1. Background
Cancer is one of the most serious challenges for children’s health (1), and leukemia is one of the most common types of cancer in children and adolescents under 20 years of age (2). The main treatment for leukemia in children is multidrug chemotherapy (3) which is an invasive method that causes many physical side effects (4). Nausea and vomiting are considered among the most common and uncomfortable side effects caused by chemotherapy in children (5). It is estimated that nausea and vomiting occur in 70% of children undergoing chemotherapy (6).
Despite the use of pharmaceutical treatments to reduce nausea and vomiting and the efforts made to control these side effects, no desired outcome has yet been achieved, and up to 60% of patients still report nausea (7). Therefore, the use of non-pharmacological techniques in the form of integrative oncology (IO) has also been recommended in numerous studies (8, 9). During the last two decades, complementary/integrative medicine has been increasingly integrated into supportive and palliative care (10) which is called IO that is a patient-centered approach to cancer care, including changes in lifestyle, mind-body practices, nutrition, and natural products that are used with conventional cancer treatments (11).
One of the non-pharmaceutical methods is overshadowing. This phenomenon was observed for the first time by Pavlov in 1927 (as cited by Geiger and Wolfgram). He stated that the effect of combined stimuli is almost always equal to the stronger stimulus. Therefore, the weaker stimulus is overshadowed by the stronger stimulus, and its strength is limited (12). In generalizing this model to chemotherapy processes, providing a stimulus during drug injection might reduce the effects of other stimuli (e.g., the presence of nurses, personnel gowns, chemotherapy equipment, and devices) on causing nausea and vomiting. The conditioned response caused by drug injection and other stimuli is weakened through this phenomenon, and this weakening prevents nausea and vomiting. It also seems that taste is more related to the stimuli that cause nausea and vomiting and can act stronger and more prominently than other sensory stimuli (12).
Due to the effectiveness of gustatory stimuli in being associated with an unconditioned stimulus that causes gastric upset, tastes were taken as overshadowing conditioned stimuli (13). Since the implementation of overshadowing in the hospital’s daily routine requires ease of use and compliance with high hygienic standards for children in the oncology ward, flavored candies can be used (12). Although few studies have addressed the effectiveness of overshadowing, they have confirmed the effectiveness of this technique. Stockhorst et al. showed that overshadowing could reduce symptoms of anticipatory nausea and rotation-induced unconditioned nausea (14). Another study showed that overshadowing reduced the duration of nausea in patients and lengthened the time between the end of the injection and the onset of nausea after treatment (13).
Considering the necessity of managing the symptoms as the basis of palliative care in children and given the general popularity of complementary medicine techniques, the use of non-pharmacological therapies is of high priority for the prevention and control of side effects, such as nausea and vomiting.
2. Objectives
Since a limited number of studies have addressed the effectiveness of overshadowing in reducing and controlling chemotherapy side effects, the present study sought to examine the effect of overshadowing by flavored candies on controlling chemotherapy-induced nausea and vomiting (CINV) in children with leukemia. If the effectiveness of this technique is confirmed, it can be used as a non-pharmacological intervention to reduce nausea and vomiting in children.
