1. Background
Acute otitis media (AOM) is characterized by moderate to severe tympanic membrane bulging or unrelated otorrhea, accompanied by acute signs of middle ear infection and inflammation (1). The diagnosis of AOM is based on the presence of symptoms associated with middle ear inflammation, such as pain, fever, bulging, and redness of the tympanic membrane (2). Acute otitis media is often associated with middle ear effusion, which leads to reduced tympanic membrane motion (3).
The American Academy of Pediatrics recommends a cautious approach to managing AOM in specific pediatric cases. For children aged 6 months to 2 years with unilateral AOM and mild symptoms, a period of observation is advised before initiating antibiotic treatment. If symptoms persist or worsen over 48 to 72 hours, initiating antibiotics is considered prudent. In contrast, infants under 6 months of age diagnosed with AOM should receive immediate antibiotic treatment. For those younger than 2 months old with AOM and fever, a thorough assessment for bacteremia is essential before starting antibiotic therapy (1, 2).
In line with the findings of McCormick et al. (4), other investigations have compared the watchful waiting strategy to immediate antibiotic intervention. These studies have demonstrated that immediate antibiotic administration is associated with reduced instances of treatment failure and improved symptom management. However, this comes at the cost of an increased risk of antibiotic-related adverse events and a higher prevalence of nasopharyngeal carriage of multidrug-resistant Streptococcus pneumoniae strains compared to watchful waiting. Such studies suggest that for certain children with non-severe AOM, a watchful waiting approach might be a viable alternative to immediate antibiotic therapy (5, 6). Only one Iranian study on this issue revealed that faster recovery from AOM is achieved when antibiotics are prescribed, although the potential risk of side effects should be considered (7).
Considering the complications associated with antibiotic use, including the potential for adverse effects and the growing concerns about antibiotic resistance, this study involving children aged 6 months and older was carried out. The objective was to compare the outcomes of patients who have completed a watchful waiting approach to those who have received antibiotic therapy, providing valuable insights into the optimal management of AOM in this specific demographic.
2. Methods
This study was conducted as a quasi-experimental study in Shiraz, Iran, involving 100 children aged between 6 months and 18 years who presented with symptoms and signs of AOM according to diagnostic criteria. The diagnostic criteria for AOM included the presence of at least 2 of the following: Abnormal tympanic membrane color, opacification, decreased motility, or middle ear effusion, along with at least one of the following acute inflammation symptoms: Ear pain, marked redness, or bulging of the tympanic membrane (2).
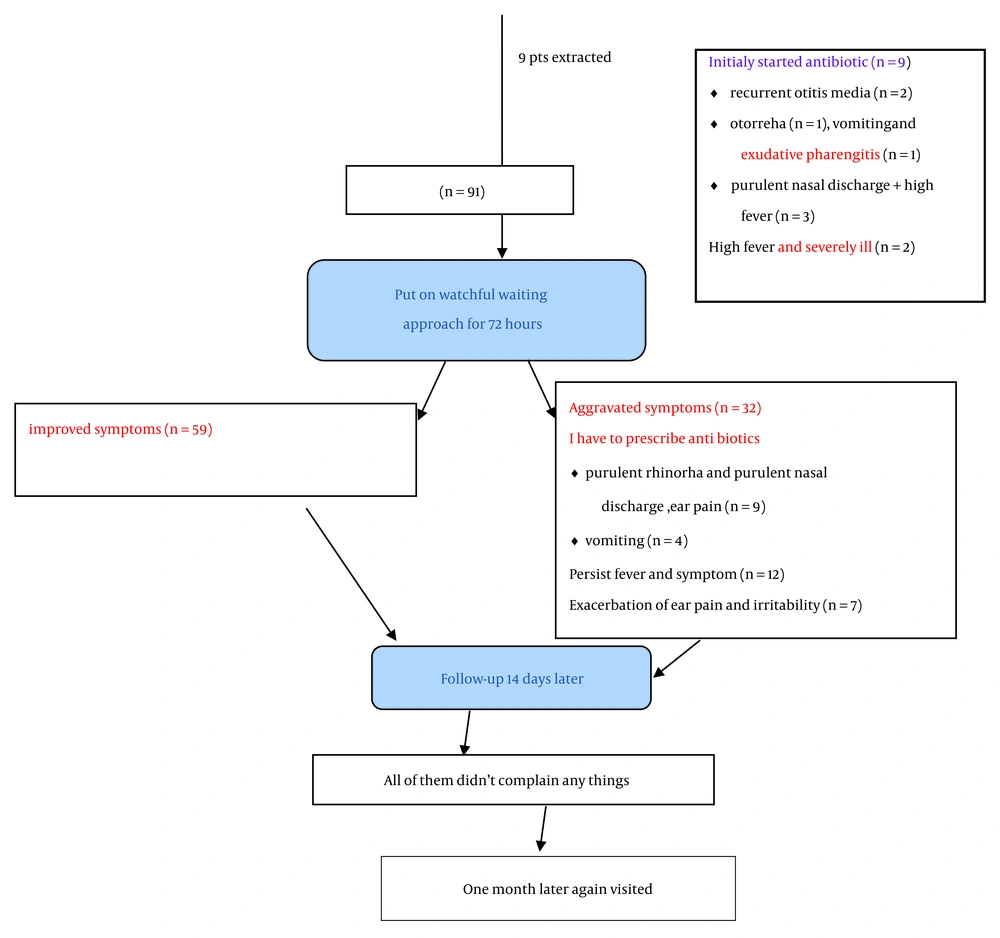
Parents were invited to participate in the study, and written informed consent letters were obtained from them. Upon their agreement, their personal information was recorded, and their contact details were collected. The research objectives were thoroughly explained to them. All enrolled patients, except those initially started on antibiotics due to worsening conditions, were placed on a watchful waiting strategy, as depicted in Figure 1 (CONSORT form). They received prescriptions for analgesics and antipyretics to manage ear pain and fever. The parents were provided with comprehensive information to closely monitor their child’s progress throughout the course of the disease.
