1. Background
Breastfeeding is the source of nutrients in children aged 6 - 23 months. It plays an important role in providing energy to babies aged 6 - 12 months, and one-third of energy needs between 12 and 24 months. Moreover, the mortality rate is lower in breastfed babies, and breastfeeding is also a critical source of energy and nutrients during illness (WHO). Breastfeeding is useful for the mother and the newborn and significantly controls chronic diseases (1). Statistics show that the lack of breastfeeding in developing countries contributes to the death of 1 child every 30 seconds and 1.5 million children annually, accounting for 70% of the neonatal mortality in these countries (2). Evidence suggested that 149 million children under five were stunted, 45 million were wasted, and 38.9 million were overweight or obese in 2020.
Factors such as the mother’s age and education, family income, family support, prenatal actions, decisions about the first breastfeeding, time of the first feeding, as well as maternal skills and self-efficacy, are effective in successful breastfeeding (3). Self-efficacy, the perceived ability to successfully perform a task, is an important principle linking awareness to action (3). Self-efficacy affects individuals’ decisions, choices, activities, and persistence (4). Fathers’ attitudes and support are alterable factors that significantly affect breastfeeding onset (5). Paternal breastfeeding self-efficacy denotes the father’s ability to help mothers breastfeed their newborn (6). Breastfeeding cessation may be due to the feelings of frustration and guilt or even helplessness in fathers as they might think that they cannot help, and starting formula feeding might seem the most straightforward solution (7).
Fathers' involvement in breastfeeding training can improve the amount and duration of exclusive breastfeeding (EBF) (8, 9). Fathers’ participation in breastfeeding promotion programs in maternity wards can significantly increase EBF in the first six months of a newborn’s life, probably due to the information given to fathers in these wards about EBF. Paternal training can encourage fathers and thus, have a positive effect on mothers in avoiding feeding the infant with water, herbal drinks, or different formulas (10). Fathers’ self-efficacy score is significantly correlated with mothers’ self-efficacy, attitudes toward breastfeeding, the importance of breastfeeding for the father, the promotion of breastfeeding, EBF, and the belief in making progress in breastfeeding (6).
Improved paternal breastfeeding self-efficacy and mothers’ perception of fathers’ cooperation and assistance show that programs to support parental cooperation in breastfeeding can benefit the parents (11). Given the recommendations of WHO about the role of breastfeeding in children’s health, the impact of parents’ self-confidence in this matter, and the more prominent role of fathers and their breastfeeding support, there is undoubtedly a need to conduct further studies on this subject.
2. Objectives
This research seeks to determine the relationship between paternal breastfeeding self-efficacy and infant and young child feeding practice.
3. Methods
3.1. Samples and Procedures
This descriptive-correlational study was conducted after obtaining the necessary approvals from the Ethics Committee of Shahid Beheshti University of Medical Sciences (ethical approval: IR.SBMU.PHARMACY.REC.1398.060). After the verbal consent, 220 couples were recruited for the study in a hospital in Karaj. Baseline data were collected from fathers and mothers in the hospital. Mothers were in the postpartum ward, and fathers waited for the mothers and their babies outside the postpartum ward. Follow-up data were collected from mothers three months postpartum via telephone. The inclusion criteria were the parents living together, not taking any medications affecting breastfeeding, singleton birth, birth weight over 2500 grams, gestational age of 37 weeks or more at delivery, normal Apgar score at birth, and no neonatal diseases or anomalies. The exclusion criteria entailed the lack of access to the subjects to complete the questionnaire three months after delivery and severe postpartum complications for the mother or newborn that had either separated them or led to their death.
3.2. Measures
Data were collected from fathers and mothers in hospitals and mothers three months after delivery. The data collected in the hospital included (1) personal characteristics, such as maternal and paternal age, education, and income; (2) mothers' midwifery characteristics, such as gravidity, type of delivery, and prenatal disease; (3) infant characteristics, such as gestational age and weight; (4) paternal breastfeeding self-efficacy. The data collected three months after delivery encompassed infants' feeding practices. The Breastfeeding Self-efficacy Scale-short form (Appendix 1) (6) was used to assess paternal self-efficacy. This questionnaire consists of 14 items scored based on a 5-point Likert scale from “always confident” to “not at all confident." The lowest score is 14, and the highest is 70. This scale was initially developed in English and was translated into Persian using the forward-backward translation method. For this purpose, the English version of the scale was first translated into Persian by two translators with expertise in medical texts. Next, the translations were compared by two obstetricians who were also faculty members, and a Persian version of the tool was prepared by matching the items in terms of meaning and concept and selecting the best options. To ensure the expressiveness of the sentences in the Persian text and their match with the original text, the initial translated version was re-translated into English by two other translators who could speak English very well and had not seen the original questionnaire before. Afterwards, the two English versions were compared, and the necessary corrections were made. A single version of the Persian questionnaire was developed (12). In order to assess the questionnaire’s face validity, it was distributed among ten fathers, who were asked to comment on the legibility, clearness, writing style, grammar, and spelling of the words, as well as the ease of completing the tool. In the present study, the reliability of this questionnaire was confirmed by Cronbach’s alpha coefficient of 0.94.
