1. Background
As of December 2019, the coronavirus disease 2019 (COVID-19) pandemic has become a particular danger to human health (1) and affected all ages; however, children are more susceptible to clinical effects to have better outcomes and milder course (2). The COVID-19 epidemic has been observed to vary between and within countries around the world regarding infections, hospitalizations, and mortality rates; nevertheless, questions about risk factors and protections against COVID-19 are increasingly consolidated (2, 3).
Recent evidence suggests that risk factors for developing COVID-19 in adults range from demographic factors to the presence of underlying conditions, such as cardiovascular disease (CVD), hypertension, and chronic obstructive pulmonary disease (COPD) (2-4). With regard to the risk factors mentioned, age and specific comorbidities, such as obesity, are more likely to contract COVID-19 and face more severe consequences (3).
Furthermore, a subset of laboratory factors, pro-inflammatory cytokine levels, and complications have been implicated as underlying risk factors for COVID-19 severity and mortality (4). The mortality rate in children with COVID-19 is much lower than in adults, which is U-shaped with age. Mortality rates in the general population of 109 per 100,000 and 1.0 per 100,000 in children (5) vary with age from 0.5 at birth to about 0.8 per 100,000 at the age of 19 years (6).
Coronavirus disease 2019 affects many systems or organs, such as respiratory, gastrointestinal (GI), cardiac, or nervous systems (7). The most common signs and symptoms in many COVID-19 patients are fever and cough, along with diarrhea, abdominal pain, sore throat, nasal congestion, and vomiting (8). Symptoms can be so severe that hospitalization is required (9), and in terms of clinical presentation, COVID-19 infection can cause asymptomatic cases (10) and range from progressive progression from mild to moderate to mild influenza-like illness (ILI), clinically good to life-threatening complications (11), although mortality in children has also been rarely reported (12).
The main component of COVID-19 infection is the respiratory tract; it can damage vital organs, such as the lungs, liver, heart, kidneys, and gastrointestinal system (13). In a meta-analysis, Zhao et al. (14) concluded that inflammatory markers, especially white blood cells (WBC), absolute lymphocyte count (ALC), absolute neutrophil count (ANC), platelet (PLT), C-reactive protein (CRP), ferritin, D-dimer, lactate dehydrogenase (LDH), fibrinogen, and erythrocyte sedimentation rate (ESR), were correlated with the multisystem inflammatory syndrome in children and adolescents with COVID-19.
2. Objectives
Considering the literature and the facts mentioned above about the clinical course in children with COVID-19, this study aimed to assess the factors that influence the mortality rate of children with confirmed COVID-19 infection.
3. Methods
This study was performed using a cross-sectional approach, and the data were extracted from medical records. All children with confirmed COVID-19 infection transferred to the Pediatric Ward of Ali Ibn Abi Talib Hospital in Zahedan (capital of Sistan and Baluchestan province, Iran) between 2021 and 2022 were included in the study. Coronavirus disease 2019 infections have been confirmed based on oral and oropharyngeal swab samples and real-time polymerase chain reaction (RT-PCR) testing. Demographic epidemiological variables, clinical presentations, underlying diseases, laboratory results, radiographic results, and pharmacological treatments were extracted from the medical records. In addition, clinical manifestations of children infected with COVID-19, including fever, difficulty breathing, cough, weakness, anorexia, diarrhea, nausea-vomiting, skin rash, and abdominal pain, were also extracted.
All treatments, including medications and supportive therapy, were also evaluated. In all children, the measures of WBC, lymphocyte count, complete blood count, hemoglobin (Hb), CRP, and ESR were recorded. In addition, liver enzymes, such as alanine transaminase (ALT), aspartate aminotransferase (AST), and LDH, PLT, potassium (K), and sodium (Na), were evaluated. All children had a chest X-ray or computed tomography (CT) scan to evaluate lung damage. This study was approved by the Health Research Institute of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1399.371).