Approximately 48 - 72 hours after the initial visit, the researcher maintained communication with the parents, either by phone or, when possible, through in-person consultations, to assess the disease’s progression. If the severity of symptoms had decreased or resolved, the watchful waiting strategy was extended for up to 10 days. However, if symptoms persisted or worsened, antibiotics were prescribed for various reasons, and these reasons were meticulously documented. The antibiotic treatment lasted for 10 days, with a follow-up period of 14 days conducted after the initial visit. All of these steps and physical examinations were conducted by a single researcher.
The inclusion criteria for participation in the watchful waiting strategy encompassed the presence of mild to moderate symptoms, a fever below 39°C, and a non-toxic appearance. The exclusion criteria comprised recent antibiotic usage, facial or cranial deformities, immunodeficiency, malnutrition, a history of frequent AOM episodes, hearing problems in the medical history, tympanic membrane perforation, Down syndrome, otorrhea (ear discharge), and poor compliance with the study protocol.
At the end of the specified observation period, each patient was scheduled for a follow-up visit. Ultimately, an evaluation of the success and failure of the watchful waiting strategy in reducing antibiotic utilization was conducted based on the data collected in this study and subsequent statistical analysis.
2.1. Ethical Considerations
Written informed consent letters were obtained from all parents/guardians. This study was approved by the Ethics Committee of Islamic Azad University (code: IR.IAU.KAU.REC.1399.014) and registered in the Iranian Registry of Clinical Trials (IRCT20200610047724N1).
2.2. Statistical Analysis
The data were reported using descriptive statistics and analyzed using t-tests and chi-square tests. The significance level for the tests was set at less than 0.05. Additionally, logistic regression models were used to estimate odds ratios. The data were analyzed using IBM SPSS Statistics for Windows (version 22.0, Armonk, NY: IBM Corp, USA).
3. Results
The study encompassed subjects within an age range spanning from 1 year to 15 years, with a mean age of 6.06 ± 2.71 years. Among these participants, 59 cases (59%) were male. Specifically, the mean age for patients was 5.12 ± 2.43 years, ranging from 1 to 11 years in the waiting group, and 3.11 ± 4.97 years, ranging from 1 to 15 years in the antibiotic group (P = 0.786). Furthermore, there was no significant difference in the distribution of gender between the 2 groups (P = 0.454) (Table 1).
| Variables | Antibiotic Group (n = 41) | Waiting Group (n = 59) | P-Value | OR (95% CI) |
|---|---|---|---|---|
| Age (mean ± SD) | 3.11 ± 4.97 | 5.2 ± 2.43 | 0.786 | 0.97 (0.1 - 84.13) |
| Gender | 0.454 | 0.97 (0.1 - 84.13) | ||
| Male | 64% | 56% | ||
| Female | 36% | 44% |
Comparison of Gender and Age in 2 Groups
Out of the 100 patients involved in the study, 59 cases (59%) opted for the waiting group and completed the study without requiring antibiotics. The remaining 41 patients (41%) were managed with antibiotics. Among the antibiotic group, nine patients (22.2%) commenced antibiotic treatment early due to specific indications related to critical conditions. These indications included a history of recurrent AOM (n = 2, 22.2%), otorrhea (n = 1, 11.1%), purulent nasal discharge (n = 3, 33.4%), vomiting and bilateral exudative tonsillar enlargement (n = 1, 11.1%), and high-grade fever and an ill appearance (n = 2, 22.2%). These 9 patients were not placed in the watchful waiting strategy but received antibiotics early (Figure 1).
