1. Background
Acute poisoning in children (APC) is one of the most common preventable causes of stressful and serious medical emergencies visits (1). Hospitalization rate due to APC is reported as up to 6.4% of children, who were visited at emergency departments (2). However, the true incidence of APC is expected to be greater.
Acute poisoning in children may be presented by different life threatening symptoms and signs that need more careful management and pediatric intensive care unit (PICU) admission (3). Poisoning is reported as the fourth cause of PICU admission in children (4). Unfortunately APC is associated with morbidity and mortality (5, 6). In 2004, more than 45000 deaths in people younger than 20 years old were reported to be due to APC around the world (7).
Furthermore, APC represents a complex interaction between children and their environmental factors. Young age is an important risk factor for APC (8). Most APC occur within the home or around it (9). In spite of intentional poisoning in adults, most APC are unintentional (10). Due to poisonous substances availability, socioeconomic and educational states of parents, parental supervision, and cultural influences, different etiological patterns of APC in various regions were reported (11, 12). Over time, some changes in trends of APC in regions have been reported, as well (13). Thus determining the epidemiologic aspects of poisonous cases and etiologies of APC are important to choose more appropriate preventive strategies for reduction of APC, planning better treatment approaches and improvement of patients’ outcomes.
2. Objectives
This study was conducted at Qods teaching hospital in Qazvin, Iran during three years from September 2009 to September 2012, to determine epidemiological aspects such as demographic characteristics of poisonous cases, poisoning agents, clinical manifestation, and outcome of APC in children younger than 13 years in this region.
3. Methods
This descriptive cross-sectional study was conducted at Qods teaching hospital in Qazvin, Iran from September 2009 to September 2012. Qods teaching hospital is the only referral pediatric hospital in Qazvin Province. All children younger than 13 years old admitted to the pediatric emergency ward with acute poisoning were assessed in this study. Children with bacterial food poisoning and food allergy were excluded. Data were collected from patients´ files. These patients´ data included age, gender, symptoms at admission, time and season of hospitalization, duration of hospitalization, previous medical history, type of poisonous substance, route of exposure with poisonous agents and outcome were extracted from patients’ files using a data registration form.
Poisonous substances were divided two main drugs and non-drugs groups. Symptoms and signs were classified as 1- neurologic (irritability, depressed level of consciousness, ataxia, abnormal movements, apnea, and seizure), 2- respiratory (tachypnea, wheezing, and cough), 3-gastrointestinal (nausea, vomiting, and abdominal pain), 4- skin (flushing, perspiration, and rashes), 5- ocular (miosis, mydriasis, and tearing), and 6- asymptomatic.
4. Results
Of the 16721 children younger than 13 years old, a total of 434 (2.59%) were admitted with acute poisoning to the pediatric emergency ward. Four patients were admitted twice during this period.
Hospitalization due to APC occurred mostly in male cases (274 v/s 160). Male/female ratio was 1.73/1.
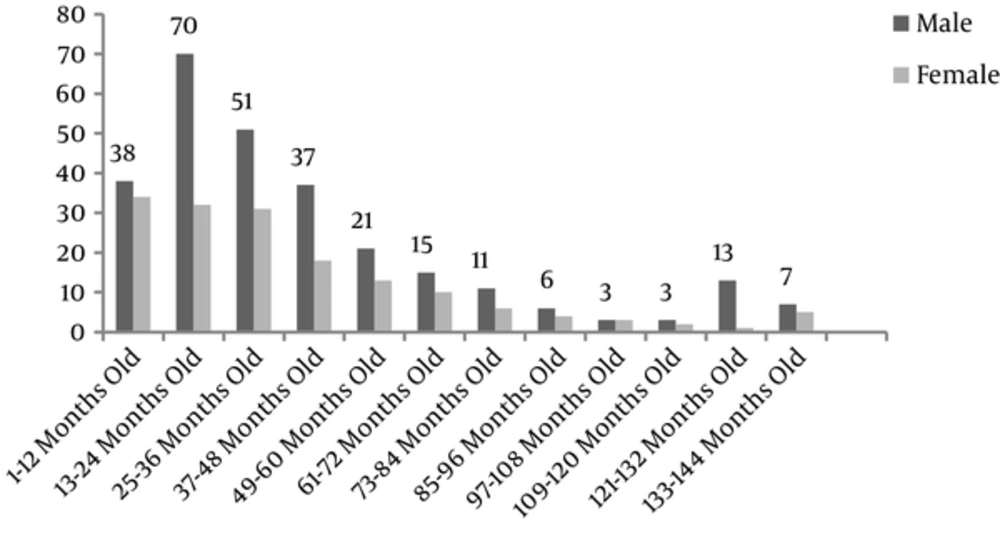
Mean age of hospitalized children was 41 ± 35 months old (45 ± 35 months for boys; 39 ± 33 months for girls). Thirty-one (7.1%) of the patients were under 7 months old (17 males and 14 females). More information about age and gender of hospitalized children with APC is shown in Figure 1.