Children admitted to the pediatric ward with a diagnosis of COVID-19 between the ages of 1 month and 19 years were included in the study. Moreover, children with infectious diseases other than COVID-19, those who tested negative, and those with primary immunodeficiency were excluded from the research. Patients with a missing status at discharge and hospitalization for less than 24 hours were also excluded. Collected data were analyzed using SPSS software (version 18; SPSS Inc., Chicago, Ill, the USA). Descriptive statistics are presented as mean and standard deviation for numeric data and frequencies and percentages for categorical data. The chi-square test, Fisher’s exact test, and t-test were applied to inferential statistics. The significance level was < 0.05 for all techniques.
4. Results
The study data resulted in a mortality rate of 13.67% in children and adolescents with COVID-19, distributed as 14.3% and 13.2% in female and male children, respectively. The mean values of age for all the children and adolescents with COVID-19, dead children, and alive children were 5.72 ± 4.97, 5.76 ± 5.38, and 5.71 ± 4.92 years, respectively.
About 96 children (52.5%) needed a CT scan due to a lack of obtaining better signs, low oxygen levels, severe respiratory symptoms, or trouble breathing. Of these children, 36 cases had normal CT scans, and the others had some CT findings, such as 3 cases (1.6%) of reticular pattern, 4 cases (2.2%) of pleural effusion, 2 cases (1.1%) of atelectasis, 46 cases (25.1%) of ground-glass, and 5 cases (2.7%) of consolidation.
Of 183 children with COVID-19, 105 individuals were free of underlying diseases, and 78 individuals had underlying diseases, as shown in Table 1. Of the children with COVID-19, 24 cases had blood disorders, with 4 deaths due to lymphoma (n = 1), acute melanocytic leukemia (n = 1), and acute lymphoblastic leukemia (ALL) (n = 2). Of the children, 16 cases had central nervous system (CNS) diseases, with 4 deaths, all due to cerebral palsy.
| Involved Organ | No. (%) | Deaths |
|---|---|---|
| Underlying Diseases | ||
| Hematology | ||
| Lymphoma | 3 (12.5) | 1.0 |
| Major thalassemia | 1 (4.2) | 0.0 |
| Histiocytosis | 1 (4.2) | 0.0 |
| Neuroblastoma | 1 (4.2) | 0.0 |
| AML | 3 (12.5) | 1.0 |
| Polycythemia | 1 (4.2) | 0.0 |
| ALL | 8 (33.3) | 2.0 |
| Beta thalassemia with ALL | 1 (4.2) | 0.0 |
| Down syndrome with ALL | 1 (4.2) | 0.0 |
| Franconia disease | 1 (4.2) | 0.0 |
| Hemangioma | 1 (4.2) | 0.0 |
| Aplastic anemia | 1 (4.2) | 0.0 |
| Hemophilia VIII | 1 (4.2) | 0.0 |
| Total | 24 (100) | 4 |
| CNS | ||
| Cerebral palsy | 10 (62.5) | 4.0 |
| Myelomeningocele | 1 (6.3) | 0.0 |
| Epilepsy | 3 (12.5) | 0.0 |
| Mental retardation | 1 (6.3) | 0.0 |
| Hydrocephaly | 1 (6.3) | 0.0 |
| Total | 16 (94) | 4 |
| Respiratory | ||
| Asthma | 5 (100.0) | 0.0 |
| Total | 5 (100.0) | 0.0 |
| Related Diseases | ||
| Endocrinology | ||
| Diabetes mellitus | 6 (60.0) | 1 |
| Metabolic disorder | 1 (10.0) | 0 |
| Hypothyroid | 1 (10.0) | 0 |
| Niemann-Pick | 1 (10.0) | 1 |
| Hypocalcemia | 1 (10.0) | 0 |
| Total | 10 (100.0) | 2 |
| Cardiovascular | ||
| Dilated cardiomyopathy | 3 (30.0) | 0 |
| Patent ductus arteriosus | 4 (40.0) | 3 |
| Ventricular septal defect and pulmonary hypertension with Down syndrome | 1 (10.0) | 1 |
| Ventricular septal defect after surgery | 1 (10.0) | 1 |
| Congestive heart failure | 1 (10.0) | 0 |
| Total | 10 (100.0) | 5 |
| Kidney | ||
| Chronic kidney disease | 3 (37.5) | 1 |
| Acute kidney disease | 1 (12.5) | 1 |
| Nephrotic syndrome | 1 (12.5) | 0 |
| Bartter syndrome | 2 (25.0) | 0 |
| Multicystic kidney disease | 1 (12.5) | 0 |
| Total | 8 (100) | 2 |
| Gastrointestinal | ||
| Adenocarcinoma | 1 (20.0) | 1 |
| Esophageal cancer | 1 (20.0) | 0 |
| Celiac disease | 2 (40.0) | 0 |
| Hepatoblastoma | 1 (20.0) | 0 |
| Total | 5 (100) | 1 |
Abbreviations: AML, acute melanocytic leukemia; ALL, acute lymphoblastic leukemia; CNS, central nervous system.