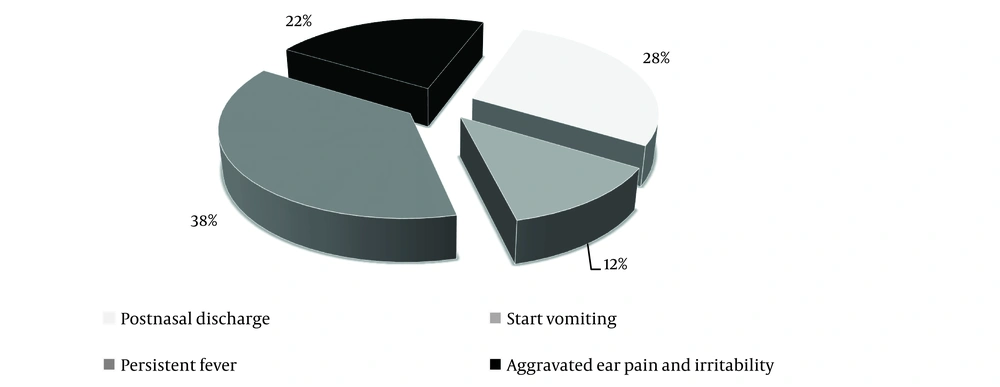
Conversely, the other 32 patients from the waiting group were excluded and subsequently administered antibiotics after 48 - 72 hours of observation for some reasons, including purulent rhinorrhea and purulent postnasal discharge (n = 9), the onset of vomiting (n = 4), persistent fever (n = 12), and exacerbation of ear pain and irritability (n = 7) (Figure 2).
A comparison was made between the two study groups to assess the relevant signs and symptoms associated with upper respiratory tract infections, such as runny nose, hoarseness, sore throat, fever, tonsillar enlargement, snoring, postnasal discharge, and unilateral or bilateral tympanic membrane involvement (Table 2).
| Variables | Antibiotic Group (n = 41), No. (%) | Waiting Group (n = 59), No. (%) | P-Value | OR (95% CI) |
|---|---|---|---|---|
| Tympanic membrane | 0.313 | 0.55 (0.17 - 1.72) | ||
| Unilateral | 34 (82.9) | 53 (89.8) | ||
| Bilateral | 7 (17.1) | 6 (10.2) | ||
| Snoring | 0.252 | 1.79 (0.65 - 4.9) | ||
| Yes | 10 (24.4) | 9 (15.3) | ||
| No | 31 (75.6) | 50 (84.7) | ||
| Fever | 0.066 | 0.3 (0.08 - 1.07) | ||
| Yes | 33 (80.5) | 55 (93.2) | ||
| No | 8 (19.5) | 4 (6.8) | ||
| Enlarged tonsil | 0.740 | 0.80 (0.21 - 2.9) | ||
| Yes | 4 (9.8) | 7 (11.9) | ||
| No | 37 (90.2) | 52 (88.1) | ||
| Cold symptoms | 0.193 | 1.98 (0.69 - 5.65) | ||
| Yes | 35 (85.4) | 44 (74.6) | ||
| No | 6 (14.6) | 15 (25.4) | ||
| PND | 0.001 | 23 (2.92 - 190) | ||
| Yes | 12 (29.3) | 1 (1.7) | ||
| No | 29 (70.7) | 57 (98.3) |
Comparison of Unilateral or Bilateral Tympanic Membrane, Snoring, Fever, Enlarged Tonsils, Upper Respiratory Tract Infection, and Postnasal Discharge in Both Groups
Regarding the presence of unilateral or bilateral tympanic membrane involvement, the difference between the two groups was 6.9%, which did not reach statistical significance (P = 0.313). A similar pattern emerged concerning the prevalence of snoring, where the difference between the two groups was 9.1% (P = 0.252), suggesting that snoring did not significantly influence the choice between the waiting method and antibiotic use.
The analysis revealed no statistically significant difference between the two groups in terms of fever (P = 0.66), with a difference of 12.7% observed between the groups. Similarly, there was no statistically significant difference in tonsillar enlargement (P = 0.740).
Notably, there was no significant difference between the two groups in terms of symptoms indicative of upper respiratory tract infections (P = 0.193). The presence or absence of these symptoms did not offer a decisive factor in selecting a treatment strategy.
To investigate the impact of postnasal discharge on the waiting method, the results highlighted a significant difference between the two groups concerning postnasal discharge. Specifically, a higher proportion of patients in the waiting group did not exhibit postnasal discharge, and this difference was statistically significant.
