1. Background
Fecal incontinence is defined as the lack of ability to retain fecal matter, happening once a week or more in children older than 4 years (1), which may result from organic or functional deficits (2). The prevalence of this disorder varies from 0.8 - 4.2% in Western countries to 2 - 7.8% in Asian countries, including Iran and South Korea. Sohrabi et al. (cited in Sarveazad et al.) reported fecal incontinence as the third most common among the gastrointestinal symptoms in Iranian adolescents (3). Due to the unhygienic nature of fecal particles and their foul odor, fecal incontinence affects the daily functional life of children (4). Moreover, it has many implications for the child’s individual, social, and family life. These children are generally excluded from their peers and may experience many social problems because of absence from school, lack of confidence, and imposed shame. Additionally, due to the chronic nature of their disease and lack of compatibility mechanisms (5), several observations confirming depression, anxiety, and aggression have been reported. Furthermore, the evidence showed that a significant number of children with fecal incontinence are at risk for psychological disorders (1, 6, 7). Meanwhile, fear of upsetting others and attracting their negative attention can cause aggression and anger in the family; therefore, child abuse (physical and emotional) has been reported in these children (4). Hence, not paying attention to these problems can cause many harms to these children and their family (6), as well as affecting the quality of life (QOL) in them (5).
The QOL is defined as the individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals (8). Various studies have demonstrated that children with fecal incontinence experience a lower QOL (9, 10). For example, Kianfar et al. indicated a severe emotional disturbance while assessing the QOL (11). In addition to emotional disorders, Bongers et al. reported disorders in the social aspects (12). Since a high-quality life not only requires resources and health, but also satisfaction and mental understanding of the social situation, it is necessary to pay attention to the QOL in these children and to wisely choose strategies to improve it.
There are a variety of invasive and non-invasive therapies for treating fecal incontinence, even though there are some complications and limitations in some children. Surgical procedures, as invasive procedures, work well in 20 - 60% of cases, but postoperative complications such as narrowing, leakage, and granulation are common. Biofeedback and spinal nerve stimulation are non-invasive methods which need advanced tools, an observer, and being in an outside environment such as a clinic (13). Despite their great success, these methods are difficult to accept. In contrast, the bowel management program (BMP), developed by Dr. Alberto Peña and Mark Levitt for 30 years, is a low-cost method easily learned by parents with a success rate of 95% (10). This program aims to keep the children completely clean within 24 hours, including enema, constipation-causing regimens, and medications to reduce intestinal movements that vary with each individual’s conditions (14). Implementation of this program requires a team approach in which the nurse is a key member respecting its holistic approach, as well as its educational role (15). The BMP promotes independence and self-sufficiency in children, helping them to integrate into the community; it also enhances their sense of well-being and provides them with a high-quality life (16). Similarly, numerous studies have shown that carrying out this program has a great impact on improving the QOL in children with fecal incontinence (13, 17). In a 2016 study evaluating the impact of BMP on the QOL in children with fecal incontinence, the QOL significantly improved in all aspects (13).
Considering the high number of fecal incontinence cases in Iran and the lack of studies in this area, it is critical to pay more attention to this issue. Since Mofid Children’s Hospital provides comprehensive services to children and it is a referral center for children from all over Iran, in this study, it was selected as the main location for presenting Peña BMP.
2. Objectives
This study aimed to determine the QOL in children with fecal incontinence before and after bowel management training program at Mofid Children’s Hospital in Tehran, Iran, from 1 February 2019 to 1 February 2020.
3. Methods
3.1. Study Population
This clinical trial study aimed to determine the effect of bowel management training program on QOL of subjects (age range: 4 - 18 years) suffering from fecal incontinence referred to the gastrointestinal and surgical clinic of Mofid Children’s Hospital in Tehran, Iran. Since Mofid Children’s Hospital provides comprehensive services to children and it is a referral center for children from all over Iran, in this study it was selected as the main location for presenting Peña BMP.