Of the children, 5 cases had asthma with no deaths. Of the children, 10 children had endocrinology disorder with 2 deaths due to diabetes mellitus and Niemann-Pick each disease one child. Of the children, 10 subjects had CVD, with 50% deaths due to patent ductus arteriosus (PDA) (n = 3), ventricular septal defect (VSD) with pulmonary hypertension (PH) (n = 1), and VSD closure with surgery (n = 1). Of the children in the study, 8 cases had diseases related to kidneys, with 2 deaths due to end-stage renal disease (n = 1) and acute kidney disease (n = 1). Moreover, 5 cases had diseases related to gastrointestinal organs, with 1 death due to adenocarcinoma.
Table 2 shows the clinical manifestations distribution in dead and surviving children. Of the children analyzed in the study, 25 subjects died, and 158 subjects survived, with a mortality rate of 136.6 in 1000. From the clinical manifestations, fever was observed more frequently in dead children than in survived children (96.0% vs. 85.4%) but not significantly (P = 0.123). Central nervous system diseases were significantly less frequent in survived children than in deaths (28.0% vs. 62.0%) (P = 0.006). Respiratory diseases and gastrointestinal diseases, including vomiting and diarrhea, were observed more frequently in dead children with COVID-19 not significantly (P > 0.05) when nephrology and dermatology of clinical manifestations were more frequently observed in survived children with COVID-19 not significantly (P > 0.05).
| Clinical Manifestations and Status | Discharge | Total | Critical Value | P-Value | |
|---|---|---|---|---|---|
| Died | Survived | ||||
| Fever | 207 | 0.123 | |||
| No | 1 (4.0) | 23 (14.6) | 24 (13.1) | ||
| Yes | 24 (96.0) | 135 (85.4) | 159 (86.9) | ||
| CNS | 10.281 | 0.006 | |||
| No | 7 (28.0) | 98 (62.0) | 105 (57.4) | ||
| Seizure | 4 (16.0) | 12 (7.6) | 16 (8.7) | ||
| Low consciousness | 14 (56.0) | 48 (30.4) | 62 (33.9) | ||
| Respiratory | 0.19 | 0.103 | |||
| No | 7 (28.0) | 69 (43.7) | 76 (41.5) | ||
| Yes | 18 (72.0) | 89 (56.3) | 107 (58.5) | ||
| Gastrointestinal | 0.664 | 0.345 | |||
| No | 13 (52.0) | 92 (58.2) | 105 (57.4) | ||
| Vomiting + diarrhea | 12 (48.0) | 66 (41.8) | 78 (42.6) | ||
| Nephrology | 0.596 | 0.351 | |||
| No | 25 (100.0) | 151 (95.6) | 176 (96.2) | ||
| Yes | 0 (0.0) | 7 (4.4) | 7 (3.8) | ||
| Dermatology | 0.134 | 0.073 | |||
| No | 25 (100.0) | 141 (89.2) | 166 (90.7) | ||
| Yes | 0 (0.0) | 17 (10.8) | 17 (9.3) | ||
| Total | 25 (100.0) | 158 (100.0) | 183 (100.0) | ||
Abbreviation: CNS, central nervous system.
