1. Introduction
Tracheal tumors are exceedingly rare in pediatric cases, with an incidence rate of 0.2% in this population (1). These tumors can originate from the larynx, bronchi, and trachea. Early detection of tracheal tumors is crucial, as they can lead to life-threatening airway obstruction, necessitating urgent intervention (2). Often, tracheal tumors remain asymptomatic, obstructing 50 to 70% of the trachea without causing noticeable symptoms. Consequently, they are sometimes misdiagnosed as other lung diseases, such as asthma (3). However, common symptoms associated with tracheal tumors include cough, shortness of breath, and nonspecific manifestations like hemoptysis, pneumonia, weight loss, and wheezing. The treatment of tracheal tumors is a multidisciplinary approach, typically involving major surgery (4).
2. Case Presentation
2.1. Present Illness
A 12-year-old girl was referred to Mofid Children's Hospital in Tehran with complaints of dyspnea and a non-productive cough. Her dyspnea was categorized as functional class 2, occurring only when not at rest. She denied recent symptoms of infection and described her dyspnea as positional, worsening when lying down but improving when sitting. Additionally, she reported experiencing dry, non-productive coughing that did not interfere with her sleep. No signs of sleep apnea or paroxysmal nocturnal dyspnea (PND) were noted, and her oxygen saturation remained high during sleep. There was no recent weight loss.
These symptoms initially manifested at the age of 4, leading to an asthma diagnosis. Treatment with short-acting beta-agonists and low-dose inhaled corticosteroids proved ineffective, prompting the prescription of long-acting beta-agonists and medium-dose inhaled corticosteroids. However, these measures did not provide relief. In 2021, the family observed abnormal breathing sounds, specifically a biphasic stridor sound, which could not be attributed to a typical asthma case. Approximately a year later, she was admitted to another hospital due to a viral infection that exacerbated dyspnea, non-productive cough, and fever. A chest x-ray was performed as part of her treatment, leading the pediatrician to recommend further evaluation and consultation with a pediatric pulmonologist.
2.2. Past Medical History
The patient is a 13-year-old girl, the eldest child in the family, born full-term via cesarean section and breastfed for two years. There was no need for NICU admission at birth, and she received all her immunizations through the Iranian national vaccination program. She has been experiencing dyspnea and coughing since the age of four and denied any other health issues since birth.
2.3. Family History
Her parents did not mention any significant history of illnesses. Her brother has a small, flat hemangioma measuring 1 cm by 1 cm on his lower back, and he does not experience any respiratory symptoms.
2.4. Physical Examination
She was a 12-year-old girl who was alert and oriented, providing responses to questions. Her weight (62 kg) and height (161 cm) fell within the normal range, resulting in a BMI of 23.9 kg/m². During lung auscultation, a biphasic stridor was detected with a stethoscope, though it was not audible without the instrument. No signs of chronic or acute hypoxia, such as finger clubbing, were observed in her physical examination. Her heart auscultation was entirely normal. The biphasic stridor had been noted in her lung auscultation since the onset of symptoms at the age of four, as indicated in her medical records. No other significant findings were identified in the physical examination.
2.5. Lab Data
Normal results were obtained for the complete blood count, liver function test, C-reactive protein, urinalysis, sputum culture, urine analysis and culture, arterial blood gas (ABG), and electrocardiogram (ECG).
