1. Background
Surgery is a painful, stressful, and traumatic experience for children (1). Postoperative pain is a common issue in pediatric surgical cases (2), with reported incidence rates ranging from 40% to 84% (3). Despite advancements in pain management technology and preoperative care, the level of acute postoperative pain remains high (2). In Iran, pain has been identified as the most frequent postoperative complication (4).
Pain is described as an unpleasant sensory-emotional experience associated with actual or potential injuries, which can range from mild to severe (5). It is well-established that children can experience pain, and its effects can persist from childhood into adulthood (6). Prior to surgery, postoperative pain is a major concern for patients (7). Pediatric pain is often underestimated and overlooked due to myths, beliefs, and challenges in assessment and treatment (6). Numerous factors influence postoperative pain, and there are additional risk factors for experiencing high levels of pain after surgery. Preoperative psychological factors, such as catastrophizing, depression, anxiety, and pain expectations, are significant predictors of acute postoperative pain intensity (7). Various studies have identified factors that impact pain perception.
Knoetze et al. discovered a significant correlation between preoperative caregiver anxiety and postoperative pain in children undergoing elective ambulatory surgery (with a moderate correlation) (8). Rabbitts et al. found preoperative sleep disorders and parental pain catastrophizing (2), and Horn-Hofmann et al. identified preoperative pain-related anxiety as influential in postoperative pain in children (9). The evidence suggests that negative emotional reactions are a critical factor in postoperative pain and can have significant physiological and psychological consequences if not effectively managed (10).
Postoperative acute pain disrupts various bodily systems, triggering a cascade of physiological events, such as increased postoperative pain, the development of chronic and enduring pain, and psychological events, such as restlessness, fatigue, difficulty concentrating, irritability, disturbed sleep, and maladaptive behaviors (11). These complications prolong the recovery and wound-healing process, increase the length of hospital stays and associated costs, and reduce patient satisfaction (12). Therefore, identifying predictors of preoperative pain can assist the healthcare team in effectively managing postoperative pain.
2. Objectives
The aim of this study was to investigate the relationship between psychological variables and postoperative pain in children.
3. Methods
This study was conducted following a descriptive-correlational study design. The study determined psychological variables related to postoperative pain in children aged 6 - 13 years hospitalized in the selected children’s hospital in Tehran, Iran. Samples were selected conveniently from the children hospitalized for elective surgery. The number of samples was calculated by considering the average effect size of 0.3 and the chi-square test statistic.
With α = 0.05 and the probability type II error β = 0.1, the number of required samples was 171 subjects.
The inclusion criteria encompassed children who met the following conditions: Admission solely for surgery, ages between 6 and 13 years, absence of physical or mental disorders according to records and parental statements, and placement in surgeon services utilizing the same pain management protocol. The exclusion criteria included the occurrence of a stressful incident during the study, a child becoming unwell to the extent of necessitating life-saving measures, and incomplete questionnaire responses. Initially, 200 children were considered for the study; however, ultimately, 171 children were selected based on the specified inclusion and exclusion criteria.
The utilized tools included four questionnaires. The demographic characteristics questionnaire comprised two parts, one relating to parental characteristics (e.g., age, gender, occupation, family monthly income, and educational level) and the other to child characteristics (e.g., age, gender, type of surgery, surgery duration, and prior pain experience). Pain severity was evaluated using the Numerical Rating Scale (NRS) (ranging from 0 = no pain to 10 = most severe pain). Consistent with previous studies, moderate to severe pain was defined as a score equal to or greater than 4 (13). The Numerical Rating Scale is a recognized method for assessing the severity of acute postoperative pain, with its validity and reliability validated in various studies (14).
The Child Pain Anxiety Symptoms Scale (CPASS) was designed for individuals aged 6 to 18 years, consisting of 20 items rated on a 6-point Likert scale ranging from 0 (never) to 5 (always). The total score ranges from 0 to 100, with higher scores indicating greater pain anxiety. The questionnaire’s validity and reliability have been established through various studies (15).