Infant and young child feeding practices were assessed by the infant nutrition questionnaire three months after delivery via phone calls to the mothers participating in the study. This questionnaire was prepared using the WHO model and was distributed among ten faculty members of the Midwifery and Reproductive Health Department of Shahid Beheshti University of Medical Sciences for content and face validity evaluation. The final infant and young child feeding practice questionnaire was developed based on their comments. Infant feeding practices were assessed based on the practices in the last 24 h prior to the study as defined by WHO. This questionnaire includes questions about the breastfeeding methods of mothers, reasons to use infant formula, maternal physical and mental illness three months after delivery, mothers’ incentives for breastfeeding, and support and opposition of spouses and others for breastfeeding. A demographic information questionnaire was also designed for the study, and its content validity was approved. Data were analyzed by the SPSS software version 23 using descriptive statistical methods, including the frequency, percentage, mean, and standard deviation tables. Moreover, the inferential statistical methods included the independent t-test, analysis of variance, Spearman’s test, and chi-squared test. At the end of sampling, 14 people were excluded from the study, reducing the sample size to 206. The reasons for this sample loss entailed not answering the phone calls (n = 10), the mother’s unwillingness to continue cooperation (6), and the death of the infant (6).
4. Results
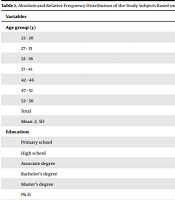
In the present study, the mean age of fathers was 33.79 years. Table 1 presents the fathers' demographic characteristics, and Table 2 presents the infants' characteristics along with the infants feeding practices. Among the fathers participating in the study, 22.8% had participated in antenatal classes, and 67.6% had cooperated in prenatal care. In addition, 87.9% of fathers chose to breastfeed as their preferred feeding method for their infant during their wife's discharge from the postpartum ward. Furthermore, 85.9% of mothers reported receiving adequate paternal breastfeeding support three months after the delivery, while 2.4% of the fathers opposed breastfeeding during three months postpartum. Among the reasons for their opposition were thinking that breast milk was insufficient, being concerned about the mother's comfort, and the deformation of mothers’ breasts due to breastfeeding. Table 3 demonstrates the relationship between paternal self-efficacy score and the examined variables, indicating that only two variables, namely the father’s cooperation in prenatal care (P = 0.0001) and the father’s attendance of antenatal classes (P = 0.0003), were correlated with paternal self-efficacy score. Table 4 shows the relationship between infant and young child feeding practice and the study variables. The father’s support for the mother in breastfeeding was the only variable correlated with the feeding practice (P = 0.006).
| Variables | Values a |
|---|---|
| Age group (y) | |
| 22 - 26 | 13 (6.31) |
| 27 - 31 | 61 (29.61) |
| 32 - 36 | 77 (37.38) |
| 37 - 41 | 40 (19.42) |
| 42 - 46 | 11 (5.34) |
| 47 - 51 | 2 (0.97) |
| 52 - 56 | 2 (0.97) |
| Total | 206 (100) |
| Mean ± SD | 33.5 ± 79.27 |
| Education | |
| Primary school | 54 (26.2) |
| High school | 109 (52.9) |
| Associate degree | 15 (7.3) |
| Bachelor’s degree | 19 (9.2) |
| Master’s degree | 7 (3.4) |
| Ph.D. | 2 (1) |
| Total | 206 (100) |
| Father’s occupation | |
| Unemployed | 2 (1) |
| Employed | 44 (21.4) |
| Self-employed | 160 (77.7) |
| Total | 206 (100) |
| Housing status | |
| Renting | 103 (50) |
| Owner | 103 (50) |
| Total | 206 (100) |
| Father’s income status | |
| Less than sufficient | 104 (4.4) |
| Sufficient | 94 (50) |
| To the extent of saving | 8 (45.6) |
| Total | 206 (100) |
| Drug use status | |
| Smoking | 34 (16.5) |
| Alcohol | 3 (1.5) |
| None | 169 (82) |
| Total | 206 (100) |
a Values are expressed as No. (%) unless otherwise indicated.
