1. Introduction
Iodine is an essential micronutrient for the synthesis of thyroid hormones, and inadequate iodine intake affects the physical and mental development of millions of people worldwide (1). The World Health Organization (WHO) recommends daily iodine intake of 120 µg for age group of 7 - 12 and 150 µg for adults above 12 years old (2). Iodine levels below these guidelines may lead to iodine deficiency disorders (IDD), whose physiological consequence is impaired thyroid hormone synthesis and endemic goiter (3). The most important indicator to monitor IDD is the median urinary iodine (MUI) concentration. According to the WHO/UNICEF/ICCIDD recommendation, the iodine concentration of a spot urine sample in 8- to 10-year-old children can be used to estimate the iodine status of the population and make sure about sufficiency of iodine intake in the society (4).
At a global scale, approximately two billion people suffer from ID, and IDD is still a challenge for both developed and less-developed countries (5). During the last 25 years, remarkable progress has been made toward the elimination of IDD worldwide. Universal salt iodization, in which all salt used in food processing, household, and agriculture should be iodized, is the agreed strategy for overcoming ID (6). The salt iodization programs have been implemented in more than 140 countries. It is estimated that about 70% of the world population are using iodized salt every day (7). According to Fan et al., the number of countries with ID has decreased from 110 in 1990s to 15 in 2016 (8).
Iran has a long history of controlling ID so that it took the first initiative in the region and established the Iranian National Committee for IDD Control in 1989 (9). A nationwide survey in 1989 revealed that goiter prevalence in most provinces was between 30 - 80% and the MUI was 1.2 - 8.2 µg/dL in different provinces of the country (10). The iodized salt was distributed and consumed from 1990, and in 1994 the first law was passed by the Iranian parliament that all salts for household use should be iodinized (11). The first national survey regarding the monitoring of this policy was conducted in 1996 (10).
2. Objectives
Since the implementation of IDD control in Iran has been started for more than 30 years, the effectiveness of this program on ID control is unclear. Hence, this study aimed to compare the ID situation in Iranian 8- to 10-year-old children in 2017 and 2017.
3. Methods
3.1. Data Collection
In this study, we used the Iran's health ministry national data in 1990 and 2017. According to the Iranian National Committee for IDD Control and based on the WHO protocols, the provincial medical universities measure urinary iodine in 8- to 10-year-old Iranian students. Iran is subdivided into 31 provinces and the population is under the supervision of provincial medical universities. The sample size of each university was about 240 students and cluster sampling method was used for sample selection (48 clusters in each area). From each cluster, five students (boys and girls equally) were randomly selected. Students who had history of thyroid disease or confirmed use of thyroid-related medication were excluded. Totally, 13,389 and 2,917 samples from the entire country were collected in 2017 and 1996, respectively. The urinary iodine concentration was measured in central laboratory of each university, and acid digestion method was used for measurement. The MUI concentration < 2 µg/dL was considered as severe ID, 2 - 4.9 µg/dL as moderate ID, and 5 - 9.9 µg/dL as mild ID. Also, the MUI concentration of 10 - 19.9 µg/dL indicated adequate iodine intake, 20 - 29.9 µg/dL indicated high iodine intake, and > 30 µg/dL indicated excessive iodine intake.
3.2. Ethical Consideration
The parents of all the included children signed a written informed consent before starting the experiment. The project was approved by the ethics committee of Shahid Beheshti University of Medical Sciences (No: IR.SBMU.RETECH.REC.1399.1037).
4. Results
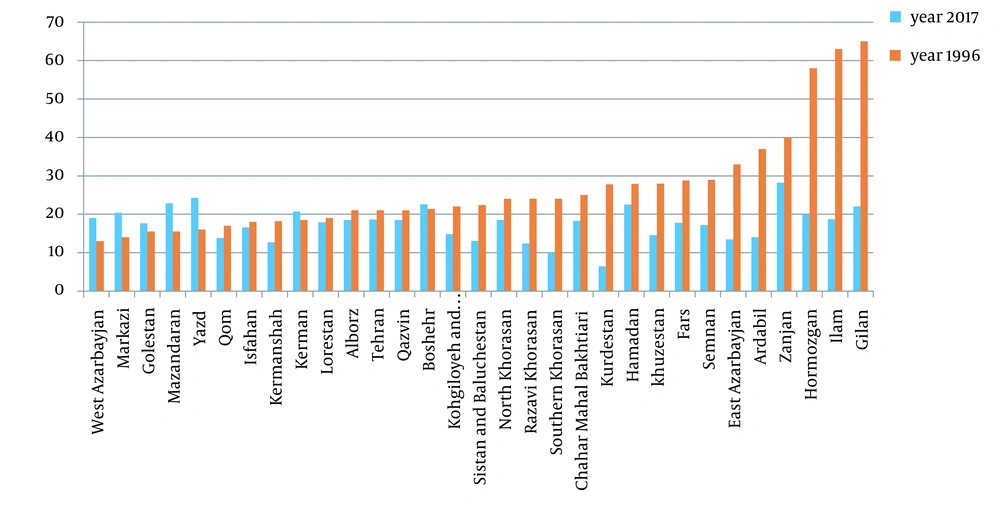
A total of 13,389 and 2,917 urine samples were examined for monitoring in 2017 and 1996, respectively. The MUI concentration was 18.26 µg/dL in 2017 and 20.5 µg/dL in 1996. Figure 1 compares the MUI status of Iranian provinces in1996 and 2017. As can be seen, in 1996, the median amount of MUI status in most provinces was higher than 2017 (except for West Azerbaijan, Markazi, Golestan, Mazandaran, Yazd, Kerman, Bushehr). Among the provinces, the MUI was inadequate (6.42 µg/dL) only in Kurdistan province.