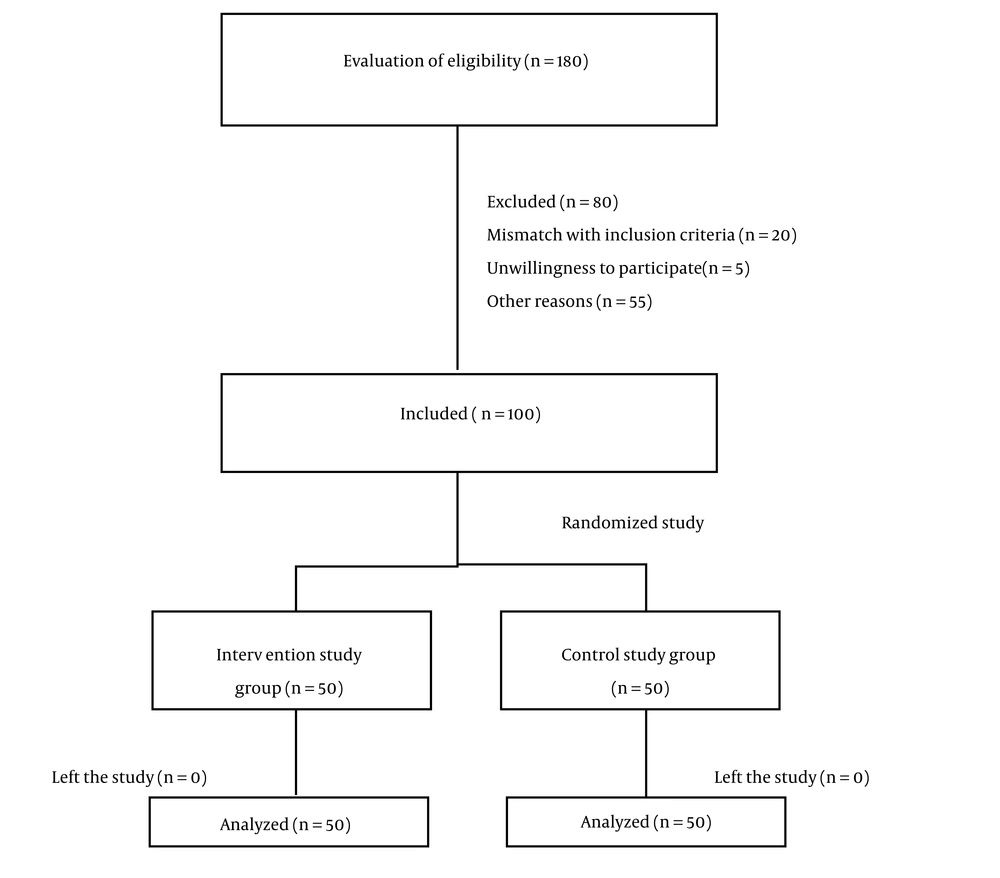
Children were selected by purposive sampling method based on inclusion criteria and randomly assigned into two groups of intervention and control. Inclusion criteria were: Willingness to participate in the study; ability to speak Persian; and a definitive diagnosis of fecal incontinence by a pediatric surgeon or pediatric gastroenterologist. Exclusion criteria were: Not willingness to continue participating in the study; absence in more than one session of the training program; not following the training program for more than one day; and inability to speak Persian. The procedure of sampling lasted from February 2019 to July 2019. Using the study by Wang et al. (18) and considering 5% error, 80% study power, and 10% loss n ≥ 2 (
3.2. Demographic Data and Clinical Characteristics
To collect data, two questionnaires, including the Demographic Characteristics Questionnaire and the Quality of Life in Children Questionnaire were used. The Demographic Characteristics Questionnaire includes such information as age, sex, birth order, education level of children and parents, fecal disposal pattern, surgical history, medical history, and fecal consistency based on the Bristol table. The Quality of Life in Children Questionnaire was designed by Warren in 1999 and includes four aspects of physical, emotional, social, and school-related performance. While the physical aspect has eight questions, each of the other aspects has five questions in both self-reported and parent-reporting categories. The 5-point scoring system from “zero=never” to “four=almost always” was designed. The total score ranged from zero to 92 and a higher score indicated better QOL. Face validity was used to determine the validity of the instrument. To this end, the tools were initially distributed among five eligible subjects to evaluate the simplicity and comprehensibility of the questionnaires. After translating, the Peña BMP was reviewed and localized according to the opinions of six specialist physicians, three pediatric surgeons, three pediatric gastroenterologists, three gastrointestinal nurses, and four nursing faculty members. Reliability of the research instrument was assessed by examining consistency (Cronbach’s alpha coefficient) and stability. To do so, a questionnaire was completed by 15 subjects twice within two weeks, and intra-class correlation coefficient and Cronbach’s alpha were calculated. The patients were selected based on inclusion criteria after referring to the pediatric surgical and gastrointestinal clinic of Mofid Children’s Hospital. After obtaining a written informed consent from the participants and their parents, the subjects were randomly assigned into two groups of intervention and control. Then, the questionnaires were completed by the subjects and their parents. Both groups were initially evaluated clinically by the physician. The evaluation included the assessment of chief complaint, past medical history, drug history, abdominal and pelvic physical examinations, and palpation of the rectum as needed. Moreover, abdominal x-ray radiography was also requested at this stage. In the intervention group, the bowel management training program was administered individually for a maximum of one hour per day, with the presence of the patient and the primary caregiver in a room at the surgical clinic of Mofid Children’s Hospital for seven days in a row. Participants in the control group received only medical treatment. Table 1 indicates the main process of research in the first seven days of the study.
