1. Background
Bronchiolitis is a viral infection that causes the airways (bronchioles) in the lungs to become narrow, which makes breathing difficult. It occurs most often in children under two years of age during winter and early spring. Very rarely, adults can also get bronchiolitis (1). In fact, it is the most common infection of the lower respiratory tract in infants and the main reason for admission from birth to 14 months of life (2). It is also one of the most important causes of mortality and morbidity in developing countries (3). This disease is the most common infection in the lower airways during the first year of life, and approximately one percent of children are hospitalized annually (4). The disease is self-limiting and is mainly associated with respiratory syncytial virus (RSV), and bronchial obstruction is associated with edema and accumulation of mucus (5). Generally, bronchiolitis is established by a syncytial pattern (6). The prevalence is 2:1 in males (7), and the highest incidence is in winter and more by RSV, although other viruses are also involved., although other viruses are also involved (6). Bronchiolitis is commonly defined as the first viral respiratory distress attack with symptoms of coryza, coughing, crackle, and wheezing, but its clinical definition varies from country to country (8, 9). The American Academy of Pediatrics (AAP) has defined bronchiolitis as a set of clinical signs and symptoms, including early symptoms of respiratory infections and wheezing in children younger than two years of age (8). However, in the UK and some parts of Europe and Australia, wheezing is not a mandatory criterion for diagnosis (8, 9). Usually, the first sign of the disease in infants is rhinorrhea. Coughing can occur simultaneously, but it usually occurs after one to three days, which can be accompanied by mild cough and sneezing at this time. Immediately after coughing, a child with bronchiolitis will have audible wheezing. If the disease is mild, the symptoms do not progress more than this stage. Auscultation often represents mild and diffused dry crackles with exhalation wheezing (10). In about half of the cases, the disease continues with a recurrent wheezing after bronchiolitis, which is referred to as wheezing after bronchiolitis. Some studies investigated the association of this wheezing with asthma, which indicated the potential role of inflammatory and interleukin processes in the onset of the disease and its related symptoms (5, 10-12). Sustained wheezing that develops after bronchiolitis as a respiratory tract disease is one of the causes of morbidity in children, besides being costly for the health system (13, 14).
According to recent studies, antioxidants (such as vitamins A, E, and C, and carotenoids) have a unique effect on the immune system (15). Vitamin A has important roles such as regulating the functions of immunity, vision, reproduction, and cellular communication. Moreover, different studies have shown its role in the health of children under the age of five, so that even a mild deficiency of this vitamin leads to increased mortality in children aged six months to six years (16-20). Regarding the proven role of vitamin A in regulating immune function, (21) some studies have examined the relationship between this vitamin and infant bronchiolitis.
Considering the relationship between bronchiolitis and wheezing and asthma in infants (11) and due to the limited studies on the efficacy of administrating vitamin A for patients with bronchiolitis, this study was carried out to determine the effect of vitamin A on persistent wheezing in infants with bronchiolitis referred to Ali Ibn Abi Talib Hospital in southern Iran in 2018.
2. Objectives
The present study aimed to determine the effect of vitamin A on persistent wheezing in infants with bronchiolitis referred to Ali Ibn Abi Taleb Hospital in Zahedan, Iran.
3. Methods
This clinical trial was conducted on infants (age range: one month to two years of age) diagnosed with bronchiolitis after taking a history and performing a physical examination. The exclusion criteria were a history of congenital heart disease, pulmonary disease, asthma, immune deficiency, and other chronic underlying diseases. Patients were also excluded from the study if another diagnosis was made during the diagnostic or treatment process.
The patients were randomly divided into two groups of case and control. The patients’ checklists were completed considering their demographic information (such as age and sex) and severity of symptoms (wheezing severity, retraction status, respiratory rate, and general condition of the patient). Both groups received the usual treatments for bronchiolitis, including nebulizer and bronchodilator. However, the case group also received 5,000 units per kilogram of body weight of the injected vitamin A. The patients in both groups were visited every 24-hours during the hospitalization, at the time of discharge, and two weeks later, and the relevant information was recorded. The collected data was entered into the SPSS software version 24 and analyzed.
4. Results
In this study, 60 infants (25 (41.7%) males vs. 35 (58.3%) females) with a mean age of 7.63 ± 4.08 months were randomly divided into two equal groups (n = 30) of case and control.