The Spielberger’s State-Trait Anxiety Inventory (STAI) comprises 2 components: The state component, which consists of 20 items expressing state anxiety that characterizes an individual's feelings at the moment of response, and the trait component, which measures a more enduring disposition to anxiety. The trait component comprises 20 items that assess trait anxiety, representing individuals’ general feelings. Each item is rated on a 4-point Likert scale, ranging from 1 (almost never) to 4 (almost always). Scores for each part range from 20 to 80, with higher scores indicating greater anxiety. The Persian version of this tool has been utilized in previous studies, confirming its validity and reliability (16).
The Coping Strategies Questionnaire (CSQ) encompasses 50 items designed for patients to self-assess cognitive and behavioral strategies for coping with pain. The questionnaire includes 2 dimensions: Cognitive strategies with 6 subscales, including ignoring pain sensations, reinterpreting pain sensations, diverting attention, coping self-statements, catastrophizing, and praying or hoping, and behavioral strategies with two subscales, encompassing increasing activity level and increasing pain behavior. Additionally, there are two items at the end of the questionnaire to evaluate the effectiveness of pain control and the ability to reduce pain. Responses are rated on a 7-point Likert scale, ranging from 0 (never do) to 6 (always do). The total score ranges from 0 to 300, with higher scores indicating enhanced pain coping. The instrument exhibits satisfactory reliability and validity (17).
Face validity and content validity were evaluated to assess the validity of the instruments in this study. Ten faculty members from Shahid Beheshti University of Medical Sciences, Tehran, Iran, reviewed the tools for relevance and simplicity, with necessary modifications made. Face validity was further assessed by distributing the tools to 10 children and their parents to evaluate item simplicity and comprehensibility. Following the collection of feedback and appropriate adjustments, the final versions were approved. In this study, internal consistency reliability and stability were employed to assess instrument reliability; nevertheless, the inter-observer correlation coefficient was used to assess the visual analog scale (VAS) (Table 1).
| Tools | Cronbach’s Alpha | ICC |
|---|---|---|
| CSQ | 0.95 | 0.95 |
| CPASS | 0.91 | 0.92 |
| STAI | 0.94 | 0.93 |
Abbreviations: CSQ, Coping Strategies Questionnaire; CPASS, Child Pain Anxiety Symptoms Scale; STAI, Spielberger’s State-Trait Anxiety Inventory; ICC, intraclass correlation coefficient.
Data collection was carried out by the researcher after obtaining ethical approval (IR.SBMU.PHARMACY.REC.1399.215). The samples were collected based on the inclusion criteria, then they were completed consent form and this process spanned approximately 3 months.
Data analysis was conducted using SPSS software (version 21). Initially, the variables were described in terms of frequency and mean. Subsequently, the correlation between independent and dependent variables was determined, and variables significant at a level less than 0.05 were subjected to linear regression analysis.
4. Results
In the study, a total of 171 children who met the inclusion criteria participated. Among these participants, 112 (65.5%) and 59 (34.5%) were male and female, respectively, with an average age of 9.58 years. The most common type of surgery was abdominal surgery, accounting for 91 cases (53.2%), followed by genitourinary surgery in 51 cases (29.8%) and other surgeries in 29 cases (17%). The average duration of surgeries was 134.29 minutes. A total of 87 children (50.8%) reported experiencing preoperative pain, with 38 of them (22.2%) describing it as moderate and 31 (18.1%) as severe; however, the remaining cases reported mild pain.
The mothers participating in the study had a mean age of 34.3 years, with the majority being housewives (80.1%) and having a bachelor’s degree (45%). On the other hand, the fathers had an average age of 39.6 years, with the majority being self-employed (48.5%) and having an educational level below a high school diploma (76%) (Table 2).