Table 3 shows the comparison of laboratory measures in dead and surviving children. The table shows that the following measures were significantly different in deaths in comparison to in living children:
White blood cell count (13.28 ± 9.80 and 9.04 ± 10.05; P = 0.051), PLT (205.56 ± 139.08 and 293.69 ± 179.76; P = 0.020), LDH (1114.92 ± 1275.12 and 480.86 ± 384.96; P < 0.001), ALT (226.32 ± 634.93 and 76.53 ± 243.78; P = 0.033), ESR (52.92 ± 40.81 and 28.19 ± 28.97; P < 0.001), and CRP (66.28 ± 36.75 and 30.75 ± 35.63; P < 0.001)
From the significant measures, all except PLT were higher in deaths.
| Laboratory Measures and Status | Mean ± SD | t | P-Value |
|---|---|---|---|
| WBC | 1.972 | 0.050 | |
| Dead | 13.28 ± 9.80 | ||
| Survived | 9.04 ± 10.05 | ||
| Lym | 0.863 | ||
| Dead | 34.46 ± 21.54 | -0.173 | |
| Survived | 35.25 ± 21.07 | ||
| Hb | -1.496 | 0.136 | |
| Dead | 10.31 ± 2.04 | ||
| Survived | 11.01 ± 2.21 | ||
| PLT | -2.341 | 0.020 | |
| Dead | 205.56 ± 139.08 | ||
| Survived | 293.69 ± 179.76 | ||
| LDH | 5.022 | < 0.001 | |
| Dead | 1114.92 ± 1275.12 | ||
| Survived | 480.86 ± 384.96 | ||
| AST | 1.389 | 0.167 | |
| Dead | 181.84 ± 360.22 | ||
| Survived | 85.22 ± 317.10 | ||
| ALT | 2.148 | 0.033 | |
| Dead | 226.32 ± 634.93 | ||
| Survived | 76.53 ± 243.78 | ||
| Na | 0.572 | 0.568 | |
| Dead | 138.04 ± 5.67 | ||
| Survived | 137.53 ± 3.90 | ||
| K | 0.896 | 0.371 | |
| Dead | 4.42 ± 0.87 | ||
| Survived | 4.27 ± 0.73 | ||
| ESR | 3.73 | < 0.001 | |
| Dead | 52.92 ± 40.81 | ||
| Survived | 28.19 ± 28.97 | ||
| CRP | 4.614 | < 0.001 | |
| Dead | 66.28 ± 36.75 | ||
| Survived | 30.75 ± 35.63 |
Abbreviations: WBC, white blood cells; Lym, lymphocytes; Hb, hemoglobin; PLT, platelets; LDH, lactate dehydrogenase; AST, aspartate aminotransferase; ALT, alanine transaminase; Na, sodium; K, potassium; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; SD, standard deviation.
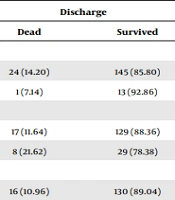
Table 4 shows the death rates in different treatment protocols. Fisher’s exact test showed that only the remdesivir medication had an effective impact on the survival of children with COVID-19. Table 5 shows the results of logistic regression to find the effect of underlying diseases on survival status. In this study, the odds ratio is the measure of the association between exposure (underlying diseases) and outcome (death).
