1. Background
According to the World Health Organization (WHO), psychiatric disorders are the leading cause of disability among youth. These conditions impact children's development, academic performance, and their potential to lead productive and fulfilling lives (1). A review of several studies (published from 2000 to 2007) in the US found that approximately one-third of children and adolescents experience a psychiatric disorder during their lifetime, and about one-fourth experience one within the last year (2). In a study by Riahi et al. on a community sample of children and adolescents in Khuzestan province, 22.66% of participants were diagnosed with at least one psychiatric disorder (3).
The COVID-19 outbreak has presented parents with significant challenges in the field of child and adolescent psychiatry. It has disrupted the daily routines of everyone, including children and adolescents (4-9). In Iran, as in other countries, routine services have been limited. Numerous public and clinical services, including schools, social services, psychiatric offices, and others, have been restructured or closed to reduce close social contact.
The pandemic and the associated limitations are expected to result in a variety of consequences for children and adolescents (9-11). Mental health responses include boredom, isolation, uncertainty, anxiety, depression, and post-traumatic symptoms among children and adolescents (9-11). They may also experience fear and grief-related symptoms due to the impact of the virus on their families (12). These effects are especially significant for youth with psychiatric disorders; the pandemic may also worsen specific types of disorders, such as OCD, GAD, and specific phobias (10, 12). In a study in the UK, 83% of adolescents (including 61% with ongoing mental health difficulties) reported that the pandemic had worsened their mental health (13). In a study on patients with eating disorders, Davis et al. found an increase in health-related anxiety related to COVID-19 (14). Individuals with attention deficit hyperactivity disorder (ADHD) may also exhibit more behavioral problems (15), and patients with autism spectrum disorder (ASD) may have greater difficulty adjusting to disruptions in daily life routines (16).
It has also been suggested that psychotic disorders and suicide may result from the fear of COVID-19, especially in individuals who have previously experienced psychiatric disorders (17). The disruption of mental health care is another important concern for patients with psychiatric disorders and their families (11).
On the other hand, home confinement may trigger domestic violence during the COVID-19 outbreak (11), and domestic violence predicts children's psychopathology (18). Moreover, children and adolescents with psychiatric disorders are at greater risk for neglect or abuse when they live in homes where intrafamilial violence occurs.
2. Objectives
Based on the above premises, it is essential to assist parents in coping constructively with difficulties related to their children during the COVID-19 pandemic. To achieve this, the responses of children and their families to this crisis should be understood. The present study aimed to investigate the difficulties faced by families with children and adolescents who have psychiatric disorders during the COVID-19 outbreak.
3. Methods
The investigation was a descriptive cross-sectional study conducted from 2020 to 2021. A total of 92 children and adolescents (age range: 2 - 18 years; mean age: 9.49 ± 4.72) diagnosed with psychiatric disorders were selected from an outpatient clinic specializing in child and adolescent psychiatry in Ahvaz, Iran, using judgmental sampling.
The diagnosis of psychiatric disorders was confirmed by a child and adolescent psychiatrist based on the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) criteria. After explaining the procedures and purpose of the study, the parents (father or mother) of the children were asked to complete an informed consent form, a questionnaire to obtain demographic data, and a questionnaire to gather information about parents’ difficulties with their children and adolescents during the COVID-19 pandemic and the existing restrictions. The history of psychiatric disorders in parents was also checked with a specific question. Approximately 95% of the questionnaires were completed by the children’s mothers. It should be noted that the data was gathered by a trained psychologist.
The inclusion criteria were an age range of 2 to 18 years and the completion of informed consent by parents. The exclusion criterion was the inability to take a precise history due to the absence of a parent or primary caregiver with detailed information about the child. One child was excluded from the study because they were brought to the clinic by their aunt. The sample size was calculated using the following formula:
3.1. Instruments
To diagnose psychiatric disorders, a clinical interview was used. It was conducted by a child and adolescent psychiatrist based on DSM-5 criteria.