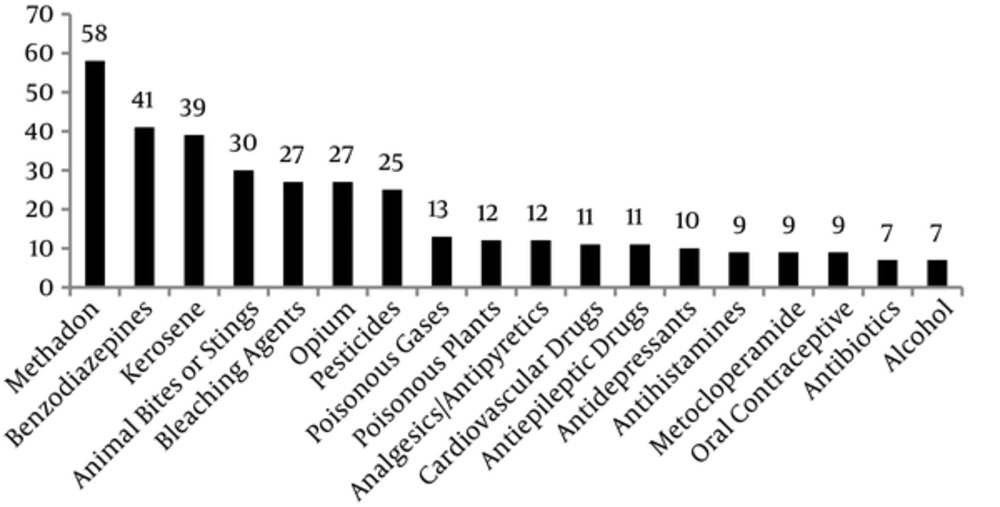
Drug poisoning occurred in 265 (61.05%) cases of APC. Multiple drugs ingestion was responsible for acute poisoning in 19 (4.37%) patients. Non-drug poisoning occurred in 169 (38.94%) cases. The most frequent causes of APC in our study were methadone poisoning in 58 cases (13.4%), benzodiazepines in 41 cases (9.4%), and kerosene in 39 cases (9%). The most frequent poisonous agents of APC are shown in Figure 2.
Neurologic symptoms and signs were the most frequent (256 cases) presentation in the patients. These neurologic symptoms and signs were mental state changes including drowsiness (117 cases), loss of consciousness (56 cases), irritability (36 cases), ataxia (36 cases), and seizure (11 cases). Fifty-three (12.21%) patients with recent positive history of exposure with poisons were admitted to the hospital without overt clinical presentation of poisoning.