| Medications and Status | Discharge | Total | Fisher’s Exact Test | P-Value | |
|---|---|---|---|---|---|
| Dead | Survived | ||||
| IVIG | 0.696 | 0.402 | |||
| No | 24 (14.20) | 145 (85.80) | 169 (100.00) | ||
| Yes | 1 (7.14) | 13 (92.86) | 14 (100.00) | ||
| Prednisolone | 0.177 | 0.098 | |||
| No | 17 (11.64) | 129 (88.36) | 146 (100.00) | ||
| Yes | 8 (21.62) | 29 (78.38) | 37 (100.00) | ||
| Remdesivir | 0.057 | 0.038 | |||
| No | 16 (10.96) | 130 (89.04) | 146 (100.00) | ||
| Yes | 9 (24.32) | 28 (75.68) | 37 (100.00) | ||
| Favipiravir | 0.355 | 0.355 | |||
| No | 23 (13.22) | 151 (86.78) | 174 (100.00) | ||
| Yes | 2 (22.22) | 7 (77.78) | 9 (100.00) | ||
| Hydroxychloroquine | 1.00 | 0.582 | |||
| No | 23 (13.86) | 143 (86.14) | 166 (100.00) | ||
| Yes | 2 (11.76) | 15 (88.24) | 17 (100.00) | ||
| Lopinavir | 1.00 | 0.642 | |||
| No | 25 (13.89) | 155 (86.11) | 180 (100.00) | ||
| Yes | 0 (0.00) | 3 (100.00) | 3 (100.00) | ||
| Kaletra | 1.00 | 0.592 | |||
| No | 24 (13.87) | 149 (86.13) | 173 (100.00) | ||
| Yes | 1 (10.00) | 9 (90.00) | 10 (100.00) | ||
| Atazanavir | 0.245 | 0.245 | |||
| No | 23 (13.07) | 153 (86.93) | 176 (100.00) | ||
| Yes | 2 (28.57) | 5 (71.43) | 7 (100.00) | ||
| Total | 25 (13.66) | 158 (86.34) | 183 (100.00) | ||
Abbreviation: IVIG, intravenous immunoglobulin.
| Underlying Diseases (Reference) | Unadjusted | Adjusted | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SD | Wald | P | OR | B | SD | Wald | P | OR | |
| Hematology (no hematology) | 0.273 | 0.596 | 0.210 | 0.646 | 1.314 | 0.903 | 0.670 | 1.812 | 0.178 | 2.466 |
| Endocrinology | 0.489 | 0.822 | 0.354 | 0.552 | 1.630 | 1.078 | 0.882 | 1.491 | 0.222 | 2.938 |
| Cardiovascular | 2.035 | 0.676 | 9.068 | 0.003 | 7.650 | 2.392 | 0.738 | 10.493 | 0.001 | 10.936 |
| Kidney | 0.790 | 0.847 | 0.870 | 0.351 | 2.203 | 1.336 | 0.902 | 2.193 | 0.139 | 3.804 |
| Respiratory | 0.690 | 0.473 | 2.124 | 0.145 | 1.994 | 0.789 | 0.533 | 2.189 | 0.139 | 2.201 |
| Gastrointestinal | 0.252 | 0.432 | 0.341 | 0.559 | 1.287 | 0.425 | 0.488 | 0.758 | 0.384 | 1.530 |
| Central nervous system | 0.840 | 0.623 | 1.822 | 0.177 | 2.317 | 1.435 | 0.703 | 4.164 | 0.041 | 4.198 |
Abbreviations: SD, standard deviation; OR, odds ratio.
According to Table 5, children with hematologic diseases were 1.3 times more likely to experience death than those without these diseases, and after adjusting, the odds changed by 2.67; however, in both cases, it was not significant. The most important disease was of the heart system, such that in the children with COVID-19 who had this disease, the odds of death were significantly higher than those who did not have these diseases. More details are observable in Table 5.
5. Discussion
The goal of the present study was to assess the causes of death in children with COVID-19. Therefore, of the clinical symptoms and signs requiring referral to the studied emergency services, CNS diseases were the most common, followed by respiratory diseases. The most important laboratory abnormal measurements were CRP, ESR, Hb, and liver enzymes. The study also showed that underlying diseases, such as cardiovascular and central nervous system diseases, were more effective than other underlying diseases.