| Variables | No. (%) |
|---|---|
| Newborn’s gender | |
| Female | 104 (50.5) |
| Male | 102 (49.5) |
| Total | 206 (100) |
| Type of delivery | |
| Vaginal delivery | 103 (50) |
| Cesarean section | 103 (50) |
| Total | 206; 100 |
| Variables | Test | P-Value |
|---|---|---|
| Father’s age | Pearson | 0.949 |
| Education | ANOVA | 0.731 |
| Father’s cooperation in prenatal care | Independent-t | 0.001 |
| Father’s attendance of antenatal classes | Independent-t | 0.003 |
| Father’s decision on the type of neonatal feeding | ANOVA | 0.347 |
| Father’s income status | ANOVA | 0.634 |
| Father’s occupation | ANOVA | 0.822 |
| Infant feeding practice three months after delivery | ANOVA | 0.99 |
| Father’s support for breastfeeding | ANOVA | 0.757 |
| Variables | Chi-Square Test Results |
|---|---|
| Father’s education | 0.240 |
| Father’s occupation | 0.194 |
| Father’s income status | 0.406 |
| Father’s attendance of antenatal classes | 0.203 |
| Father’s cooperation in prenatal care | 0.180 |
| Housing status | 0.812 |
| Father’s decision on the type of neonatal feeding | 0.279 |
| Father supports the mother in breastfeeding | 0.006 |
5. Discussion
The current study was conducted to determine paternal breastfeeding self-efficacy and its relationship with infant feeding practices. The mean paternal breastfeeding self-efficacy score before the discharge of mothers was 58.33 out of 70 in the present research. This was the first investigation on the breastfeeding self-efficacy of Iranian fathers, there was no other information that could be used for comparison purposes. In a study by Dennis, the self-efficacy score of Canadian fathers was 48.96 out of 70. This discrepancy and the higher self-efficacy score of Iranian fathers can be due to cultural differences between the two samples and the importance of breastfeeding upon birth in Iranian families. Meanwhile, this study found no relationship between paternal breastfeeding self-efficacy and infants' feeding practices three months after delivery. This finding contradicts the results reported by Dennis, who found a significant relationship between paternal self-efficacy score, attitudes toward breastfeeding, breastfeeding rate, and EBF (6). Nonetheless, Dennis did not specify the feeding practice at 12 weeks (13) and the rate of EBF. In the present study, only 5.8% of Iranian children used formula feeding at three months of age, 74.3% were exclusively breastfed, and 19.9% received both formula feeding and breastfeeding, and there was no relationship between these infant feeding practices and paternal self-efficacy. Another study (14) reported a relationship between paternal self-efficacy score, breastfeeding support, and the onset of breastfeeding, while the long-term breastfeeding pattern (11) was not investigated. Several factors affect infant feeding practices, including but not limited to the father's role. Research findings indicate a direct relationship between fathers' support for breastfeeding and the greater likelihood of continued breastfeeding (15). In contrast, some studies do not find the role of fathers significant in EBF. A study in India (16) suggested that although fathers’ attitude toward breastfeeding is effective, it does not affect the duration of EBF. The present study only examined paternal breastfeeding self-efficacy concerning infant feeding practices. One of the limitations of the current research was the impossibility of measuring the self-efficacy of fathers three months postpartum. If the self-efficacy of fathers had been measured three months after delivery, the trend of changes in this variable could have been better evaluated and analyzed.
We found a significant relationship between paternal breastfeeding self-efficacy scores after childbirth and fathers who cooperated in prenatal care, as the mean paternal breastfeeding self-efficacy score was higher in the fathers who cooperated in prenatal care (P = 0.001). According to the results of the present study, paternal breastfeeding self-efficacy score had a significant relationship with attending antenatal classes (P = 0.003) (17). Attending antenatal classes prepared fathers for accepting the role of father. Research suggested that educating fathers before and after childbirth improved EBF six and four months postpartum, reduced using formula feeding two months postpartum, and decreased breastfeeding problems (16). In the present study, there was no correlation between paternal breastfeeding self-efficacy scores at discharge and fathers’ decision on the type of neonatal feeding after childbirth, their income status, occupation, age, education, and breastfeeding support.
Fathers’ support is a modifiable and alterable factor. Parental cooperation in breastfeeding offers an ideal framework for designing interventions to raise fathers’ involvement and help the parents work together to meet their breastfeeding goals (15). In the current investigation, a significant relationship was observed between fathers' support for breastfeeding three months after delivery and infants' feeding practices three months postpartum (P = 0.006). This finding is consistent with the results of another study (9), which showed that although fathers' attitudes were effective in supporting breastfeeding, infant and young child practice three months after delivery was not correlated with occupation, education, income, housing status, father’s attendance to antenatal classes, father’s cooperation in prenatal care, and father’s decision on the type of neonatal feeding at the time of discharge (18). Moreover, fathers' attitudes were not correlated with the duration of EBF.
5.1. Conclusions
According to the findings of the present study, no correlation was found between paternal breastfeeding self-efficacy scores and infant and young child practice three months postpartum. Paternal breastfeeding self-efficacy scores correlated significantly with the fathers attending antenatal classes and the father's cooperation in prenatal care. Nonetheless, the paternal breastfeeding self-efficacy score was not significantly related to fathers’ age, occupation, education, income, and breastfeeding support. Furthermore, in this study, infant feeding practice was not correlated with the father’s education, occupation, income status, housing status, and decision on the type of neonatal feeding. However, there was a significant relationship between infant and young child practice and paternal support for breastfeeding (P = 0.006).