As Table 1 demonstrates, the mean age of infants did not show a statistically significant difference between the two groups (P > 0.05).
| Group | Number | Mean | SD | P Value |
|---|---|---|---|---|
| Case | 30 | 6.69 | 4.09 | 0.058 |
| Control | 30 | 8.57 | 3.91 |
As shown in Table 2, the prevalence of gender did not show a statistically significant difference between the two groups (P > 0.05).
| Sex | Group | All | P Value | |
|---|---|---|---|---|
| Case | Control | |||
| Male, No. (%) | 10 (33.3) | 15 (50) | 25 (41.7) | 0.19 |
| Female, No. (%) | 20 (66.7) | 15 (50) | 35 (58.3) | |
| All, No. (%) | 30 (100) | 30 (100) | 60 (100) | |
First: Determination and comparison of the severity of wheezing in infants with bronchiolitis at pre-treatment, 24 hours after treatment, during discharge, and two weeks after treatment in the two groups.As shown in Table 3, the severity of wheezing in infants before treatment and 24 hours after treatment did not show a statistically significant difference (P > 0.05). While 6.7% of infants in the control group had severe wheezing during discharge, no wheezing was reported in the case group. Also, the frequency of the moderate wheezing in the control and case groups was 40% and 10%, respectively (P = 0.006). Also, two weeks after the treatment, the frequency of wheezing in control group was 30%, but no wheezing was reported in case group, indicating a statistically significant difference (P < 0.001).
| Time/ Wheezing | Case | Control | All | P Value |
|---|---|---|---|---|
| Before treatment, No. (%) | 0.4281 | |||
| No | 10 (33.3) | 5 (16.7) | 15 (25) | |
| Mild | 10 (33.3) | 10 (33.3) | 20 (33.3) | |
| Moderate | 4 (13.3) | 7 (23.3) | 11 (18.3) | |
| Severe | 6 (20) | 8 (26.7) | 14 (23.3) | |
| 24 hours after treatment, No. (%) | 0.1521 | |||
| No | 12 (40) | 5 (16.7) | 17 (28.3) | |
| Mild | 9 (30) | 10 (33.3) | 19 (31.7) | |
| Moderate | 6 (20) | 7 (23.3) | 13 (21.7) | |
| Severe | 3 (10) | 8 (26.7) | 11 (18.3) | |
| During discharged, No. (%) | 0.0062 | |||
| No | 15 (50) | 5 (16.7) | 20 (33.3) | |
| Mild | 12 (40) | 11 (36.7) | 23 (38.3) | |
| Moderate | 3 (10) | 12 (40) | 15 (25) | |
| Severe | 0 (0) | 2 (6.7) | 2 (3.3) | |
| 2 weeks after treatment, No. (%) | 0.0012 | |||
| No | 27 (90) | 9 (30) | 36 (60) | |
| Mild | 3 (10) | 12 (40) | 15 (25) | |
| Moderate | 0 (0) | 9 (30) | 9 (15) |
a1, Pearson chi-square test; 2, Fisher’s exact test.
Second: Determination and comparison of the status of retraction in infants with bronchiolitis at pre-treatment, 24 hours after treatment, during discharge, and two weeks after treatment in the two groups.
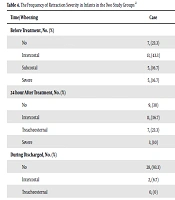
As shown in Table 4, the frequency of retraction severity in infants did not show a statistically significant difference between the two groups (P > 0.05).
| Time/ Wheezing | Case | Control | All | P Value |
|---|---|---|---|---|
| Before treatment, No. (%) | 0.1741 | |||
| No | 7 (23.3) | 13 (43.3) | 20 (33.3) | |
| Intercostal | 13 (43.3) | 13 (43.3) | 26 (43.3) | |
| Subcostal | 5 (16.7) | 1 (3.3) | 6 (10) | |
| Severe | 5 (16.7) | 3 (10) | 8 (13.3) | |
| 24 hour after treatment, No. (%) | 0.0541 | |||
| No | 9 (30) | 13 (43.3) | 22 (36.7) | |
| Intercostal | 11 (36.7) | 3 (10) | 14 (23.3) | |
| Treacheosternal | 7 (23.3) | 6 (20) | 13 (21.7) | |
| Severe | 3 (10) | 8 (26.7) | 11 (18.3) | |
| During discharged, No. (%) | 0.2732 | |||
| No | 28 (93.3) | 24 (80) | 52 (86.7) | |
| Intercostal | 2 (6.7) | 5 (16.7) | 7 (11.7) | |
| Treacheosternal | 0 (0) | 1 (3.3) | 1 (1.7) | |
| 2 week after treatment, No. (%) | 0.3552 | |||
| No | 30 (100) | 28 (93.3) | 58 (96.7) | |
| Intercostal | 0 (0) | 1 (3.3) | 1 (1.7) | |
| Treacheosternal | 0 (0) | 1 (3.3) | 1 (1.7) |
a1, Pearson chi-square test; 2, Fisher’s exact test.