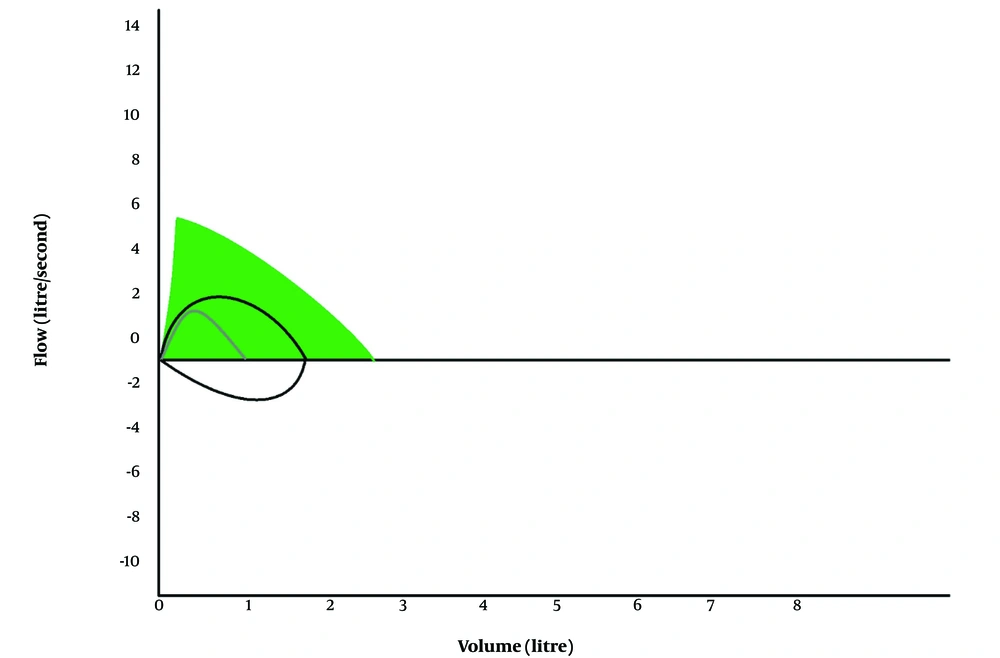
2.6. Spirometry
The spirometry reveals a large airway obstruction rather than the involvement of small airways, noted as fixed during both the inspiration and expiration phases. This spirometry pattern strongly suggests the presence of tracheal issues (Figure 1).
2.7. Differential Diagnosis
At the forefront of the differential diagnoses are tracheal abnormalities, encompassing tracheomalacia and tracheal obstruction. This obstruction may result from an intra-tracheal tumor. Conversely, it could be attributed to an extra-tracheal tumor in adjacent tissues, exerting pressure on the trachea. Intra-tracheal issues might involve subglottic stenosis, hemangioma, complete tracheal ring, or an inhaled foreign body.
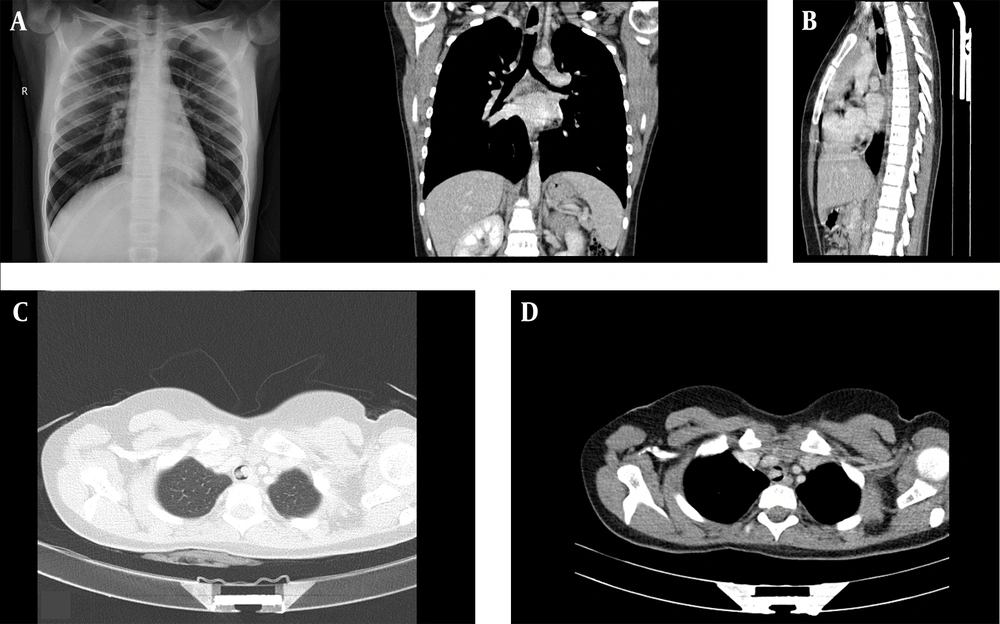
2.7.1. Imaging
To differentiate between diagnoses, a spiral chest CT with IV contrast and a chest X-ray were conducted. The chest X-ray revealed bilateral lung emphysema (Figure 2). The CT scan identified a 10 × 7 mm polypoid intra-tracheal lesion located anteriorly, leading to severe tracheal narrowing. The aortic arch exhibited a regular branching pattern, with no stenosis, abnormal dilatation, or filling defect observed in the thoracic arteries. The tumor showed no signs of blood overflow, and there was no evidence of tracheal invasion, making interventional bronchoscopic excision feasible.
