1. Background
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic, resulting in a disease named coronavirus disease 2019 (COVID-19), has spread worldwide since the beginning of 2020 (1, 2). The World Health Organization (WHO) declared the COVID-19 outbreak to be a pandemic on March 11. COVID-19 is now regarded as the sixth public health emergency of global concern (3). Egypt was part of the global spread, where on February 14, 2020, there was a record of the first case. By May 1, 2020, there were 5895 confirmed cases in total, with a 6.9% case fatality rate. Similar to other age groups, children were affected; however, the overall incidence was less than 10%. Healthcare professionals represented 11% of all confirmed cases (4).
The SARS-CoV-2 presents with a wide array of presentations in both adults and children (5). The infection passes through three phases, progressing from upper airway affection to viral descent into the alveolar cells, which causes abnormal imaging. The third phase is characterized by a cytokine storm caused by a vigorous immune response. High inflammatory markers and severe interstitial pneumonia are present in this phase (6). However, in children, presentations are milder, with flu-like manifestations (7), followed by a full recovery. Most are treated via outpatient clinics or have an asymptomatic course (8, 9). Serious cases are infrequent, and only a few require hospitalization. The few severe cases frequently had underlying or coexisting medical conditions.
Early reports identified other symptoms in pediatrics, such as gastrointestinal symptoms. Some children with confirmed COVID-19 had no initial respiratory manifestations. Their affection was masked until signs of viral pneumonia were observed in chest computed tomography (CT) scans. The nucleic acid detection for SARS-CoV-2 was then performed, confirming the diagnosis (10, 11). There is limited data on children in the literature; milder symptoms are reported in children compared to adults, and rare deaths in children, and adolescents have been observed.
2. Objectives
The current study’s objective was to report the epidemiological, clinical, radiological, and laboratory findings of a group of suspected COVID-19 children. Consequently, atypical presentations could be emphasized, and better prediction of the disease with the earlier implementation of therapy could achieve better outcomes with fewer possibilities for the spread of infection; for example, respiratory manifestations could be a clue for non-respiratory system affections (e.g., distress due to metabolic acidosis in severe diarrhea).
3. Methods
3.1. Study Design
The present investigation was a cross-sectional and analytical study.
3.2. Study Setting
This study was carried out for patients referred to the Emergency Department of Abu El-Reesh Japanese Hospital, Cairo, Egypt, and managed as inpatients during the third wave, which began in March 2021 and lasted up to the end of October 2021 (12). Owing to the epidemic, the authors prepared a designated area in the Emergency Department for children with suspected COVID-19 manifestations; nevertheless, those with positive nasopharyngeal or oropharyngeal (NP or OP) swabs were managed in isolation zones. All clinical and laboratory data were collected from the 404 children admitted to the emergency department. The criteria for suspected cases were reviewed according to WHO guidelines (13, 14). All children met the diagnostic guidelines established by the Egyptian Ministry of Health (15). The enrolled patients were categorized into four groups based on age, including those within the first 2 years, within 2 - 6, within 6 - 12, and over 12 years. Children in the emergency department with suspected manifestations of COVID-19 were transferred after triaging to the designated zones. Then, reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 was performed from nasopharyngeal swabs. The swabs were collected under strict infection control measures. The samples were collected in specific tubes containing viral transport. Viral ribonucleic acid was then extracted and mixed with commercially available PCR master mix and primers.
3.3. Inclusion Criteria
All children who presented to the emergency department with suspected COVID-19 infection to be confirmed via swabs and/or specific CT changes for COVID-19 infection were included in the study.
3.4. Exclusion Criteria
Children presented to the emergency department without suspicious criteria for COVID-19 infection were excluded from the study.
Respiratory distress and grading were outlined as children with tachypnea, additional working accessory muscles of respiration, additional grunting, and cyanosis categorized as grades 1, 2, 3, and 4, respectively. Additionally, a clinical-respiratory scoring of patients aided in their risk stratification (16, 17). Regarding children who had respiratory manifestations, high-resolution CT chest scans were conducted to confirm COVID-19 infection through the presence of specific features, such as ground-glass opacities with bilateral peripheral distribution (18, 19). Children were considered to have a positive infection when they tested positive for SARS-CoV-2 by RT-PCR, had a sensitivity > 60% (13-15), and/or had a high-resolution chest CT that showed findings specific to COVID-19. When the swabs were negative and/or CT changes were absent, they were considered negative for COVID-19 infection. Tests carried out on the enrolled patients were recorded, such as complete blood count with differential, blood gases, serum albumin, D-dimer, C-reactive protein, erythrocyte sedimentation rate, and bilirubin.