A researcher-made questionnaire was used to measure the difficulties faced by families with children and adolescents who have psychiatric disorders. The questionnaire consists of 10 sections, including access to clinical services; worsening of symptoms; changes in eating patterns (overeating); changes in physical activity (inactivity); overweight (resulting from overeating and inactivity); hygiene issues; alcohol, smoking, and substance use; education (academic issues and the use of virtual education); media (excessive use of social media); sleep problems; and communication with family members. The severity of each problem, conflicts with the child regarding the problem, and conflicts with the spouse concerning the child’s problem are assessed in each item.
To assess the validity of the questionnaire, it was reviewed by an expert panel, and the face validity of the questionnaire was well supported. Reliability was assessed using Cronbach’s alpha, and the questionnaire demonstrated high internal consistency (α = 0.7) across different sections.
3.2. Data Analysis
Data were analyzed using descriptive statistics (to summarize and describe the distribution of the dataset), the chi-squared test, and Fisher’s exact test (to compare the distribution of categorical variables in two groups). Gender was identified as a potential confounder; therefore, we compared samples of men and women separately to provide more clarity in the research. A probability level of 0.05 was accepted as statistically significant. Statistical analyses were conducted using SPSS 16 software.
4. Results
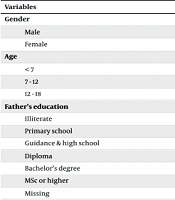
The demographic characteristics of participants and the distribution of psychiatric disorders are presented in Tables 1, and 2, respectively. As shown in Table 3, the most common challenges that parents faced were sleep problems (disruption of the sleep-wake cycle; 58.7%), excessive use of media (54.3%), and significant challenges with eLearning (53.33%).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 66 (72.5) |
| Female | 23 (25.3) |
| Age | |
| < 7 | 29 (31.5) |
| 7 - 12 | 25 (27.2) |
| 12 - 18 | 35 (38.0) |
| Father’s education | |
| Illiterate | 1 (1.1) |
| Primary school | 6 (6.5) |
| Guidance & high school | 3 (3.3) |
| Diploma | 32 (34.8) |
| Bachelor’s degree | 33 (35.9) |
| MSc or higher | 9 (9.8) |
| Missing | 8 (8.7) |
| Mother’s education | |
| Illiterate | 2 (2.2) |
| Primary school | 4 (4.3) |
| Guidance & high school | 5 (5.4) |
| Diploma | 36 (39.1) |
| Bachelor’s degree | 29 (31.5) |
| MSc or higher | 14 (15.2) |
| Missing | 2 (2.2) |
| Father’s job | |
| Public sector | 46 (50.0) |
| Private sector | 37 (40.2) |
| Unemployed | 1 (1.1) |
| Missing | 8 (8.7) |
| Mother’s job | |
| Public sector | 17 (18.5) |
| Private sector | 16 (17.4) |
| Unemployed (housewife) | 55 (59.8) |
| Missing | 4 (4.3) |
| History of psychiatric disorder in parents of children | |
| Father | |
| Yes | 18 (19.6) |
| No | 68 (73.9) |
| Missing | 6 (6.5) |
| Mother | |
| Yes | 11 (12.0) |
| No | 75 (81.5) |
| Missing | 86 (6.5) |
| Total | 92 (100) |
| Variables | No. (%) |
|---|---|
| ADHD | 22 (24) |
| ADHD + intellectual disability | 2 (2.2) |
| ADHD + LD | 2 (2.2) |
| ADHD + anxiety disorder | 4 (4.4) |
| ADHD + anxiety disorder + depression | 2 (2.2) |
| ADHD + depression | 1 (1.1) |
| ADHD + OCD | 4 (4.4) |
| ADHD + OCD + LD | 2 (2.2) |
| ADHD + OCD + Tic | 1 (1.1) |
| ADHD + ODD | 6 (6.6) |
| ADHD + ODD + anxiety disorder | 1 (1.1) |
| ADHD + CD | 1 (1.1) |
| ADHD + PTSD | 2 (2.2) |
| ADHD + Tic | 1 (1.1) |
| ADHD + Tic + anxiety disorder | 1 (1.1) |
| ADHD + Tic + BMD | 1 (1.1) |
| ADHD + SAD + pathological masturbation | 1 (1.1) |
| ASD | 12 (13.2) |
| ASD + ADHD | 6 (6.6) |
| GAD | 1 (1.1) |
| Social phobia | 3 (3.3) |
| Anxiety disorder + Tic | 1 (1.1) |
| Anxiety disorder + trichotillomania | 1 (1.1) |
| BID | 3 (3.3) |
| MDD + GAD | 1 (1.1) |
| Mood + anxiety disorder | 3 (3.3) |
| OCD | 3 (3.3) |
| OCD + depression + anxiety disorder | 1 (1.1) |
| OCD + schizophrenia | 1 (1.1) |
| Impulsivity control disorder + paranoia | 1 (1.1) |
Abbreviations: LD, learning disorder; OCD, obsessive compulsive therapy; ODD, oppositional defiant disorder; CD, conduct disorder; PTSD, post-traumatic stress disorder; BMD, borderline mood disorder; ASD, autism spectrum disorder; GAD, generalized anxiety disorder; BID, bipolar I disorder; MDD, major depression disorder.