4. Discussion
In line with the 2013 guidelines from the American Academy of Pediatrics, children aged 6 months to 2 years with unilateral AOM and mild symptoms and children over 2 years with mild unilateral or bilateral AOM are advised to undergo observation and wait after consulting with their parents, without an immediate prescription for antibiotics (1). Previous studies have aimed to either support or refute this guideline. Drawing inspiration from these studies and available information, the present investigation was initiated to identify which signs and symptoms, beyond age and severe pain, could aid in making a more informed decision regarding the treatment of AOM.
In the current study, it was observed that more than half of the patients responded favorably to the watchful waiting approach. Antibiotics were prescribed for 32 out of 91 patients after a 72-hour observation period. Importantly, there were no statistically significant differences in age and gender between the two groups (P = 0.786 and P = 0.445, respectively), which aligns with findings from prior meta-analyses and reviews conducted by McCormick et al. (4) and Venekamp et al. (8).
A meta-analysis conducted by Rovers et al. (9) indicated that children under two years of age benefit the most from antibiotic therapy; nevertheless, waiting for therapy is a more reasonable option for children over two years of age. Their analysis suggested that pain and fever subsided earlier in those who received antibiotics.
In the present study, there was no significant difference between the 2 groups concerning the distribution of affected ears (unilateral or bilateral) (P = 0.313). However, studies by Rovers et al. (9) and Spurling et al. (6) have shown that bilateral involvement is more common in the antibiotic group.
Additionally, the prevalence of snoring and enlarged tonsils exhibited no significant differences between the two groups (P = 0.252 and P = 0.740, respectively). The aforementioned findings suggest that physical indicators of upper airway obstruction do not provide clear guidance in choosing a treatment strategy. Adenoid and tonsillar hypertrophy have a significant correlation with otitis media with effusion (OME) and AOM (10).
The prevalence of fever in both treatment groups showed no significant difference (P = 0.066). Nonetheless, some studies, including those by Rovers et al. (9), Tahtinen et al. (5), and Little et al. (11), have indicated that fever tends to subside earlier in the antibiotic group, with a higher incidence of fever among those receiving antibiotics than the waiting group.
Furthermore, when examining the presence of upper respiratory tract infection symptoms in both groups, there was no significant difference (P = 0.193). Therefore, the presence or absence of cold symptoms alone does not provide adequate guidance for determining the appropriate treatment strategy.
A comparative analysis of postnasal discharge between the 2 groups revealed that a higher proportion of patients in the antibiotic group had postnasal discharge and required antibiotic therapy, with this difference being statistically significant (P = 0.001). Consequently, it can be inferred that the waiting method might not effectively alleviate postnasal discharge, and for patients with this symptom, it might not be an ideal treatment strategy (P = 0.001).
Notably, postnasal discharge has received limited attention in prior research, with Tahtinen et al. (12) being one of the few to suggest that children, especially those with tympanic membrane bulging, are more likely to benefit from antibiotic therapy. Tympanic membrane bulging is typically associated with increased secretion and might manifest as non-purulent postnasal discharge.
The watchful-waiting approach was mentioned in 9 of the 12 studies of large meta-analysis (13). The patients managed with watchful waiting ranged from 7.5% (14) to 55.2% (15). Antibiotic treatment was required in only 2.8% of cases in a study by Smolinski et al. (16) and in 53.5% of cases in a study by García Ventura et al. (17). In the present study, 32% of antibiotic treatment was required in watchful waiting cases.
Out of the 41 patients in the antibiotic group, 9 cases initially received antibiotic treatment and were excluded from the watchful waiting strategy due to severe and high-risk conditions. The remaining 32 began antibiotics due to a lack of improvement or worsening symptoms after 48 to 72 hours (Figure 1). Consequently, among these children (n = 9) who initially commenced antibiotic treatment, 3 of them (33.4%) did so immediately due to purulent nasal discharge and concurrent rhinosinusitis. Therefore, both purulent and non-purulent postnasal discharge could be regarded as warning signs for initiating antibiotic treatment in patients with AOM.
It seems that further studies with a larger population and antibiotic susceptibility measurements are needed to provide a local guideline for the watchful waiting strategy or antibiotic therapy according to antibiotic susceptibility. The advantages and disadvantages of this trial include decreased antibiotic prescription and side effects, cost-benefit, and decreased antibiotic-resistant pathogens. However, if patients are allocated to the watchful waiting approach, close follow-up is necessary, which might become challenging due to possible antibiotic prescriptions later and loss of patient follow-up. This approach requires cooperative parents.
4.1. Conclusion
The findings of the present study support the notion that the watchful waiting approach is a suitable method for managing mild to moderate symptoms in children over 6 months of age, provided parents are willing to cooperate with necessary follow-up. Although postnasal discharge (PND) is a dependent condition, a patient with AOM associated with purulent or non-purulent postnasal discharge might not be an ideal candidate for the watchful waiting strategy, and consideration should be given to prescribing antibiotics.