3.5. Ethical Considerations
The present study was carried out according to the principle of Helsinki. The study protocol was revised and approved by the Scientific Committee of the Pediatrics Department at Cairo University, Egypt. The study protocol was approved by the Ethical Committee of the Faculty of Medicine, Cairo University. The ethical approval number is N-100-2021. Informed consent was obtained from the parents or caregivers.
3.6. Statistical Analysis
The data were analyzed using SPSS software (version 25, Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA). Categorical variables were presented as frequency counts and percentages. Nevertheless, numerical variables were described as median and interquartile range, with minimum and maximum. The chi-square (χ2) test was used to determine associations between categorical variables. Fisher’s exact test was used instead when the expected frequency was less than 5. The p-value was two-tailed and set as significant at the 0.05 level.
4. Results
This study enrolled 404 children suspected of COVID-19 infection, with 58 confirmed cases in the total enrollment. Table 1 shows the demographic characteristics of all included children. Male subjects represented the greater proportion of the study participants (n = 230/404, or 56.9% of the study participants). Unexpectedly, non-respiratory manifestations occupied the upper hand. It represented 62.9% (n = 254) of the total presentations of the enrolled children. Among the non-respiratory manifestations, gastrointestinal ones were predominant (n = 63). Tables 1 and 2 show the most commonly affected systems and their presentations. Table 2 shows the causes of admission among the enrolled children. Respiratory distress was the most common cause of admission in the study participants, followed by diarrhea. It is important to note that although distress was the most common cause, it did not mean that this category had respiratory system affections. In other words, respiratory manifestations could be a clue for non-respiratory system affections (e.g., distress due to metabolic acidosis). Table 3 shows the manifestations and causes of admissions. Note that the same presenting manifestation can be for more than one system affection. Positive COVID-19 cases were 58 out of a total of 404 subjects (14%), with higher male predominance (Table 4).
| Demographic Characteristics | Values |
|---|---|
| Age group (y) | |
| < 2 | 207 (51.2) |
| 2 ≤ 6 | 104 (25.7) |
| 6 ≤ 12 | 75 (18.6) |
| ≥ 12 | 18 (4.5) |
| Median (IQR) | 1.6 (0.4 - 5.0) |
| Minimum-maximum | 0.1 - 13.0 |
| Gender | |
| Male | 230 (56.9) |
| Female | 174 (43.1) |
| Total | 404 (100.0) |
Abbreviation: IQR, interquartile range.
a Values are expressed as No. (%) unless otherwise indicated
| Cause of Admission | No. (%) |
|---|---|
| Respiratory distress | 155 (38.4) |
| Dehydration | 34 (8.4) |
| Heart failure | 31 (7.7) |
| Hemodynamic instability | 24 (5.9) |
| Newly diagnosed diabetic ketoacidosis | 20 (5) |
| Nephrotic syndrome | 14 (3.5) |
| Appendicitis | 13 (3.2) |
| Encephalitis | 13 (3.2) |
| Renal failure | 13 (3.2) |
| Febrile convulsions | 12 (3) |
| Intestinal obstruction | 9 (2.2) |
| Hepatic encephalopathy | 7 (1.7) |
| Guillain-Barré syndrome | 5 (1.2) |
| Kawasaki disease | 5 (1.2) |
| Intussusception | 4 (1) |
| Immune thrombocytopenia | 4 (1) |
| Aplastic anemia | 3 (0.7) |