Third aim: Determination and comparison of respiratory rate in infants with bronchiolitis at pre-treatment, 24 hours after treatment, during discharge, and two weeks after treatment in the two groups.As shown in the Table 5, the respiratory rate decreased significantly in both groups, and this difference existed until the end of the follow-up of patients due to the difference in baseline characteristics.
| Time | Number | Mean | SD | P Value |
|---|---|---|---|---|
| Before treatment | 0.0091 | |||
| Case | 30 | 46.86 | 9.86 | |
| Control | 30 | 53.03 | 7.77 | |
| 24 hours after treatment | 0.0011 | |||
| Case | 30 | 45.63 | 9.25 | |
| Control | 30 | 53.33 | 7.26 | |
| During discharged | 0.0012 | |||
| Case | 30 | 41.43 | 6.05 | |
| Control | 30 | 47.06 | 4.98 | |
| 2 weeks after treatment | 0.0192 | |||
| Case | 30 | 40.03 | 7.36 | |
| Control | 30 | 43.13 | 4.62 |
a1, Pearson chi-square test; 2, Fisher’s exact test.
Forth aim: Determining and comparing the general conditions of the infants with bronchiolitis at pre-treatment, 24 hours after treatment, during discharge, and two weeks after treatment in the two groups. As shown in Table 6, general conditions did not show a statistically significant difference between the two groups (P > 0.05).
| Time | General Conditions | Group | Case | Control | All | P Value |
|---|---|---|---|---|---|---|
| Before treatment | Normal | Case | 6 | 1 | 7 | 0.124 |
| Control | 20 | 3.3 | 11.7 | |||
| Difficult feeding | Case | 18 | 23 | 41 | ||
| Control | 60 | 76.7 | 68.2 | |||
| Agitation | Case | 6 | 6 | 12 | ||
| Control | 20 | 20 | 20 | |||
| 24 hours After Treatment | Normal | Case | 26 | 20 | 46 | 0.125 |
| Control | 86.7 | 66.7 | 76.7 | |||
| Difficult feeding | Case | 4 | 10 | 14 | ||
| Control | 13.3 | 33.3 | 23.3 |
5. Discussion
Bronchiolitis is a lower respiratory viral disease and a cause of wheezing (13). Diagnosis is generally based on history and clinical examination, and about 3% of infants are admitted due to bronchiolitis in the first year of infancy (6). Proper treatment and wheezing control can reduce the risk factors for asthma in infants and consequently reduce morbidity (5, 10, 11). So far, no definitive treatment has been introduced for bronchiolitis, but the common treatments include using supportive cold nebulizer and bronchodilator (15).
Due to the role of vitamin A in the epithelium stabilization of the lower respiratory tract and immune system, (12) the present study aimed to investigate the effect of vitamin A on persistent wheezing in 60 infants with bronchiolitis referred to Ali Ibn Abi Talib Hospital of Zahedan, Iran in 2018. The mean age and frequency of sex were not significantly different in the two groups.
The results of our study showed that the severity of wheezing was not significantly different in infants before and 24 hours after treatment. However, while 6.7% of infants in the control group had severe wheezing during discharge, no wheezing was reported in the case group. Also, there was no significant difference between the severity of retraction and general conditions in the infants of the two groups. There was also a significant decrease in the respiratory rate in both groups, which was observed until the end of the follow-up.
Pinnock et al. evaluated children’s respiratory diseases and reported that children with frequent episodes of respiratory problems benefited from vitamin A supplements. In a randomized clinical trial in 1988, they also investigated 206 children aged 2 to 7 years with a history of hospitalization during infancy due to bronchiolitis and treated them with vitamin A supplementation. The results showed that this supplement did not alter plasma retinol levels and did not affect respiratory morbidity (22). These results are in line with the findings of our study.
In our study, it was found that vitamin A supplementation in infants could improve wheezing, and it did not have a negative effect on the general conditions and retraction of patients.