3. Methods
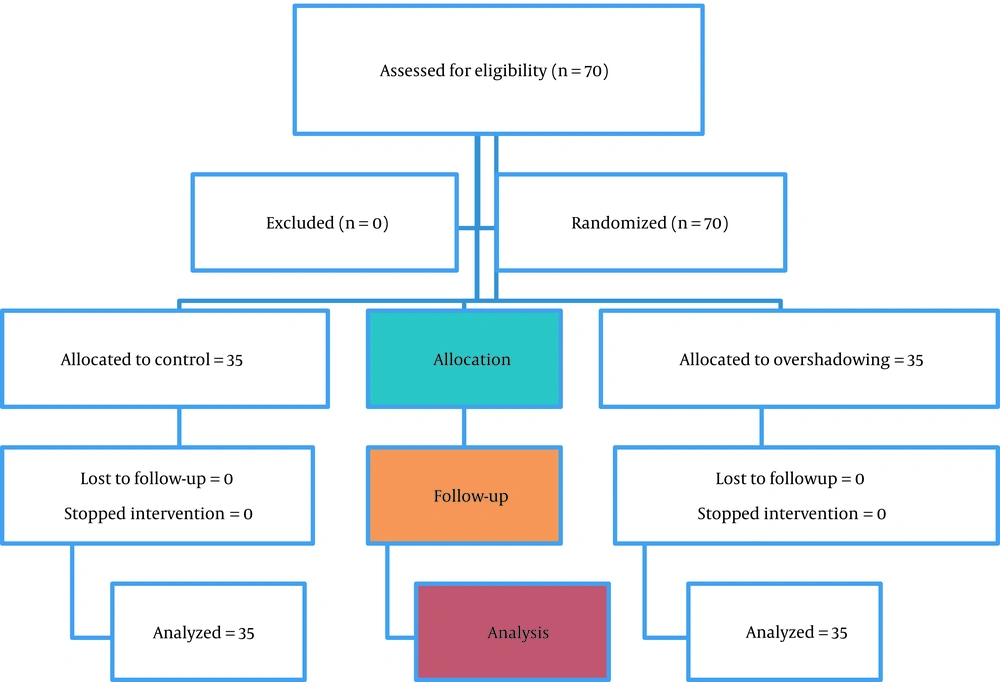
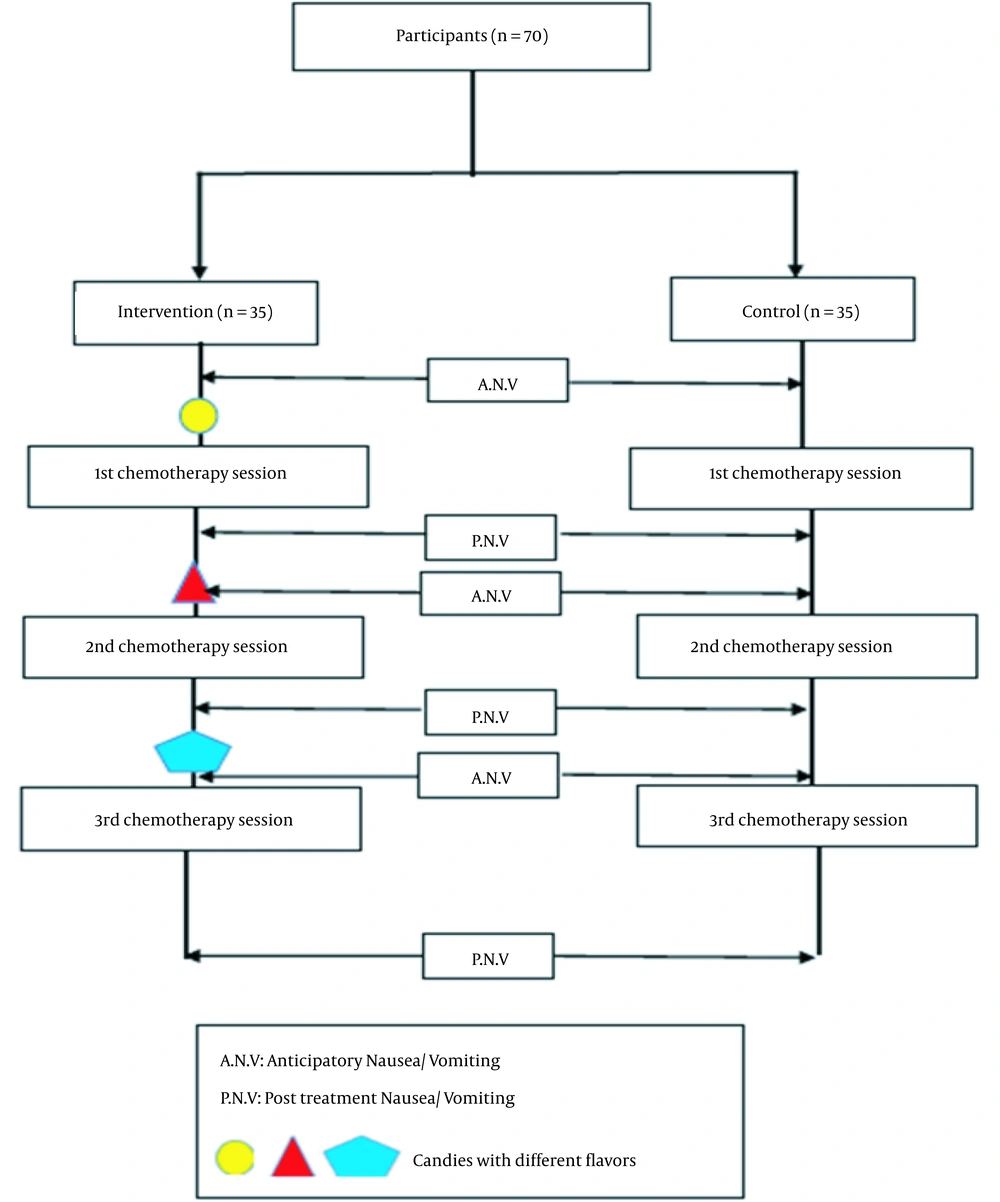
This clinical trial study examined the effect of overshadowing on reducing CINV in children with leukemia in the Oncology Department of Mofid hospital affiliated with Shahid Beheshti University of Medical Sciences, Tehran, Iran, within April 9 to June 27, 2022. The participants were selected using convenience sampling from children with leukemia undergoing chemotherapy. The inclusion criteria were willingness to participate in the study, the completion of a written consent form, the age of 3 - 18 years, the presence of a gag reflex and the ability to swallow, and no metastatic disease to the central nervous system (CNS) or the gastrointestinal tract (to eliminate the organic causes of nausea and vomiting). Impaired consciousness, nothing by mouth (NPO), change of hospitalization, and child death were considered the exclusion criteria. A total of 70 children who met the criteria for enrollment in the study were selected based on the even and odd days of chemotherapy appointments and were randomly assigned to intervention (n = 35) and control (n = 35) groups. Enrolling participants and assigning them to intervention and control groups were performed by a researcher. Following a similar study by Stockhorst et al. (14), the sample size was estimated with 5% accuracy and 80% power using the following formula:
Finally, considering a 25% dropout probability, a total of 70 children were selected as the final sample (35 subjects in each group). Figure 1 shows the sampling procedure.
The data in this study were collected using the child demographic and clinical information questionnaire and the Baxter Animated Retching Faces (BARF) Scale. The child demographic and clinical information questionnaire assessed the information about the child, such as age, gender, duration of the disease, age of diagnosis, and type of leukemia. The outcome measures of this study were the severity of nausea and the frequency of vomiting 10 minutes before the start of chemotherapy and immediately after its completion; accordingly, the severity of nausea was checked through the BARF Scale, and the frequency of vomiting was recorded. The BARF Scale developed by Baxter et al. is a 6-figure scale, with its left (0) and right (15) sides indicating no nausea and the most severe nausea, respectively (15). The reliability of the scale was assessed by calculating the intraclass correlation coefficient (ICC) between 2 raters, and the ICC was equal to 0.87. To measure the frequency of vomiting, a table was designed in which the number of cases of vomiting was recorded.