| Difficulty | No. (%) |
|---|---|
| Access to clinical services | |
| Difficulty in finding medication | |
| Yes | 6 (6.5) |
| No | 80 (87.0) |
| Missing | 6 (6.5) |
| Difficulty in access to psychiatrist | |
| Yes | 30 (32.6) |
| No | 56 (60.9) |
| Missing | 6 (6.5) |
| Difficulty in access to other therapists (psychologist, speech therapist, physiotherapist, occupational therapist, and etc.) | |
| Yes | 22 (23.9) |
| No | 58 (63.0) |
| Missing | 12 (13.0) |
| Change in symptoms of the psychiatry disorder | |
| Worsening of symptoms | |
| Yes | 22 (23.9) |
| No | 58 (63.0) |
| Missing | 12 (13.0) |
| Return of symptoms | |
| Yes | 20 (21.7) |
| No | 47 (51.1) |
| Missing | 25 (27.2) |
| Change in eating pattern (overeating) | |
| Yes | 27 (29.3) |
| No | 56 (60.9) |
| Missing | 9 (9.8) |
| Change in physical activity (inactivity) | |
| Yes | 38 (41.3) |
| No | 44 (47.8) |
| Missing | 10 (10.9) |
| Overweight (because of overeating or inactivity) | |
| Yes | 23 (25.0) |
| No | 56 (60.9) |
| Missing | 13 (14.1) |
| Hygiene issues | |
| Lack of hygiene | |
| Yes | 24 (26.1) |
| No | 51 (55.4) |
| Missing | 17 (18.5) |
| Alcohol /smoking /substance use | |
| Yes | 3 (3.3) |
| No | 81 (88.0) |
| Missing | 8 (8.7) |
| Education (academic issues and the use of virtual education) | |
| Yes | 32/60 (53.33) |
| No | 22/60 (36.66) |
| Missing | 8/60 (13.33) |
| Media | |
| Excessive use of social media | |
| Yes | 50 (54.3) |
| No | 34 (37.0) |
| Missing | 8 (8.7) |
| Sleep problems | |
| Disruption of the sleep-wake cycle | |
| Yes | 54 (58.7) |
| No | 30 (32.6) |
| Missing | 8 (8.7) |
| Nightmare | |
| Yes | 16 (17.4) |
| No | 68 (73.9) |
| Missing | 8 (8.7) |
| Difficulties related to communication with family members | |
| Problem with siblings | |
| Yes | 18 (19.6) |
| No | 58 (63.0) |
| Missing | 16 (17.4) |
| Problems with parents | |
| Yes | 24 (26.1) |
| No | 53 (57.6) |
| Missing | 15 (16.3) |
Inactivity (41.3%), difficulty accessing a psychiatrist (32.6%), difficulty accessing other therapists (23.9%), and worsening symptoms (23.9%) were the next most prevalent challenges.