A, chest X-ray: Both sides show a downward displacement of the diaphragm, and bilateral lung emphysema is evident. B, sagittal section of the thoraco-abdominal CT scan. C, the axial section of the thoraco-abdominal CT scan (parenchymal view) indicates almost complete trachea blockage. D, axial section of the thoraco-abdominal CT scan (mediastinal view).
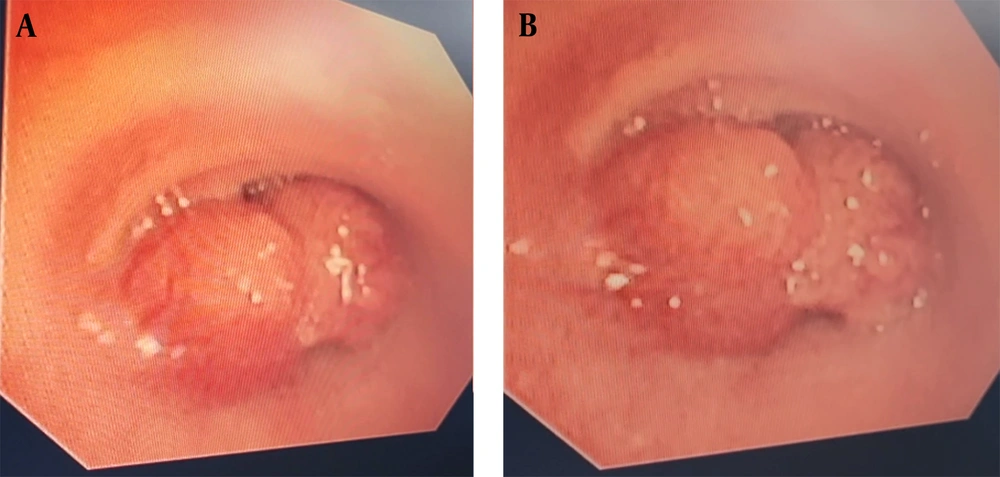
2.7.2. Bronchoscopy
In the subsequent step, a flexible bronchoscopy was performed, revealing approximately 90% airway obstruction in the trachea (Figure 3). This obstruction was attributed to 2 tumors located in the upper third of the trachea, situated on the lateral walls on both sides. One of the lesions had a heterogeneous wall, while the other exhibited a smooth wall. Both tumors were found to be vascular.
2.7.3. Surgical Intervention
The patient was referred to the interventional bronchoscopy center. The anesthetist recommended midazolam and propofol to relax the muscles while maintaining spontaneous breathing. During the bronchoscopy procedure, a flexible probe was inserted, revealing 2 tumors in the upper third of the trachea on the lateral walls of both the right and left sides, causing 90 percent airway obstruction. The appearance of the tumor suggested it could be a hemangioma, hemangiopericytoma, inflammatory pseudotumor respirator, Langerhans cell histiocytosis, juvenile xanthogranuloma, or papilloma. To resect the tumor, the pedicles of the tumors were cauterized with a cutter and subsequently removed using forceps.
2.7.4. Clinical Diagnosis
The clinical diagnosis confirms the presence of a primary tracheal tumor. Imaging and pathological assessments did not reveal any signs of malignancy. From an epidemiological standpoint, the most likely primary intra-tracheal tumor is Mucous Gland Adenoma (MGA). There was no indication of mass penetration into the surrounding tissues or involvement of other organs.