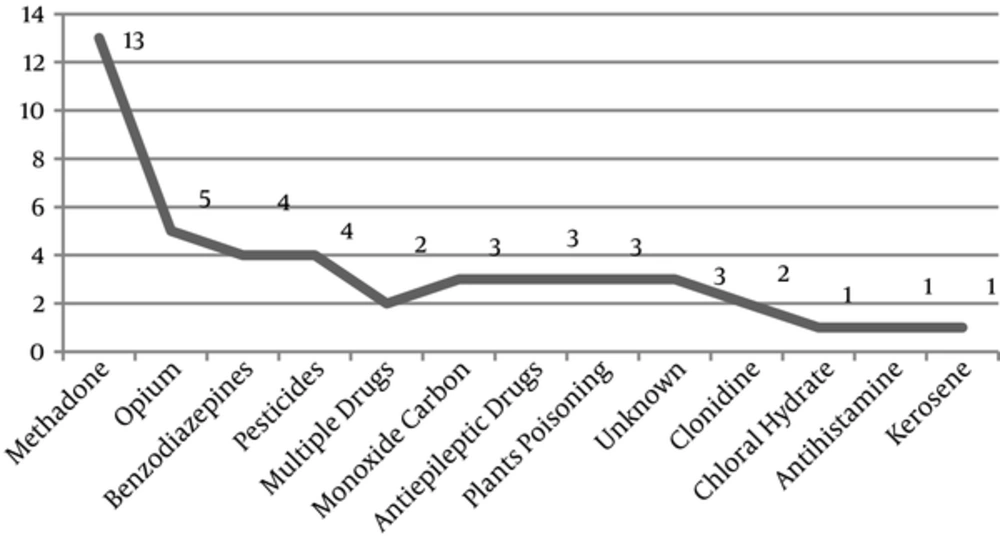
Mean hospital stay was 25 ± 22 hours. Overall, 370 patients (85.25%) were discharged during 48 hours. Forty-five poisoned children were admitted to the PICU. Frequency of poisonous agents in children with acute poisoning admitted to PICU is shown in Figure 3.
The most frequent route of poisoning in 391 (90.09%) cases was ingestion. Other routes of APC were skin injection (animal and insects bites) in 30 (6.91%) cases and respiratory in 13 (2.99%) cases.
Accidental acute poisoning occurred in 431 (99.3%) cases. Intentional poisoning occurred in 3 patients; two male cases due to suicidal attempt with antiepileptic drugs and one female case with aluminum phosphide poisoning as a homicidal action.
Three female (0.69%) cases of APC died during this period. Two female deaths (16 and 30 months old) occurred due to monoxide carbon intoxication. One female death (37 months old) was the result of methadone intoxication.
5. Discussion
Acute poisoning in children is a serious cause of emergency department visits around the world (1). It is a potentially preventable health problem in developed and developing countries; however different poisonous agents are responsible for APC in various regions, at different times. Etiologies of APC are important to choose more appropriate preventive strategies for reduction of poisoning, planning a better treatment approach and improvement of patients’ outcomes. The important findings of this study were lower intentional poisoning rate, lower mortality rate due to APC, and monoxide carbon inhalation as the deadliest route of poisoning and methadone as the leading cause of APC.
Hospitalization due to APC in our study was 2.59%. Similar rate for hospital admission in APC was reported by another study (14). However, the hospital admission rate was 6.3% in a study in Shiraz during 2008 to 2013 that was higher than the present study (2). This difference may be due to greater intentional poisoning (53.3%) of APC in the mentioned study (2).
In our study male/female ratio (257/150) was 1.7/1. The world health organization (WHO) reported higher rate of poisoning in boys than girls in all regions of the world in 2004 report (7). The same male/female ratio (1.5/1) was reported in another study (8). Male predominance in poisoned children less than four years old was also reported (14). This was probably because boys are more active and curious than girls. No difference between the two genders was reported in children with APC less than 15 years old during 1998 to 2008 in Zahedan (1). Haghighat et al. reported female dominancy in APC less than 18 years old, during 2009 in Shiraz (15). In this study 331 of 773 (42.8%) patients were older than 12 years old yet our patients were under 13 years old. Perhaps this difference in age range is responsible for the difference in gender dominancy of the two studies. Ozdemir et al. reported two distinct peak ages in poisoned children, for boys this was between 1 and 5 years old and for girls between 13 and 16 years old (3).
Mean age of poisoning in our study was 41.37 ± 34.9 months old. The majority of 370 (85.2%) poisonings occurred in children less than 6 years old. Different studies reported that most cases of APC occurred in preschool aged children (1, 16).