| Variables | No. (%) or Mean ± Standard Deviation |
|---|---|
| Child’s age (y) | 8.58 ± 2.233 |
| Gender | |
| Female | 59 (34.5) |
| Male | 112 (65.5) |
| Type of surgery | |
| Abdominal | 91 (53.2) |
| Genitourinary urine | 51 (29.8) |
| Other surgeries | 29 (17) |
| Experience of pain | |
| Mild | 102 (59.7) |
| Medium | 38 (22.2) |
| Severe | 31 (18.1) |
| Duration of surgery (min) | 134.29 ± 68.58 |
| Mother’s age | 34.38 ± 6.663 |
| Father’s age | 39.63 ± 6.342 |
| Mother’s job | |
| Housewife | 137 (80.11) |
| Manual worker | 7 (4.09) |
| Employee | 16 (9.36) |
| Freelance job | 11 (6.44) |
| Father’s job | |
| Unemployed | 8 (4.67) |
| Manual worker | 54 (31.5) |
| Employee | 26 (15.21) |
| Freelance job | 83 (48.54) |
| Mother’s education | |
| Illiterate | 9 (5.26) |
| High school | 55 (32.16) |
| Diploma | 30 (17.58) |
| Bachelor | 77 (45) |
| Father’s education | |
| Illiterate | 16 (9.35) |
| High school | 65 (38.02) |
| Diploma | 65 (38.02) |
| Bachelor | 25 (14.61) |
| Child Pain Anxiety Symptoms Scale | 53.66 ± 21.284 |
| Spielberger’s State-Trait Anxiety Inventory | |
| Manifest | 47.85 ± 15.11 |
| Latent | 30.15 ± 12.43 |
| Coping Strategies Questionnaire | |
| Cognitive | 127 ± 14.93 |
| Behavioral | 84.30 ± 18.54 |
Table 2 shows information on the mean preoperative anxiety levels, with children having a mean preoperative anxiety score of 53.66 ± 21.28 and parents exhibiting state and trait anxiety scores of 47.85 ± 14.15 and 30.15 ± 12.43, respectively. Additionally, the mean scores for cognitive and behavioral coping strategies in children were 127 ± 14.93 and 84.30 ± 18.54, respectively.
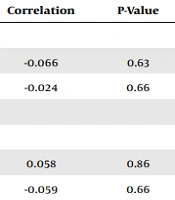
The analysis of Table 3 revealed no significant correlations between demographic factors such as age, gender, type of surgery, and preoperative pain with postoperative pain. However, Table 4 shows correlations between child anxiety, parent anxiety, and child coping mechanisms with acute postoperative pain. Specifically, for each point increase in the mean anxiety score of children and parents, there was a corresponding 0.31% and 0.30% increase in postoperative pain, respectively. Conversely, for each point increase in the mean coping score of children, there was a 0.14% decrease in postoperative pain. The odds ratio (OR) was 0.47, with a 95% confidence interval (CI) of 0.023, and the P-value was 0.001.
| Variables | Correlation | P-Value |
|---|---|---|
| Demographics variables | ||
| Age | -0.066 | 0.63 |
| Gender (male) | -0.024 | 0.66 |
| Physiological variables | ||
| Type of surgery | ||
| Abdominal | 0.058 | 0.86 |
| Genitourinary urine | -0.059 | 0.66 |
| Facial and skull | -0.003 | 0.70 |
| Orthopedic | 0.021 | 0.69 |
| History of surgery | 0.124 | 0.03 |
| Model | Unstandardized Coefficients | Standardized Coefficients, Beta | t | Sig. | F | r2 | |
|---|---|---|---|---|---|---|---|
| B | Standard Error | ||||||
| Constant | 3.489 | 1.014 | 3.442 | 0.001 | 18.215 | 0.28 | |
| Child Pain Anxiety Symptoms Scale | 0.009 | 0.002 | 0.311 | 4.271 | 0.000 | ||
| Spielberger’s State-Trait Anxiety Inventory | 0.040 | 0.009 | 0.311 | 4.271 | 0.000 | ||
| Coping Strategies Questionnaire | -0.047 | 0.023 | -0.147 | -2.082 | 0.039 | ||
5. Discussion
The aim of this study was to determine the psychological variables related to postoperative pain in children hospitalized at the selected children’s hospital in Tehran. The results of the present study revealed that most children experienced moderate to severe postoperative pain, and those children and their parents with higher anxiety levels were more likely to experience postoperative pain; nevertheless, children with higher coping abilities were less likely to experience postoperative pain.