Another study conducted by Dowell et al. in Chile aimed at assessing the effect of high-dose vitamin A on RSV infection in 180 children aged one month to six years old. Based on the specimen from the nose, the patients were treated with oral vitamin A (50,000 to 200,000 IU retinol palmitate based on age) and placebo. The results showed that there was no significant relationship between the administration of vitamin A and the reduction in hospitalization period, the need for oxygen, or the time of loss of hypoxemia. However, in the analysis of subgroups, it was found that the administration of this vitamin resulted in a significant reduction in the duration of tachypnea and shortening of the hospitalization period for children who had severe hypoxemia during admission (23). In our study, the duration of hospitalization was not studied, but it was found that administration of vitamin A could reduce wheezing; but its effect on reducing the respiratory rate was similar to that of the control group.
On the other hand, some studies have found that the prevalence of vitamin A deficiency is higher in patients with persistent wheezing, and serum retinol levels are associated with the severity of this wheezing (24). These results are in contrast with the results of our study. In our study, it was found that the administration of vitamin A in infants improved their wheezing and had no negative effects on the general conditions and retraction of patients.
Although the serum vitamin A level was not measured in our study, it could be concluded that the serum vitamin A level increased in the case group after treatment, which was associated with a decrease in the severity of wheezing. The reason for this difference may be due to the difference in the sample size, study design, demographic characteristics of the patients, and the effects of the confounders. Therefore, serum vitamin A levels are important at prior to treatment. (25).
In this regard, Sharafian et al. examined the effect of vitamin A on persistent wheezing after bronchiolitis in 84 one- to twelve-year-old infants in Yasouj, Iran. In this study, patients diagnosed with viral bronchiolitis were randomly assigned to two groups (case and control). The control group received conventional treatments for bronchiolitis, including cold nebulizer and wet oxygen with bronchodilator, and the case group received a vitamin A dose of 5000 units per kilogram in addition to the above-mentioned treatment. The severity and rate of wheezing were examined in the two groups at pre-treatment, after the treatment, as well as one and two weeks after the treatment. After two weeks, there was a significant decrease in the severity and rate of wheezing in the group receiving vitamin A compared to the control group (P < 0.05). The authors concluded that the administration of a dose of vitamin A in hospitalized patients due to viral bronchiolitis can significantly reduce post-bronchial wheezing (24). The results of this study are in line with the findings of our study.
Tian et al. examined the causes of bronchiolitis in infants and reported that (a) lack of breastfeeding, exposure to cigarette smoke, and vitamin A and D deficiency were a major contributor to the onset of RSV bronchiolitis; (b) exposure to cigarette smoke, vitamin D deficiency, a history of atopy and a family history of atopy were important risk factors for wheezing after bronchiolitis in children; (c) patients with eosinophilia, high serum IgE, RANTES, and a decrease in the ratio of TH1 to TH2 increased the risk of wheezing (26). However, in our study, it was found that vitamin A has a direct relationship with the wheezing of patients, which is inconsistent with the results of the study. The reason for this difference may be due to the difference in sample size, type of study, demographic characteristics of patients, and the inclusion criteria. T
In a study by Ellison, vitamin A supplementation was associated with a 60% reduction in mortality in measles patients, which researchers attributed to the effect of vitamin A on the immune system and epithelium (27).
In a study by Tiras et al. (28), the relationship between RSV infection and vitamin A serum levels in children with bronchiolitis in Turkey was examined and No relationship was detected between RSV infection and decrease of serum vitamin A levels.
In a study on serum vitamin A levels in 400 patients aged 3 to 36 months with wheezing, Shalaby et al. concluded that low levels of vitamin A are associated with persistent wheezing and acute respiratory disease (29). Although these results were in line with our findings, the study design was different from ours.
In a study in Australia on 206 children aged 2-7 years with a history of bronchiolitis leading to hospitalization, measuring serum levels of vitamin A and its administration showed that administration of vitamin A supplements could not raise serum retinol levels, and it did not affect the morbidity rate (30). These results are in contrast with the results of our study.
5.1. Conclusions
The results of this study showed that the severity of wheezing in infants receiving vitamin A significantly decreased during discharge and two weeks after treatment. Therefore, considering the prevalence of bronchiolitis in children and the high incidence of wheezing in infants following bronchiolitis, and given the direct effect of vitamin A on reducing infant wheezing, it is recommended that vitamin A along with other treatments be administrated for infants with symptoms of bronchiolitis.