In our study, 31 (7.1%) cases of APC occurred in infants less than 7 months old. In another study, 35 (4.5%) poisoned infants less than 7 months were reported (15). These infants were not able to move and explore their environments. All poisonous agents were given by their caregivers. One important reason for early infancy poisoning was lack of awareness of parents about keeping poisonous agents in bottles of drugs and keeping unlabeled drugs at home. Caregiver and parental education about keeping drugs and poisonous items in labeled bottles’, use of drugs in proper dosage and awareness about serious injuries of illicit drugs like opium for treatment of cough, gastroenteritis and calming the infants is an essential step to reduce APC in this age group.
In our study, most cases of APC (24.8%) occurred in 13 to 24 months old infants. Similar results were reported by other studies (14). Toddlers have a desire to put different substances including poisonous agents in their mouths and try to explore the world with their mouth. This behavior makes toddlers the most common victims of accidental poisoning in all regions, especially if they do not have adequate supervision of their caregivers.
The least frequency of APC occurred in children 7 to 12 years old (primary school ages). Children in this age range were educated and had more information about their environmental hazards, thus risk of accidental poisoning decreased in this period. Other studies showed APC was less frequent in this age group (1, 13).
Methadone as a drug for opium detoxification was the most common agent for APC in our study. An increasing trend in proportion of methadone poisoning from 2010 to 2013 was reported in Shiraz, as well (2). Opioid was reported as the most important agent for APC in Birjand (6). These findings are warning signs. Benzodiazepines, paracetamol, and tricyclic antidepressant drugs were the most common causes as reported by other studies in other regions (1, 14, 16). Kerosene was the second leading cause of APC in our study. Kerosene as a non-pharmaceutical agent was the most common agent for APC in other studies (12, 17). Kerosene as a fuel in our region has now been substituted by natural gas, but in some houses kerosene was kept in bottles and children drank it accidentally.
In our study, the majority of APC (99.5%) occurred accidentally. Intentional APC in this study was lower than other studies (14, 16). In preadolescence and adolescence period, suicide and intentional poisoning is a serious problem. Perhaps one reason for this difference is lower number of adolescent cases with APC in our study than other studies. Koliou et al. reported that unintentional poisoning was more common in older girls and accidental poisoning more common in younger boys (14).
Neurologic symptoms and signs were the most common presentation of APC in our study. This finding was reported by Sadeghi-Bojd et al. (1), whereas nausea and vomiting as the most common presentation of APC followed by neurologic manifestation were reported in another study (16). Lin et al. reported neurological symptoms as the most common presentations in patients with drug poisoning while alimentary complaints were the most common presentation in non-drug poisoning (18).
Forty-five (10.3%) cases were admitted to the PICU in our study. This rate of PICU admission was more than other studies (15, 18). This difference may be due to younger age of our patients, and more cases with depressed level of consciousness in this study. Most patients with PICU admission were poisoned with drugs; the most frequent drug was methadone. In another study, benzodiazepines were the leading cause of PICU admission (4).
Mortality rate (0.69%) in our study was lower than other studies (15, 17). This decrease in mortality rate in APC cases may be the result of greater parental awareness about poisoning, early recognition of exposure to poisons in children, shorter time for reaching medical centers, improved medical managements and technological advances in the PICU.
Fatality rate for respiratory route of poisoning was higher than other routes of poison exposure in this study. Two deaths occurred in 13 cases of monoxide carbon intoxication. Symptoms of monoxide carbon poisoning are headache, dizziness, weakness, nausea, vomiting, chest pain, and confusion. People, who are sleeping can die from monoxide carbon poisoning before they have symptoms. Poisoning with monoxide carbon, a colorless and odorless gas, was reported as the deadliest non-drug agent poisoning in another study (3). More education about prevention of this type of poisoning is necessary.
There are many potentially life threatening poisonous substances around children. One of the most preventive strategies to decrease APC incidence is educational programs, through public communication devices, for parents and caregivers. Increasing awareness of caregivers about hazards of APC helps them provide safer environments for their children.