Among parents of children with disruption in the sleep-wake cycle, 80.8% reported that this issue caused conflict with their children (conflict intensity: 25.6% low; 41.9% moderate; 30.2% high; 2.3% very high). Among these parents, 31.9% reported conflict with their spouses over the sleep problem of their child.
Among parents whose children had excessive use of social media (n = 50), 83.5% reported parent-child conflict over this issue (conflict intensity: 36.6% low; 36.6% moderate; 22% high; 4.9% very high), and 33.3% reported spouse conflicts (conflict intensity: 45.5% low; 27.3% moderate; 27.3% high).
Among parents of children with educational problems, 79.3% reported conflict with their child over this issue (conflict intensity: 27.3% low; 36.4% moderate; 27.3% high; 9.1% very high). In 21.73% of these children, the issue resulted in conflict between the parents (conflict intensity: 40% low; 20% moderate; 40% high).
Among the parents, 18 fathers (19.6%) and 11 mothers (12%) reported a history of psychiatric disorders (Table 1). A history of psychiatric disorders in parents did not predict parent-child conflict over the children’s problems during the quarantine (all P > 0.05; Table 4). A history of psychiatric disorders in parents also did not predict spousal conflict over the children’s problems during the quarantine (all P > 0.05; Table 5).
| Variables | History of Psychiatric Disorder in Father | Sig. | OR | CI 95 | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Parent-child conflict over media use | 0.3 | 0.84 | 0.96 - 0.74 | ||
| Yes | 6 | 33 | |||
| No | 0 | 8 | |||
| Parent-child conflict over academic problems | 0.59 | 0.9 | 1.03 - 0.78 | ||
| Yes | 2 | 19 | |||
| No | 0 | 6 | |||
| Parent-child conflict over sleep problems | 0.1 | 0.8 | 0.93 - 0.68 | ||
| Yes | 8 | 32 | |||
| No | 0 | 9 | |||
| History of psychiatric disorder in mother | |||||
| Parent-child conflict over media use | 0.45 | 2.06 | 0.22 - 19.35 | ||
| Yes | 10 | 29 | |||
| No | 1 | 6 | |||
| Parent-child conflict over academic problems | 0.1 | 0.11 | 1.54 - 0.008 | ||
| Yes | 1 | 18 | |||
| No | 2 | 4 | |||
| Parent-child conflict over sleep problems | 0.58 | 0.84 | 4.88 - 0.14 | ||
| Yes | 8 | 33 | |||
| No | 2 | 7 | |||
| Variables | History of Psychiatric Disorder in Father | Sig. | OR | CI 95 | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Spouses conflict over media use in child | 0.1 | 3.54 | 0.51 - 24.25 | ||
| Yes | 3 | 11 | |||
| No | 2 | 26 | |||
| Spouses conflict over academic problems in child | 0.7 | 1.14 | 0.95 - 1.37 | ||
| Yes | 0 | 3 | |||
| No | 2 | 14 | |||
| Spouses conflict over sleep problems in child | 0.14 | 3.39 | 0.65 - 17.69 | ||
| Yes | 4 | 11 | |||
| No | 3 | 28 | |||
| History of Psychiatric Disorder in Mother | |||||
| Spouses conflict over media use in child | 0.36 | 1.76 | 0.38 - 7.98 | ||
| Yes | 4 | 10 | |||
| No | 5 | 22 | |||
| Spouses conflict over academic problems in child | 0.7 | 1.14 | 0.95 - 1.37 | ||
| Yes | 0 | 3 | |||
| No | 2 | 14 | |||
| Spouses conflict over sleep problems in child | 0.3 | 1.89 | 0.42 - 8.4 | ||
| Yes | 4 | 11 | |||
| No | 5 | 26 | |||
5. Discussion
The purpose of this study was to highlight the challenges faced by families of children and adolescents with psychiatric disorders during the COVID-19 outbreak, with the aim of providing clinicians and behavioral scientists with useful insights. We hope this will stimulate subsequent efforts to alleviate the burden of the pandemic on these families. The most common challenges that parents faced were sleep problems (disruption of the sleep-wake cycle), excessive use of media, and significant challenges with eLearning.