Ranabothu et al. (15) performed a pediatric study in 2020 and characterized the clinical features of children with confirmed COVID-19 infection based on available data. They report that the prevalence of COVID-19 in children is lower than in adults, with rates ranging from 1% to 5%.
Armin et al.’s (16) study showed the mortality rate in Iranian children with COVID-19 in 2022 and that the mortality rate was 8.3% (59 from 711) in all age groups, more common in male children, especially in children with underlying diseases. Similarly, Efendi et al. (17) conducted a study to predict the death rate of children with COVID-19 in Indonesia in 2023, which was reported as 2.7% lower than Armin et al.’s study (16). In this regard, Flaxman et al. (5) in 2023 found 1 person per 100,000 across all age groups, about 4 children under 1 year, 0.6 in children from 1 to 4 years, 0.4 for children from 5 to 9 years, 0.5 for children from 10 years to 14 years, and 1.8 per 100,000 for children aged 15 - 19 years. Efendi et al. (17) reported that several factors, such as age, treatment, disease severity, and underlying medical conditions, had a significant effect on the mortality rate of children with COVID-19. In this way, it is possible that as age increases, the risk of dying from COVID-19 will decrease.
In 2020, a Brazilian study (18) reported that the probability of in-hospital mortality was 4.8% during the first 10 days and increased with the length of hospital stay. In 2022, a study by Gonzalez-Dambrauskas et al. (19) showed that deaths among children under 2 years of age with COVID-19 occurred more frequently in male children and about half of those with the diseases, such as lung and heart diseases.
To confirm the above-mentioned facts about the factors influencing mortality in children with COVID-19, Efendi et al. (17) pointed to underlying diseases, such as heart disease, laboratory measurements, and clinical manifestations. In this regard, preventive measures and systematic management strategies are needed to improve outcomes in children with heart disease (20) and the extent to which markers are monitored. Dynamic inflammation can help pediatricians assess and effectively evaluate the care of children and adolescents with multisystem inflammatory syndrome, especially as a priority during the COVID-19 pandemic (21). The most common symptoms in children with COVID-19 are fever and cough, followed by diarrhea and abdominal pain, and very few children have severe clotting disorders, respiratory failure, shock, and kidney damage (21).
Of the clinical presentations in the present study’s children with COVID-19, CNS diseases had a significant presentation, compared to others, when it has been reported that the clinical presentations were varied from GI symptoms, cardiac disease, mild or absent respiratory symptoms, variable incidence of rash, red eyes, and oral mucous membrane changes from center to center (22). A study was performed in Iran by Kiani et al. (23) in 2021 and reported fever (86.5%), asthenia (75.7%), and anorexia (73%) as manifestations of clinical symptoms. Moreover, abdominal pain (48.7%), diarrhea (45.9%), nausea and vomiting (37.8%), cough (32.4%), sore throat (29.7%), and shortness of breath (27%) were the most common symptoms.
Mantovani et al. (24) in 2021 found that 47% of children with COVID-19 had a fever, 37% had a cough, 2% had a stuffy nose, and 1% had difficulty breathing. Children with mild symptoms accounted for 79% of cases; nevertheless, only 4% were in critical condition.
In 2020, two studies by Oualha et al. (25) and Bixler et al. (26) reported some facts about the relationship between underlying diseases and death due to COVID-19 such that Oualha et al. (25) observed that 70% of their patients with COVID‐19 had underlying diseases, more frequently CNS (25.92%). Bixler et al. (26) observed that among the 121 dead children due to COVID-19, 91 cases (75%) had underlying diseases. Of the children, 79 cases (65%) died after admission to a hospital, and 39 subjects (32%) died at home or in the emergency department (ED) (26). Kiani et al. (23) noticed that 12% of children had underlying medical conditions in which gastroenteritis was more common in their study. Ranabothu et al. (15) concluded that the majority of children with COVID-19 had one or more underlying medical conditions, such as chronic lung disease and CVD.