| Bicytopenia | 3 (0.7) |
| Hypertensive encephalopathy | 3 (0.7) |
| Hypocalcemia convulsions | 3 (0.7) |
| Pancytopenia | 3 (0.7) |
| Uremic encephalopathy | 3 (0.7) |
| Deep vein thrombosis | 2 (0.5) |
| Pericardial effusion | 2 (0.5) |
| Sickle cell crisis | 2 (0.5) |
| Acute peritonitis | 1 (0.2) |
| Aspiration pneumonia | 1 (0.2) |
| Decompensated anemia | 1 (0.2) |
| Dermatomyositis | 1 (0.2) |
| Hypertensive emergency | 1 (0.2) |
| Hypoglycemic convulsions | 1 (0.2) |
| Intracerebral hemorrhage | 1 (0.2) |
| Infected hydrocephalic shunt | 1 (0.2) |
| Liver failure | 1 (0.2) |
| Obstructive uropathy | 1 (0.2) |
| Pleural effusion | 1 (0.2) |
| Poststreptococcal glomerulonephritis | 1 (0.2) |
| Stroke | 1 (0.2) |
| Suspected barter syndrome | 1 (0.2) |
| Suspected Stevens-Johnson syndrome | 1 (0.2) |
| Suspected viral myocarditis | 1 (0.2) |
| Supraventricular tachycardia | 1 (0.2) |
| Total | 404 (100) |
| Presenting Manifestation | No. (%) | Cause of Admission | No. (%) |
|---|---|---|---|
| Respiratory system affection (n = 150) | |||
| RD grade 1 | 4 (2.7) | RD | 147 (98.0) |
| RD grade 2 | 49 (32.7) | Heart failure | 2 (1.3) |
| RD grade 3 | 71 (47.3) | Hemodynamic instability | 1 (0.7) |
| RD grade 4 | 23 (15.3) | ||
| Shock | 3 (2.0) | ||
| Non-respiratory System Affection | |||
| Gastrointestinal (n = 63) | |||
| Diarrhea | 34 (54.0) | Dehydration | 34 (54.0) |
| Acute abdomen | 26 (41.3) | Appendicitis | 13 (20.6) |
| Gastrointestinal bleeding | 1 (1.6) | Intestinal obstruction | 9 (14.3) |
| Perforated viscus | 1 (1.6) | Intussusception | 4 (6.3) |
| Shock | 1 (1.6) | Hemodynamic instability | 2 (3.2) |
| Acute peritonitis | 1 (1.6) | ||
| Cardiac (n = 51) | |||
| RD | 39 (76.4) | Heart failure | 29 (56.9) |
| Shock | 8 (15.7) | Hemodynamic instability | 8 (15.7) |
| Skin rash | 3 (5.9) | RD | 7 (13.7) |
| Convulsions | 1 (2.0) | Kawasaki disease | 3 (5.9) |
| Pericardial effusion | 1 (2.0) | ||
| Hypertensive emergency | 1 (2.0) | ||
| Viral myocarditis | 1 (2.0) | ||
| Supraventricular tachycardia | 1 (2.0) | ||
| Neurological (n = 41) | |||
| Convulsions | 19 (46.3) | Febrile convulsions | 12 (29.3) |
| Disturbed consciousness level | 15 (36.6) | Encephalitis | 13 (31.7) |
| Acute flaccid paralysis | 5 (12.2) | Guillain-Barré syndrome | 5 (12.2) |
| Bulbar palsy | 1 (2.4) | Hypertensive encephalopathy | 3 (7.3) |
| Hemiplegia | 1 (2.4) | Hypocalcemia convulsions | 3 (7.3) |
| Aspiration pneumonia | 1 (2.4) | ||
| Hypertensive emergency | 1 (2.4) | ||
| Intracerebral hemorrhage | 1 (2.4) | ||
| Infected hydrocephalic shunt | 1 (2.4) | ||
| Stroke | 1 (2.4) | ||
| Renal (n = 39) | |||
| Oliguria | 18 (46.2) | Nephrotic syndrome | 14 (35.9) |
| Generalized edema | 14 (35.9) | Renal failure | 13 (33.3) |
| Convulsions | 4 (10.3) | Uremic encephalopathy | 3 (7.7) |
| Disturbed consciousness level | 2 (5.1) | Hypertensive encephalopathy | 2 (5.1) |
| Hematuria | 1 (2.6) | Hemodynamic instability | 2 (5.1) |
| Obstructive uropathy | 1 (2.6) | ||
| Pericardial effusion | 1 (2.6) | ||
| Pleural effusion | 1 (2.6) | ||
| Poststreptococcal glomerulonephritis | 1 (2.6) | ||
| Suspected barter syndrome | 1 (2.6) | ||
| Endocrinal (n = 21) | |||
| RD | 12 (57.1) | Hypoglycemic convulsions | 1 (4.8) |
| Acute abdomen | 8 (38.1) | Newly diagnosed diabetic ketoacidosis | 20 (95.2) |
| Convulsions | 1 (4.8) | ||