| Timeline | Process |
|---|---|
| Day 1 | Introduction, obtaining written consent, completing the Demographic and Quality of Life Questionnaires by the subjects or their home caregivers. Preparation of pediatrics bowel management training program by a researcher and physician. |
| Day 2 | Education of pediatrics bowel management training program to the primary caregiver. Providing educational booklet. |
| Day 3 | Previous plan approvement or designing a new program at the discretion of a physician. Evaluation of bowel management in collaboration with a physician. Responsiveness to the questions of parents and learning assessment. |
| Day 4 | Evaluation of bowel management in collaboration with a physician. Responsiveness the questions of parents and learning assessment. |
| Day 5 | Evaluation of bowel management in collaboration with a physician. Responsiveness the questions of parents and learning assessment. |
| Day 6 | Evaluation of bowel management in collaboration with a physician. Responsiveness the questions of parents and learning assessment. |
| Day 7 | Evaluation of bowel management in collaboration with a physician. Responsiveness the questions of parents and learning assessment. |
The Main Process of the Research in the First Seven Days of Introduction, Education, and Evaluation of Participants
3.3. Intervention
In the first session, the researcher introduced the purpose of the study and the method of intervention to the subjects and their parents. The physician examined the patients based on the pattern and frequency of defecation, as well as fecal consistency and shape. Diet, behavioral and excretory habits, and abdominal and perinea examinations were also performed. Then, the educational curriculum was formulated exactly after the initial review. On the second day, the individualized training program was implemented. Then, the patients’ knowledge was assessed by asking some questions and re-educated if needed, and all the questions raised by subjects and their parents were addressed. At the end, they were given a training booklet. In subsequent sessions, physical examinations and paraclinical bowel studies were performed at the discretion of the physician, and subsequently, the bowel evaluation management was assessed. The following sessions were conducted based on the previous programs, individual training, as well as questions for assessing the knowledge of subjects and parents. On the seventh day, the BMP was finalized and re-explained to the patients and their parents. Then, the subjects and their parents followed the program for one month. Afterward, they were referred to the clinic for re-examination and stabilization of the program. The Quality-of-Life Questionnaire was completed again by the subjects and their parents. During this month, all patients could contact via making phone calls to ask their questions in the morning shift.