Postoperative pain is a common complication in children (2, 18), influenced by various factors, including mental status (19). The results of this study demonstrated that children with high levels of preoperative anxiety reported experiencing more postoperative pain. Similarly, several previous studies have shown that child anxiety is a potential contributor to postoperative pain (2, 20), affecting both acute (21-23) and chronic (20) postoperative pain. Therefore, it can be stated that preoperative anxiety, as a psychological factor, can trigger a cascade of physiological events, including increased postoperative pain, depression, and prolonged opioid use (7). These findings align with the results of the present study.
Pain anxiety, representing cognitive, emotional, behavioral, and physiological responses in predicting or experiencing pain, significantly predicts postoperative acute pain (9). Therefore, pain anxiety, as a psychological component, is projected to be a predictor of postoperative pain in children.
Furthermore, postoperative pain is not only influenced by child anxiety; the evidence has shown that parent anxiety and postoperative pain are also positively correlated. Parents with high levels of anxiety tend to report more pain in their children (1, 24, 25). The results of the present study further confirmed that parental anxiety serves as a predictor of postoperative pain in children.
Based on the evidence, parental anxiety might manifest in two types: state anxiety or trait anxiety. Anxiety is a temporary emotional state characterized by tension, conflict, and a sense of losing control of the situation (26). In the present study, the parents predominantly exhibited state anxiety, reporting feelings such as anger, nervousness, fear, hesitation, restlessness, and unrest. These findings are consistent with numerous studies indicating that parental anxiety tends to be of the state anxiety type, particularly when a procedure or painful event occurs involving the child (26). In clinical settings, the majority of children are accompanied by caregivers who can directly or indirectly influence anxiety and pain levels. Children often mirror the emotional regulation demonstrated by their parents or caregivers, affecting their own emotional and physiological responses (6). In a similar vein, Frank et al. (27) demonstrated that 53% of the variation in child distress during immunization was related to parenting behavior.
In addition to the above-mentioned factors, coping is another psychological variable that plays a role in pain management as a coping mechanism. The results of this study indicated that most children had lower coping scores, and those with high coping strategies were less likely to experience postoperative pain. These findings are consistent with previous studies that have also confirmed this correlation (28, 29).
Various emotional and psychological factors can influence a child’s perception of pain and trigger their response (27). Therefore, it is essential to prioritize pain management, particularly during acute painful procedures (30).
A good pain assessment is an initial step in preventing or early detecting pain, leading to effective pain management. Several factors must be considered, such as the assessment skills of the medical staff, changes in children’s age and gender, their level of development and communication abilities, their individual personalities and moods, their unique clinical conditions, personal responses to painful stimuli, and the presence of the patient’s parents, caregivers, or relatives (27). Additionally, trained children showed better engagement in breathing techniques, resulting in significantly lower distress levels in this group (31).
The results of the study on children’s coping behaviors in both cognitive and behavioral dimensions revealed that the highest scores were related to pain assessment and an increase in pain behaviors. This could explain the lower level of coping strategies in children. Since surgery is an unforeseen event in children, it is challenging to develop a coping strategy for this condition, and a low level of adaptation seems reasonable.
5.1. Conclusions
The research findings indicate that most children experience moderate to severe postoperative pain. Child anxiety and parental anxiety are positive predictors of postoperative pain; nevertheless, coping strategies are negative predictors of postoperative pain. Therefore, identifying children at risk and providing psychological interventions can be effective in managing postoperative pain in children and improving their comfort.
One limitation of this study is the small sample size, which limits the generalizability of the results. Therefore, further studies in larger populations are recommended. Additionally, it is suggested to explore the relationship between other psychological variables and child pain beyond those measured in this study.
The authors note that several modalities are used to decrease postoperative pain in children. The improper management of postoperative pain not only increases the morbidity of infants but is also unethical. Guidelines can provide a way to reduce postoperative pain. These guidelines can help pediatric surgeons properly manage postoperative pain, as has been described in guidelines for antibiotic use in various infectious diseases.