3.1. Data Collection
Before collecting the data, the researcher provided some information about the research procedure and selected the children who met the inclusion criteria based on the information in their medical records. The selected children were placed into the intervention and control groups. Accordingly, the children admitted to the hospital for chemotherapy on even days were placed into the intervention group (receiving flavored candies). Moreover, those admitted to the hospital for chemotherapy on odd days were assigned to the control group. The sampling continued until the required number of children was selected. Chemotherapy started every day at 10 a.m., and a nurse injected the chemotherapy drugs after taking the child’s venipuncture and injecting the anti-nausea and vomiting medicine.
The children underwent chemotherapy every week. The children in the intervention and control groups received the same standard anti-nausea and vomiting drug, ondansetron 0.15 mg/kg, according to the physician’s order, 5 - 10 minutes before the injection of chemotherapy drugs. The treatment protocol of both groups was the same. First, the severity of nausea was checked through the BARF Scale, and the frequency of vomiting was recorded for the children in both groups 10 minutes before the start of each course of chemotherapy. In addition to the routine care, each child in the intervention group received one flavored candy 10 minutes before the start of chemotherapy. Following Geiger and Wolfgram (12), this process was repeated for 3 chemotherapy rounds. To avoid the possible effects of taste, candies with different flavors (i.e., cherry, orange, and blueberry) were used in each injection. Immediately after the end of each chemotherapy session, the information about the severity of nausea and the frequency of vomiting was recorded for the participants in both groups. No intervention was performed for the patients in the control group. Figure 2 shows the procedure followed in this study.