3.4. Statistics Analysis
Data were analyzed by SPSS 21 software using t-test or Mann-Whitney U tests for quantitative variables and chi-square and Fisher’s exact tests for classified variables. A P-value less than 0.05 was considered a significant difference.
3.5. Ethical Approval
All the steps in this study were in accordance with the ethical criteria of the Ethics Committee of Shahid Beheshti University of Medical and health Sciences (ethics code: IR. SBMU.PHNM.1397.150 and registration code: IRCT, IRCT20181113041644N1).
4. Results
In this study, 100 subjects (males = 60 vs. females = 40) were assigned into two equal groups of intervention and control (n = 50 each). The mean age of participants was 12.07 and 11.63 years in the intervention and control groups, respectively. Based on chi-square and Fisher’s exact tests, the two groups were matched in terms of such demographic information as gender, age group, parents’ education, exemption pattern, surgical history, type of fecal based on Bristol table, mother’s job, father’s job, toilet time, and number of children in the family. Table 2 shows the mean score of QOL before intervention in the intervention and control groups (65.17 ± 14.74 and 63.36 ± 17.25, respectively) (P = 0.692). After the intervention, there was a significant difference between the QOL scores of intervention and control groups (P < 0.05), indicating that the bowel management training program improved the QOL. The results on different dimensions of QOL also showed a significant increase in all dimensions in the intervention group, with the highest increase in social (P < 0.001) and physical (P < 0.001) dimensions. In the control group, there was a significant difference in the emotional dimension (P = 0.002), so that the scores significantly decreased after one month. There was no significant difference in other dimensions of the control group.
| Children’s Quality of Life | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| Pre-intervention | Post-intervention | P-Value | Pre-intervention | Post-intervention | P-Value | |
| Overall score | 65.17 (14.74) | 78.78 (10.89) | < 0.001 | 63.36 (17.25) | 64.19 (12.56) | < 0.757 |
| Physical activity | 70.37 (18.34) | 84.56 (10.68) | < 0.001 | 71.25 (20.95) | 80.50 (13.13) | < 0.056 |
| Emotional issues | 46.50 (19.90) | 68.00 (13.70) | < 0.001 | 53.90 (27.80) | 36.60 (21.60) | < 0.002 |
| Social issues | 75.70 (16.53) | 87.30 (13.02) | < 0.001 | 70.30 (20.23) | 75.40 (20.40) | < 0.169 |
| School environment | 72.22 (20.76) | 79.77 (11.57) | < 0.012 | 61.89 (16.97) | 57.02 (15.15) | < 0.221 |
Comparison of the Mean (SD) Quality of Life Between the Intervention and Control Groups
5. Discussion
The purpose of this study was to evaluate the effect of bowel management training program on QOL of patients with fecal incontinence. The results demonstrated that the QOL in participants was low before the intervention, which is consistent with the results of some previous studies (7, 12, 19, 20). Fecal incontinence can impair physical functionality, and consequently affect emotional and social aspects of well-being. Regarding the physical aspect, after practicing the BMP, the subjects performed better in walking-related activities, running, exercising, lifting equipment, bathing, and they had more energy to do the things. In this regard, Wang et al. (18) demonstrated that the implementation of a BMP on 48 children with fecal incontinence reduced the score of the Cleveland index, meaning that they had a greater control over defecation. The Cleveland Index indicates the type of fecal incontinence (rigid, fluid, or gas) and the frequency of defecation (from complete control to severe incontinence; with 0 indicating perfect control, and 20 indicating severe incontinence). The fear of upsetting other people and their negative attention caused hostility and anger in the family of these patients. As a result, both forms of physical and emotional child abuse have been reported in these children (4).
