbladder dysmotility to be able to lead to chronic cholecystitis, the pain imitates biliary colic pain caused by gallstones (16).
Gallbladder dyskinesia is an uncommon disorder with symptoms that can be seen in a variety of diseases. According to Rome IV criteria for functional gallbladder disorders, it is diagnosed by typical biliary pain in the absence of gallstones, sludge, or any structural disorders (19). The biliary pain is characterized by intermittent postprandial RUQ and/or epigastric pain which gradually increases and lasts for 30 minutes or higher, and it is not postural, related to bowel movements, or gastric acid secretion. This pain can be severe enough to interfere with the patient’s daily activities (13). The most prominent symptoms of the patients diagnosed with GBD in the current study were abdominal pain and vomiting. This was compatible with previous studies, which reported the most common symptoms in children suffering from GBD to be abdominal pain (upper right quadrant/epigastric), fatty food intolerance, nausea, and vomiting (20, 21).
Laparoscopic cholecystectomy has been the standard treatment for GBD in recent years; however, not all patients benefit from cholecystectomy. Previous studies have reported a wide range of satisfaction rate from 34% to 100% in patients undergone this surgery (9, 15). With regards to the prediction of pain improvement in patients undergoing surgery, there is evidence suggesting that the symptoms and duration of them can predict cholecystectomy outcomes in patients. However, findings of previous studies concerning the predictive value of hepatobiliary scintigraphy results, including gallbladder EF rate, are inconsistent (15, 22). Future studies should address if symptoms and the duration of them can prevent unnecessary surgical operations in patients that do not benefit from cholecystectomy. Here, we followed patients until one year after cholecystectomy. Case 1 complained of transient vomiting about two months after cholecystectomy, which in further follow-ups this complaint was not repeated. Other cases were good and without the previous symptoms.
Data regarding the role of hepatobiliary scintigraphy in the management of chronic abdominal pain in children is limited. To the best of our knowledge, this is the first study that reports the efficacy of hepatobiliary scintigraphy in the diagnosis of chronic abdominal pain in children in a developing country and the first study that reports cases of gallbladder dyskinesia in Iran. Moreover, the use of CARE checklist to improve the quality of our work in case of completeness and transparency can be considered as another strength of our study. On the other hand, the limited number of reported cases in this study hinders us from drawing a definitive conclusion, which can be assumed as a limitation of our study.
In conclusion, hepatobiliary scintigraphy, as a method to investigate hepatobiliary system, can be of a great value to save time and help pediatricians to detect biliary tract disorders, and this diagnostic study can be suggested in the management of chronic abdominal pain and significant vomiting in pediatric patients. Moreover, GBD, which is a rare but well-studied condition in adult patients, should be considered in pediatric patients since it can present with chronic intermittent abdominal pain in association with nausea and vomiting.