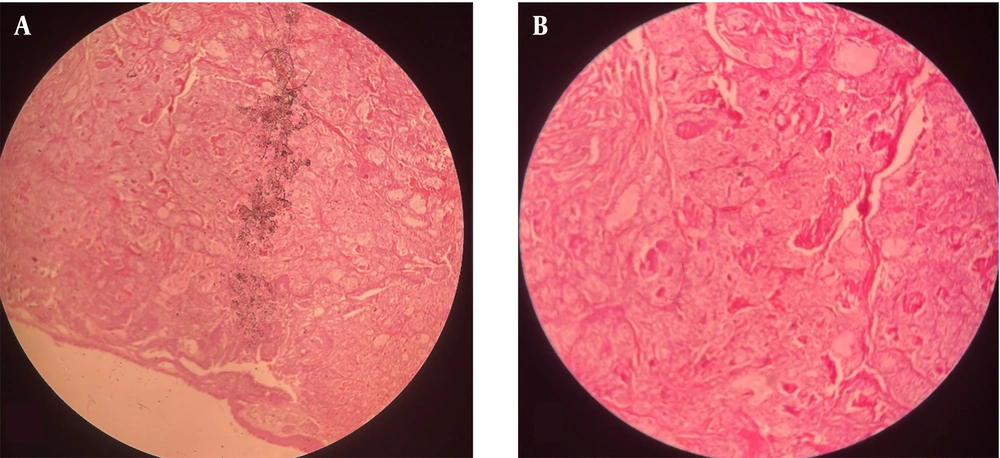
2.7.5. Pathology
In its gross appearance, the specimen received in formalin comprises a fragment of elastic tissue measuring 1.5 × 1.1 × 0.5 cm. Under the microscope, the specimen resembles small round blue cells, confirming the epithelioid nature of the tumor cells. There was no evidence of cancer, and mitosis was not observed. Immunohistochemical studies using electron microscopy were conducted to identify IHC markers. In this study, P63 was positive in the basal layer of surface epithelium and scattered neoplastic cells. Chromogranin and synaptophysin were negative, while CEA was positive in a few neoplastic cells. The glandular epithelium tested negative for TTF1, TG, calcitonin, and PAX8 (Figure 4).
2.8. Follow-up
She had 2 follow-up visits, one after approximately three months and another after approximately 6 months. During both visits, she remained completely symptom-free, and no pathology was detected in her physical examination. On her second visit, a follow-up spirometry was conducted, revealing complete normalcy with no signs of recurrence.
3. Discussion
Intra-tracheal tumors are rare, particularly when compared to bronchial or lung tumors. The majority of these tumors are malignant, including squamous cell carcinoma and adenoid cystic carcinoma. Non-malignant tumors primarily consist of papillomas, hamartomas, hemangiomas, and MGAs. Additionally, there is a small group of rare tumors known as neurogenic tumors, including neurofibromas and neurilemmomas (5, 6). Primary intra-tracheal tumors typically manifest nonspecific symptoms in the early stages. However, as they grow and obstruct over half of the tracheal lumen, symptoms of airway blockage such as dyspnea, coughing, and stridor sound of breathing emerge (7).
Mucous gland adenoma (MGA) are rare tumors originating from mucous-secreting glands, mainly from the large airway mucosa. Most arise from the main, lobar, or segmental bronchi and rarely from the trachea (8, 9). Pathologically, MGAs consist of mucus-secreting components of tracheobronchial seromucinous glands, typically presenting as an endobronchial, multicystic, well-circumscribed tumor (10). The nonspecific nature of signs and symptoms can lead to misdiagnosis, with approximately half of the patients initially misdiagnosed with asthma, leading to delayed diagnosis and treatment (11).
Treatment with glucocorticoids or bronchodilators can provide temporary relief in the early stages. However, as dyspnea persists, radiographic techniques aid in diagnosing the tumor (7). Spirometry testing reveals a pattern of upper airway fixed obstruction in both inspiration and expiration phases, showing no proper response to bronchodilators (12). To prevent misdiagnosis, radiographic techniques should be employed in all cases without proper responses to treatment. Chest X-rays may not effectively show the tumor, especially when done anteroposteriorly due to the coverage of mediastinal soft tissues (13). CT scans help define the pathology and its relation to other structures (12). Bronchoscopy is valuable in the diagnosis, allowing for biopsy collection for pathological studies. Tumor resection can be achieved through flexible bronchoscopy or other surgical interventions. Subsequently, a tumor biopsy is sent for pathological studies to determine the exact origin and type of the tumor. The malignancy and recurrence of intra-tracheal tumors vary based on the nature of the tumor (6). In our patient, there was no tumor recurrence 6 months after surgery. The preferred treatment is complete excision of MGA, which may involve the bronchus, segment, or lobe (14).
3.1. Conclusions
In conclusion, intra-tracheal mucoepidermoid tumors are uncommon, and their presentation is size-dependent, lacking specificity. It is crucial to assess asthmatic patients who do not respond adequately to treatment for potential underlying complications. Radiological methods can be beneficial for all patients with complex presentations and those not responding properly to treatment. Bronchoscopy aids in diagnosis, biopsy, and tumor resection. Long-term monitoring is essential to detect any potential tumor recurrence.