In addition to the physical aspect, the regulation and control of defecation has also influenced the emotional and social aspects (12). Children afflicted with fecal incontinence often spend their time at home in fear of incontinence and are generally unable to communicate with their peers. So, they experience many psychological and social problems. The results of this study illustrated that in terms of emotional aspects, feelings of fear, anxiety, anger, sleep problems, and worrying about the future were among the negative emotions among our participants, which significantly decreased after holding the training sessions. Similarly, Wang et al. showed that children with fecal incontinence were more sensitive and shyer, and they had more difficulty in concentrating compared to normal children. After several months, a significant improvement in QOL was observed in children attending a BMP, leaning particularly more towards the emotional aspect of life (18). Based on the evidence, children’s presence in the community and playing with their peers were linked with heightened self-esteem, as well as with diminished negative thoughts and feelings (6). Furthermore, fecal incontinence had major social effects on the child (21). In the social aspect (e.g., communication and group activities), the patients got better scores after one month. Daily exercise was an integral part of our program whereby children took part in community activities and were more successful in communicating with other children. In the training programs, we considered the need for walking and exercising lightly. Also, helping the child to stay in the community while maintaining an acceptable level of hygiene and a reduced sense of shame was prioritized, which consequently promoted the child’s social activity. Evidence also suggests that children will no longer have to worry about being unhygienic after experiencing a BMP and will experience a sense of freedom and enjoy their life (16). Perhaps one of the reasons for this success is the impact of the day-to-day follow-up and support of the team nurse, which has increased the motivation of children and their parents in carrying out the program. Consistent with these results, Bongers et al. showed a significant association between social functionality and fecal incontinence (12). Children with fecal incontinence reported lower levels of social functioning in health-related QOL in the social functioning domain (12). In a study by Falirus, children with defecation disorders had lower social scores (20). From an educational point of view, higher scores were observed regarding school absenteeism, concentration, and coursework. Because of improved physical condition and better control over defecation, the number of absences was reduced. In the same manner, due to increased intervals of being clean and, reduced stress caused by dirty underwear, as well as reduced pain and concern, the level of focus and concentration shown by children in the classroom was increased. In general, QOL is a principal matter in caring for a chronic patient (7). In this study, the results of evaluating the QOL in children one month after implementing the Peña BMP illustrated a positive effect on all aspects of children’s life, including physical, mental, emotional, and scholastic aspects. Previous studies have also reported the effectiveness of the program in improving the QOL of children (13, 14). Wang et al. illustrated that the implementation of this training program improved the QOL in all aspects. The mean score of QOL in this study rose from 59.14 to 73.09, indicating the effectiveness of the BMP based on its unique bowel management plan (18). Peña BMP, by examining the intestinal function of each individual child, can improve intestinal function (14, 16). Therefore, in addition to focusing on improving the child’s symptoms, this program caused other factors such as preferences, priorities, the available resources, and the cultural context to play a role. Therefore, it is expected that the child will feel better about his/her life and be more satisfied with the selected treatment, which could justify the improvement in QOL. Another possible reason for the success of this treatment may be attributed to the multidisciplinary approach to bowel management. In this approach, different aspects of the disease are managed in a coordinated manner; so, it is well-expected to increase satisfaction and QOL in patients. The nurses can teach these programs to the children and their families. A structured BMP can improve bowel symptoms and enhance overall QOL in patients. Bowel management should be a priority for patients admitted to rehabilitation and children’s wards.
According to various studies, non-adherence to the BMP treatment in the long run and poor compliance of patients are among the well-known challenges of this method of treatment (13, 22). Although the results of this study showed the efficacy of the BMP in most patients, the short duration of follow-up is one of the weaknesses of this study. Further studies with longer follow-ups are suggested to determine the consistent effectiveness of this program.
5.1. Conclusions
According to our results, despite various treatment modalities, BMP can help children with a poor QOL due to fecal incontinence and significantly improve their QOL. Therefore, indigenized adaptation of the Peña program to improve the QOL in comprehensive gastrointestinal centers for children is suggested. The BMP is an effective way for the treatment of fecal incontinence and improving the patient’s QOL.
According to the results of this study, we could run a center as a pilot for providing BMP for children with fecal incontinence, and develop it to other centers in Iran. However, further research is required in this respect.