| Hematologic (n = 18) | |||
| Purpura | 13 (72.2) | Immune thrombocytopenic purpura | 4 (22.2) |
| Acute limb painful swelling | 2 (11.1) | Aplastic anemia | 3 (16.7) |
| RD | 1 (5.6) | Bicytopenia | 3 (16.7) |
| Severe anemia | 1 (5.6) | Pancytopenia | 3 (16.7) |
| Acute chest syndrome | 1 (5.6) | Sickle cell crisis | 2 (11.1) |
| Deep venous thrombosis | 2 (11.1) | ||
| Decompensated anemia | 1 (5.6) | ||
| Hepatologic (n = 12) | |||
| Disturbed consciousness level | 7 (58.3) | Hepatic encephalopathy | 7 (58.3) |
| Shock | 4 (33.3) | Hemodynamic instability | 3 (25.0) |
| Generalized edema | 1 (8.3) | Liver failure | 1 (8.3) |
| RD | 1 (8.3) | ||
| Multi-organ system failure (n = 8) | |||
| Shock | 8 (100.0) | Hemodynamic instability | 8 (100.0) |
| Rheumatologic (n = 5) | |||
| Skin rash | 4 (80.0) | Kawasaki disease | 3 (60.0) |
| Dysphagia | 1 (20.0) | Dermatomyositis | 1 (20.0) |
| Stevens-Johnson syndrome | 1 (20.0) | ||
| Neuro-metabolic (n = 1) | |||
| Disturbed consciousness level | 1 (100.0) | Encephalitis | 1 (100.0) |
Abbreviation: RD, respiratory distress.
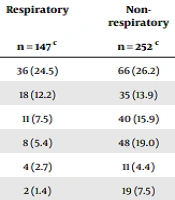
Thrombocytopenia, leucopenia, and pancytopenia were significantly higher in children with non-respiratory manifestations than in those with respiratory manifestations, as shown in Table 5.
a Values are expressed as No. (%)
b P-value is significant if < 0.05.
c The remaining cases (total sample size = 404, respiratory = 150, non-respiratory = 254) had missing data.
Blood pH analysis was significantly different among patients who presented with respiratory system affection and those patients who presented with non-respiratory system affection (P < 0.001). Post-hoc pairwise comparisons with Bonferroni adjustment showed that patients with respiratory system affection had a higher proportion of blood pH abnormalities (68.1%) than patients presenting with other systems affection (44.9%) (P < 0.001). Respiratory acidosis was significantly higher in patients with respiratory system presentation (51.9%) than in patients with non-respiratory system presentation (6.9%) (P < 0.001). However, the proportion of patients with metabolic acidosis was significantly higher in patients presenting with non-respiratory system affection (28.7%) versus (2.2%) patients with respiratory system affection with a P-value of < 0.001 (Table 6).
a Values are expressed as No. (%).
b P-value is significant if < 0.05.
c The remaining cases (total sample size = 404, respiratory = 150, non-respiratory = 254) had missing data.
Other laboratory findings included hypoalbuminemia and elevated D-dimer, which were significantly higher in groups with non-respiratory manifestations (Table 7).
| Laboratory Findings | Respiratory | Non-respiratoryn | P-Value b |
|---|---|---|---|
| No. | 135 c | 216 c | |
| Elevated C-reactive protein | 2 (1.5) | 4 (1.9) | 1.0 |
| Elevated erythrocytic sedimentation rate | 0 (0.0) | 3 (1.4) | 0.288 |
| Elevated D-dimer | 0 (0.0) | 16 (7.4) | 0.001 |
| Elevated kidney functions tests | 1 (0.7) | 3 (1.4) | 0.662 |
| Hypoalbuminemia | 0 (0.0) | 27 (12.5) | < 0.001 |
| Hyperbilirubinemia | 0 (0.0) | 8 (3.7) | 0.026 |
| Proteinuria | 0 (0.0) | 5 (2.3) | 0.161 |
a Values are expressed as No. (%).
b P-value is significant if < 0.05.
c The remaining cases (total sample size = 404, respiratory = 150, non-respiratory = 254) had missing data.