In the present study of children, 42.6% (n = 78) had underlying diseases, such as hematology and CNS, that were more common, and those with heart disease had the highest mortality, followed by CNS diseases. Among 78 children with this underlying disease, 13.12%, 8.74%, 2.73%, 5.46%, 5.46%, 4.37%, and 2.73%, respectively, suffered from hematology, neurology, respiratory, endocrine, cardiovascular, renal, and digestive diseases. Consistent with the present study’s findings, Armin et al. (16) observed that more than 90% of their children with COVID-19 had underlying diseases than in the present study. The aforementioned study demonstrated that 35.26% of the children with CNS had malignancy and primary immunodeficiency, and 8.82% had heart disease. A case series in Iran (27) reported no underlying disease in children with COVID-19; however, Singh et al. (28) detected neurological disease in 11.11% of patients with COVID-19. Kiani et al. (23) reported that about 60% and 8% of children with COVID‐19 had Hb and mean corpuscular volume (MCV) less than normal levels, 80% and 60% had abnormal elevations in CRP and ESR, 32% and 35% had an increase in ALT and AST levels, respectively, and about 40% of them had hypoalbuminemia.
Armin et al. (16) observed an increase in ESR, CRP, LDH, AST, and ALT and the presence of proteinuria and hematuria in more than 50% of patients. Qiu et al. (29) noticed a decrease in lymphocyte counts, higher levels of procalcitonin and creatinine, and increased D-dimer levels in patients with COVID-19. Sun et al. (30) reported normal or increased leukocyte count, high levels of CRP, procalcitonin, lactate dehydrogenase, and abnormal liver function. A study showed an association between admission to the pediatric intensive care unit (PICU) and higher levels of CRP, procalcitonin, and pro-B-type natriuretic peptide and platelet count (31). Henry et al. (32) observed that about 69.6% of the children with COVID-19 had normal leukocyte count and absence of lymphopenia due to milder disease. Furthermore, they revealed that an increase in procalcitonin levels could be caused by bacterial coinfection as a complication of COVID-19, also reported by Xia et al. (33), with an increase in 80% of Chinese pediatric patients. Elevated liver enzymes that were reported in the present and the aforementioned studies might be related to the presented angiotensin-converting enzyme 2 (ACE2) in the intestines. Finally, and based on the available data, it is not possible to document a pattern of changes in the laboratory measures in pediatric COVID-19 based on disease severity.
Kiani et al. (23) noticed that about a third of their children had breathing problems; nevertheless, chest X-rays were reported to be unspecific in most children. In this regard, the most common finding on chest CT scans was bilateral opacification, which has been reported by Hoang et al. (34). These results are comparable to the results of the current study; among 147 individuals who underwent CT scans 3, 4, 2, 46.5, and 87 reticular, pleural effusion, atelectasis, opacified glass, solidification, and normal CT scans were present, respectively. Kiani et al. (23) reported that their children with COVID-19 received antibiotics, such as ceftriaxone and clindamycin, and antiviral drugs, such as Kaletra. Alternatively, if needed, the patient is given a bronchodilator, such as Duolin or Ventolin, along with a nebulizer and oxygenated via a nasal cannula. In the present study, children 14, 37, 37, 9, 17, 3, 10, and 7 received intravenous immunoglobulin (IVIG) injections, prednisolone, remdesivir, favipiravir, hydroxychloroquine, lopinavir, Kaletra, and atazanavir, respectively. Moreover, in the emergency situation, antibiotics were used. Because the data were collected from the medical records of the patients, there were some constitutive limitations in the present study.
5.1. Conclusions
The present study concluded that the associated factors with death were laboratory measures, such as CRP, ESR, Hb, and liver enzymes, and underlying diseases, such as cardiovascular and central nervous system diseases. Knowledge regarding the clinical characteristics and disease burden in children with COVID-19 is the critical stage of the pandemic for better treatment, better control of transmission, and appropriate allocation of healthcare resources to decline mortality.