Finally, the collected data were analyzed with SPSS software (version 25) using descriptive and inferential statistics. The data were described using frequency, percentage, mean, and standard deviation. Moreover, the repeated measures analysis of variance (ANOVA) was run to test the research hypothesis. Finally, to determine the effect of the independent variable on the dependent variables, the t-test, and Pearson’s correlation were used.
3.2. Ethical Considerations
The protocol of this study was approved by the Vice-Chancellor for Research and Technology of Shahid Beheshti University of Medical Sciences (ethics code: IR.SBMU.PHARMACY.REC.1400.131; IRCT code: IRCT20211004052665N1). Verbal and written consent was also obtained from all participants and their parents.
4. Results
Table 1 shows the demographic and clinical characteristics of the participants in the intervention and control groups. All children in the intervention group lived with both parents. Moreover, 8.6% of the children in the control group lived only with their fathers, and the same number of children lived only with their mothers. Fisher’s exact test showed that the 2 groups had a statistically significant difference (P < 0.05) in terms of living with their parents. Therefore, the effect of repeated data was controlled by ANOVA. However, the participants in the 2 groups were homogenous regarding other demographic characteristics, and there was no statistically significant intergroup difference (P > 0.05). This confirms that the participants were distributed similarly in the 2 groups regarding gender, type of leukemia, birth order, age, and duration of leukemia.
| Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Gender | 0.467 | ||
| Female | 16 (45.7) | 13 (37.1) | |
| Male | 19 (54.3) | 22 (62.9) | |
| Type of leukemia | Fisher’s exact test = 0.139; P = 0.183 | ||
| ALL | 32 (91.4) | 28 (80) | |
| AML | 1 (2.9) | 6 (17.1) | |
| Both | 2 (5.7) | 1 (2.9) | |
| Age (y) | 6.75 ± 2.42 | 6.64 ± 2.98 | 0.86 |
| Disease duration (mo) | 7.28 ± 7.47 | 7.65 ± 6.31 | 0.82 |
Abbreviations: SD, standard deviation; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia.
a Values are expressed as No. (%) or mean ± SD.
The statistical results showed that the children in both intervention and control groups experienced more nausea after chemotherapy in the first and second chemotherapy sessions. The Wilcoxon test showed that nausea increased in both groups similarly (P < 0.05). However, the Mann-Whitney U test results showed no statistically significant difference in the severity of nausea between the 2 groups before and after the intervention (P > 0.05). In the third chemotherapy session, the children in the control group experienced more nausea after chemotherapy; nevertheless, the severity of nausea in the children in the intervention group did not show a statistically significant difference. The results of the Wilcoxon test showed that the severity of nausea in the children in the control group significantly increased (P < 0.05). The data from the Mann-Whitney U test indicated no statistically significant difference between the 2 groups in terms of the severity of nausea before the intervention; however, the 2 groups showed significant differences after the intervention (P < 0.05).
Following the data in Table 2, a comparison of the mean scores of nausea and vomiting in the 3 chemotherapy phases between the intervention and control groups using the independent t-test showed no statistically significant difference (P > 0.05). In addition, the repeated measures ANOVA showed that the changes in nausea and vomiting scores before and after the intervention by removing the effects of age, gender, illness duration, and type of leukemia were not statistically significant (P > 0.05).
| Group Time | Control | Intervention | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | df | P-Value | Mean ± SD | df | P-Value | |
| Pre-intervention nausea score | 1.24 ± 0.35 | 52.474 | 0.453 | 1.34 ± 0.65 | 68 | 0.452 |
| Post-intervention nausea score | 2.50 ± 1.15 | 62.467 | 0.120 | 2.12 ± 0.84 | 68 | 0.120 |
| Changes in nausea scores | 1.25 ± 1.13 | 63.390 | 0.053 | 0.78 ± 0.86 | 68 | 0.053 |
| Pre-intervention vomiting score | 0.01 ± 0.11 | 57.649 | 0.185 | 0.06 ± 0.17 | 68 | 0.184 |
| Post-intervention vomiting score | 0.34 ± 0.55 | 67.998 | 0.435 | 0.44 ± 0.55 | 68 | 0.435 |
| Changes in vomiting scores | 0.32 ± 0.50 | 67.971 | 0.643 | 0.38 ± 0.51 | 68 | 0.643 |
Abbreviation: SD, standard deviation.