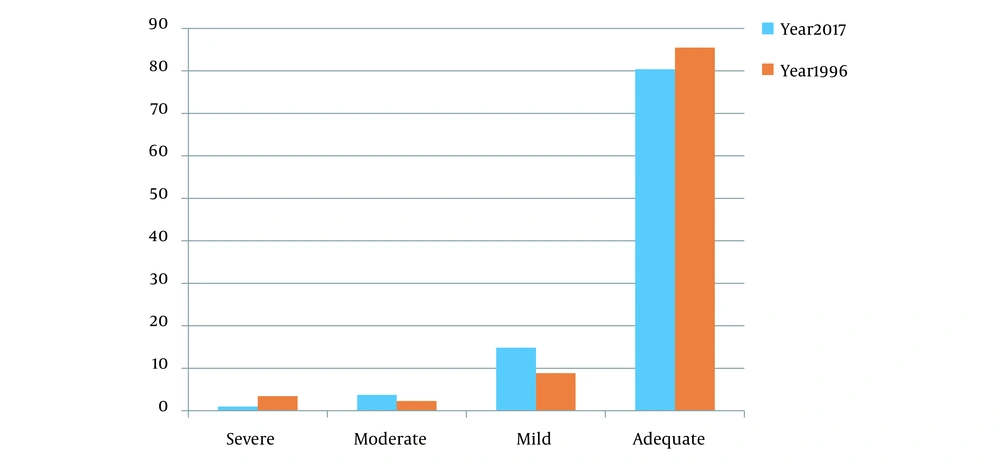
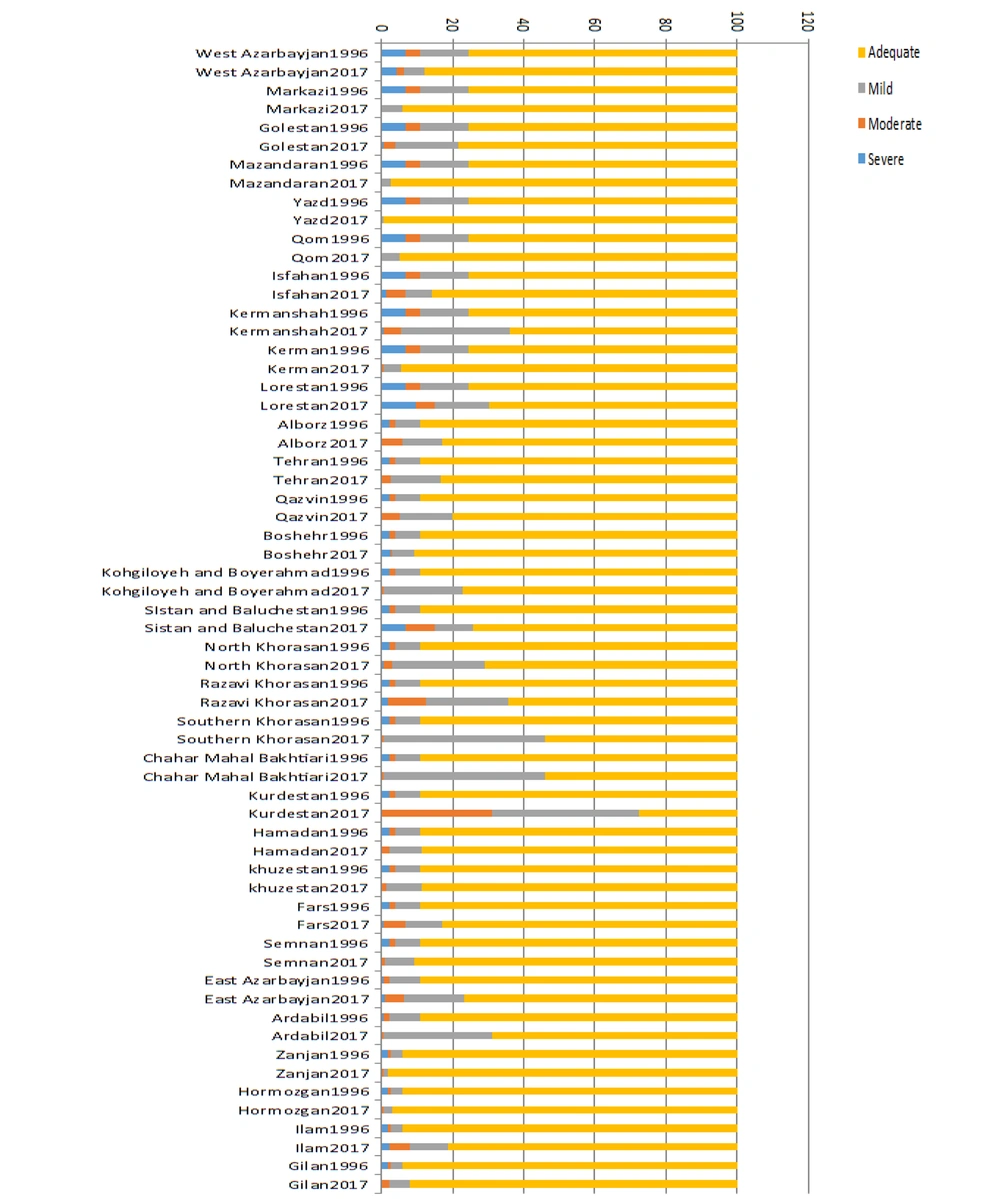
Based on urinary iodine index, 85.47% of students in 1996 had adequate levels, while in 2017, this rate was 80.39%. Also, mild, moderate, and severe ID rates were 8.83%, 2.3% and 3.43% in 1996 and 14.86%, 3.72%, and 1.01% in 2017 (Figure 2). The ID rates in different provinces have been presented in Figure 3.
5. Discussion
This study demonstrated the solid progress toward the implementation of IDD control program in Iran. We reported the iodine status of Iranian students in 2017 and compared it with the first national report carried out in 1996. According to our results, 80.39% and 85.47% of students had no ID in 2017 and 1996, respectively. According to the Global Iodine Network report in 2017, the assessment of iodine status in school-age children has been conducted in 143 countries. Based on the results, about 78% of the reports were in an appropriate range (12). Based on the Iranian National Committee for IDD Control, the MUI excretion was 20.5 µg/dL, and the IDD elimination program was very effective (10). Despite unchanged way for urinary iodine measurement during 1996 to 2017, the fall in MUI could be due to iodized oil injection in earlier years of program initiation, inadequate iodine content of salts, or dietary habits change, particularly in young people. A similar result was previously observed in China National IDD report about iodine status of 8- to 10-year-old children within 20 years follow-up (13).
Figures 2 and 3 report the distribution of ID in 1996 and 2017, respectively. As shown, the mild and moderate deficiency rate in 2017 was higher than 1996, but the severe deficiency in 2017 was almost three times lower than 1996 (1.01 vs. 3.43 µg/dL). It seems that the most important success of this program during these years was reducing the severe deficiencies. Zimmermann in 2012 (14) showed that iodine supplementation has clear benefits to severe iodine deficient populations. However, the short- and long-term implications of mild and moderate ID are still unclear.
Although the adequacy of iodine intake at national level was indicated in this study and some similar reports (15, 16), the policymakers should consider that the IDD control programs are vulnerable and a long-term commitment from salt industry, donors, governments, and consumers is necessary (16). In several countries in which IDD had been eliminated, monitoring faltered, and IDD recurred (17, 18). Therefore, to ensure the achievement of a sustained IDD control program, monitoring of the indicators is a vital element. Also, according to the importance and standardization of ID handling in children, the best way for education and also proper use of iodine in this issue is to utilize public and bulletins guidelines by the National Committee for IDD Control. In critical medical situations, the guidelines and public bulletins are very practical for parents and primary care physicians to use the elements properly and manage the general medical situations (19).
The present study had some limitations. First, our analysis was merely based on serum iodine concentration, and other clinical and biochemical indicators were not considered. Second, the lack of information about the students’ household, socio-economic status, and dietary sources of iodine impeded a comprehensive interpretation.
5.1. Conclusions
Based on our findings, the IDD control program in Iran was found to be very useful in controlling the risk of ID 20 years after the first national survey. Comparing the ID status in 1996 and 2017 showed that the main achievement of this continuous program was reducing the severe ID rate.