5. Discussion
The present study sought to identify the characteristic demographic, clinical, and laboratory features of SARS-CoV-2 infection in pediatrics. Although the most common cause of admission was respiratory distress, the most common presentations were non-respiratory; however, gastrointestinal affection predominated. It was shown that suspected SARS-CoV-2 infection in pediatrics presents mainly with non-respiratory manifestations. This finding is in line with the findings of previous studies reviewed by AlSamman et al., who concluded that although SARS-CoV-2 infection usually presents primarily with respiratory manifestations, the extra-pulmonary or non-respiratory manifestations of the virus are unexpected and varied. Therefore, better understanding and awareness of these manifestations can result in a more efficient diagnosis, rapid treatment, isolation, and a decrease in the spread of the disease (20).
The present study revealed that gastrointestinal manifestations were the presenting clinical picture in a considerable number of the enrolled children. This finding is in line with a previous report that demonstrated that nearly a quarter of pediatric patients with SARS-CoV-2 infection have gastrointestinal symptoms. It is essential for clinicians to be aware of the gastrointestinal manifestations of SARS-CoV-2 infection (21). Clinicians should also be aware that thrombocytopenia might appear in both mild and severe COVID-19 infections at any time during the course and can be linked to a higher bleeding risk; therefore, its diagnosis might be critical.
Xu et al. suggested three mechanisms by which thrombocytopenia could occur in COVID-19. The first mechanism is increased consumption of platelets, mainly due to lung injury, which generates microthrombi in the circulation and thus increases their consumption. The second mechanism is a decline in platelet production by the medullary invasion of the virus, inhibiting hematopoiesis, and by the reduction of hematopoietic precursors secondary to the cytokine storm. The third mechanism is increased platelet destruction due to autoantibodies and immune complexes (22, 23). The current study revealed that thrombocytopenia was more common in children presenting with non-respiratory manifestations. This might be attributed to the atypical nature of presentations in children due to different immune responses from adults.
Notably, hypoalbuminemia leads to undesirable outcomes in infectious diseases. This could be due to the fact that it is considered a negative acute-phase reactant and could be associated with inflammatory reactions in various infections (24). Hypoalbuminemia was significantly higher in children with non-respiratory manifestations. This finding is nearly similar to a previous study where reduced serum albumin in mild/moderate COVID-19 pediatric cases was observed. It has been postulated that the serum albumin level could point out children with a higher liability of developing potentially life-threatening conditions and death. Therefore, it can be of value as a risk stratification tool in COVID-19-affected children (25, 26).
Both genders were affected by a higher male predominance. This finding is in line with a former report in which it was shown that of 48 pediatrics admitted with SARS-CoV-2 infection, 52% were male. This gender variation might also be related to a shorter life span in males than females. An explanation could be that females experience a stronger antigenic reaction to infections and vaccines at the cost of a higher incidence of autoimmune diseases (27-30) than males, who, in turn, are more susceptible to infections.
It is recommended that healthcare providers pay attention to the non-respiratory presentations of COVID-19 in children. In other words, not every child with respiratory distress should have a respiratory origin of COVID-19.
5.1. Study Strengths
To the best of our knowledge, the present study is one of the few studies that were carried out on children with suspected COVID-19 infection. Suspicions and early prediction of this disease are very important for better outcomes and the prevention of infections. Additionally, correlating the presentations with the affected systems is valuable for healthcare providers to help establish various differential diagnoses and consequently establish a preliminary diagnosis through which actions might be taken earlier for a better prognosis. It is observed in the present study that not all children with respiratory distress had respiratory origin of the disease; a child might have respiratory distress due to gastrointestinal infections and diarrhea through metabolic acidosis, which was another strong consideration taken into account by the present study. Additionally, this study correlated the laboratory findings with the presentations. . It seems that serum albumin and D-dimer were significantly reduced and elevated, respectively in children whose presentations were non-respiratory manifestations.
5.2. Study Limitations
The current study’s limitations included the limited sample size, which was a major concern, and the overlap between COVID-19 symptoms and those of multiple system affection. This means that numerous cases might be underestimated, which might eventually contribute to the underdiagnosis of a larger population.
5.3. Conclusions
A diversity of presentations for COVID-19 is observed in children that could be classic or non-typical, such as hematological, neurological, or renal presentations. Respiratory manifestations in children could be a clue for another system affection.