5. Discussion
Frequent treatment with chemotherapy drugs leads to nausea and vomiting as common side effects of this treatment method (16). The present study examined the effectiveness of overshadowing in controlling CINV in children with leukemia. The present study’s findings indicated that there was not a statistically significant difference in the mean frequency of vomiting between the children undergoing the overshadowing intervention and children in the control group. This showed that the overshadowing technique was not effective in reducing the frequency of vomiting.
Opposite to the present study, Sadat Hoseini examined the effect of music therapy on nausea and vomiting in children with malignancy and found that music reduces the severity of nausea in children but does not affect their vomiting (17). Genc et al. and Zhang et al. found that massage does not affect vomiting (18, 19). However, Byju et al. studied the effectiveness of acupressure on nausea and vomiting in patients undergoing chemotherapy. The results showed significant differences between the control and intervention groups in terms of the frequency of vomiting every 3 days; accordingly, the acupressure group reported the least frequency of vomiting on the third day (8), contrary to the results of the present study. These contradictory findings could be attributed to the non-pharmacological methods used and the type of nausea and vomiting.
The current study investigated the effect of the overshadowing technique on anticipatory nausea and vomiting (ANV) as a subset of CINV, which was not effective. However, the study detailed above addressed the effect of acupressure in controlling CINV. Therefore, their findings are inconsistent with the results of the present study. The data in the present study revealed that the overshadowing technique had no effect on the severity of nausea and frequency of vomiting. Accordingly, it can be argued that constant exposure to drugs and tolerance of chemotherapy agents as behavioral indicators of nausea and vomiting instead of normalization can lead to increased sensitivity (14). Moreover, the participants’ frequent exposure to chemotherapy increased their sensitivity to drugs that could undermine the effect of overshadowing on reducing the severity of nausea and frequency of vomiting.
The results indicated that the severity of nausea increased significantly in the children in both the intervention and control groups after the intervention in the first and second chemotherapy sessions, compared to the severity of nausea before the intervention. Moreover, no reduction was observed in the severity of nausea in the children in the intervention group. This finding is not consistent with the results of a study by Stockhorst et al. that examined the effect of overshadowing on nausea in cancer patients and studies that addressed the effects of overshadowing on conditioned and unconditioned nausea in a rotation paradigm (13, 14, 20). The aforementioned studies reported that the severity of nausea decreased after the intervention for the participants in the intervention group. This inconsistency in the findings could be attributed to differences in the participants and their age groups and differences in the causes of nausea and vomiting, cancer type, and chemotherapy drugs.
In the present study, no statistically significant difference was observed in the severity of nausea between the 2 intervention and control groups before and after the intervention. This finding is contrary to the results of a study by Haddadi et al. that examined the effect of drinking ice-containing plain water on nausea and vomiting during chemotherapy in breast cancer patients (21) and a study by Dadkhah et al. that reported that music therapy with periorbital massage led to a significant improvement in CINV in patients with gastrointestinal cancer undergoing chemotherapy (9). The use of ice-containing plain water causes vascular contraction, and music therapy with periorbital massage affects the CNS and creates a feeling of relaxation in the patient in the very early stages of chemotherapy.
Chemotherapy-induced nausea is affected by several factors, such as gender (female), a history of nausea and vomiting, anxiety, fatigue, low quality of life, chemotherapy drugs, and cancer stage (22). Moreover, whether nausea and vomiting are acute or chronic is also effective in their management because the drugs or interventions used for managing acute nausea and vomiting might not be effective in the management of chronic nausea and vomiting (23). Therefore, future studies should take into account these intervening factors.
The differences in the previous studies that have confirmed the effectiveness of complementary treatments in controlling nausea in cancer patients could account for their contradictory findings, compared to the results of the present study. Since the intervention conducted in the present study was a mental technique and a form of deconditioning, increasing the number of chemotherapy cycles could improve the effectiveness of the intervention and the comparability of the treatment process (12).
Bastani et al. examined the effect of acupressure on CINV among school-age children with acute lymphoblastic leukemia and reported a significant difference in the severity of nausea immediately and 1 hour after implementing the intervention between the 2 groups, with no significant difference occurring 12 hours later. According to Chinese and traditional medicine, which considers the cause of nausea and vomiting to be the disruption of the energy balance in the body, acupressure is a solution to restore this balance (16). In other words, acupressure reduces nausea by activating the sensory receptors and interrupting the signals that trigger nausea and vomiting. It also improves blood circulation in the body’s organs, including the gastrointestinal tract (24). However, overshadowing is a psychological technique used to reduce the effect of stimuli and conditioned responses resulting from them, which requires time to be more effective (12).
The data in the present study revealed that in the third chemotherapy session, the children in the control group experienced more nausea after chemotherapy. However, the severity of nausea in the children in the intervention group did not show a statistically significant difference. Additionally, there was no statistically significant difference between the 2 groups regarding the severity of nausea before the intervention; however, the 2 groups showed significant differences after the intervention. This finding indicates that the overshadowing intervention in the third chemotherapy session was more effective in reducing the amount of nausea in children.
Since the overshadowing technique reduces a person’s response to stimuli by limiting the conditioned response and creating adaptation to repeated nauseating stimuli (14), the frequent implementation of this technique and the child’s adaptation to the stimulus might have led to a decrease in the severity of nausea in the children. Similarly, Stockhorst et al. reported that the reduction of nausea after chemotherapy was delayed and shorter in the overshadowing group. In the aforementioned study, no patient in the experimental group complained about anticipatory nausea. In other words, anticipatory nausea did not occur in the overshadowing group in the third cycle of chemotherapy (13).
Although the changes in the severity of nausea in the 3 chemotherapy phases were not significantly different before and after the intervention between the 2 groups, Goerges showed that overshadowing was effective, and none of the children undergoing chemotherapy in the intervention group suffered from anticipatory nausea (25). Furthermore, Stockhorst et al. reported that the overshadowing intervention during 3 chemotherapy sessions contributed to controlling anticipatory nausea (13). This might be due to the effect of the child’s mental condition and anxiety before chemotherapy, the environmental and cultural factors of the child and their family, and the child-nurse interaction. Mental conditions and anxiety are related to the incidence and severity of vomiting after treatment, and anxiety might enhance the severity of ANV (12).
Environmental characteristics might also affect patients’ capacity to tolerate nausea and lower its threshold. In addition, family conditions can affect the child’s ability to cope with the effects of CINV. For example, children from families who are allowed to speak about their pain and problems experience less anticipatory nausea (26). Another reason for the lack of a significant difference in the severity of nausea was using a self-report tool to measure nausea as a subjective variable. Other studies have used a 7-to-9-item Nausea Severity Scale or objective data of vagus nerve stimulation, such as heart rate. There is always uncertainty over the use of self-report tools to evaluate individual and psychological variables and psychological processes; therefore, a definite outcome cannot be expected from the measurement and interpretation of the data from nausea assessment tools. Moreover, the present study and the studies reviewed above did not focus on prevention behaviors and self-management of nausea and vomiting. Consequently, the frequency and variety of self-care methods, such as drinking fluids, listening to music, controlled/deep breathing, eating small meals, and distraction used by the child or family, are unknown and can affect the research results (27).
Rodriguez argued that the characteristics of clinics, as an external factor, affect the severity of anticipatory nausea, and the conditions of the chemotherapy unit, such as the absence of entertainment devices or comfortable beds and chairs, can increase the manifestation of anticipatory nausea. Feelings of anxiety and depression are also considered internal factors that might lead to variability in the occurrence of nausea (26). The Chemotherapy Department in the present study did not have suitable conditions to provide comfort and relaxation for the children. Moreover, the mental state of the children was not investigated during the intervention. These problems could lead to the exacerbation of CINV and undermine the effects of the intervention.
A review of the literature showed no similar studies on the impact of overshadowing on CINV in children. Therefore, it was not possible to compare the results of the present study to other studies in the literature and draw a definite conclusion about the efficacy of overshadowing in reducing nausea and vomiting in children undergoing chemotherapy. In addition, since the participants in this study were selected using purposive sampling from a teaching hospital affiliated with Shahid Beheshti University of Medical Sciences, the findings of this study have limited generalizability to other groups and populations. Due to the small number of samples, the changes in the vomiting scores were borderline significant. Therefore, there is a need for further research in this field.
5.1. Conclusions
The results of the present study suggested that the severity of nausea in children who were subjected to the overshadowing technique was reduced in the third chemotherapy session, compared to the children who were not subjected to this intervention. However, there was no significant difference in nausea and vomiting by overshadowing using flavored candies between the 2 groups, and this technique did not affect the severity of nausea and the frequency of vomiting in children.