Regarding the disruption of the sleep-wake cycle, it is recommended to educate parents (especially mothers) and/or children on sleep hygiene and stimulus control, or to use cognitive-behavioral therapy or pharmacotherapy as needed (19-27).
Some of the challenges parents faced with their children's education included the child's/adolescent's adaptation to eLearning, an inadequate learning environment, the lack of structure at home during self-isolation, difficulties with self-motivation and self-discipline, low computer literacy, and technical issues (28, 29).
Several studies have offered suggestions to address these challenges. For example, Shahzad et al. noted that the quality of the system and the quality of information are directly related to students' satisfaction with eLearning (28). Nabih et al. found that eLearning could be improved by making it more interactive (30), and Soni suggested designing detailed lesson plans to create satisfactory study materials (29).
Guidance has also been provided for parents and caregivers of children who are learning at home through virtual education during the COVID-19 pandemic. However, this guidance is insufficient for children and adolescents with psychological disorders. Mental health professionals should educate parents on how to effectively manage their children's education. For example, parents can create a structured learning environment at home, involve both parents in the child/adolescent's educational program, and stay in touch with the child's teacher, asking for cooperation to increase supervision over their children.
Most parents reported excessive media use in their children, particularly among teenagers. This finding is consistent with studies (31, 32) that report the overuse of digital technologies in children and adolescents as an outcome of the COVID-19 pandemic. A longitudinal study conducted by Zhou et al. suggests that individuals with ADHD are more likely to overuse the internet. These tendencies could be heightened during lockdowns, social distancing, and in-home confinement related to COVID-19 (33, 34).
Since excessive screen time may lead to detrimental consequences in youth, such as psychopathological states, reduced empathic skills, lower social competencies, and diminished motor skills (35-37), it is important to help parents find the right balance—specifically, how to reduce screen time in children and adolescents during the pandemic—and to monitor the potentially harmful aspects of their behavior. Parental supervision of children’s media use is a key factor in determining desirable programming, fostering positive outcomes from media use, controlling harmful effects, and regulating appropriate media use durations (38). Children should be allowed to use media under the supervision of their parents. Therefore, educating parents on how to monitor and manage their children’s media use is essential.
Another challenge for parents during the outbreak was a change in physical activity, specifically inactivity. Encouraging children to be active within the constraints of existing restrictions is recommended. Some parents also reported temporarily losing access to clinical services, trained caregivers, or community service providers. Therefore, it is crucial to plan and advocate for resources and services that deliver high-quality psychiatric care. In Iran, mental health professionals have considered telepsychiatry as a means of delivering services to minimize patients' exposure to hospitals and other mental health centers. People are also encouraged to seek support through telehealth services. It is urgent to ensure that clients have access to the internet and necessary devices.
One-fifth of the responders reported a return of symptoms, and about a quarter reported a worsening of symptoms in their child. This may be due to difficulties in adjusting to lockdown, fear of infection, and/or disruption of professional mental health care. Parent-focused interventions and/or patient-focused non-pharmacological interventions should be implemented, and the risks and benefits of pharmacological treatment under the COVID-19-specific situation should also be considered (39).
When addressing individuals with intellectual and neurodevelopmental disabilities, social distancing during COVID-19 has had a disproportionate impact. These individuals have been disproportionately isolated during the pandemic (40). While people around the world have embraced virtual interactions, screen-based technologies are inadequate substitutes for individuals with intellectual and neurodevelopmental disabilities. These individuals may also not benefit from electronic substitutes for education and therapy (40). Special education for this community often requires interpersonal prompting, nuanced physical contact and redirection, close attention to the motivational structure of the environment, and enhanced teacher-to-student ratios. It places a disproportionate burden on families to attempt to replicate the conditions of an “appropriate” education at home and to prevent negative outcomes such as individuals with disabilities falling behind in training or academic achievement and struggling to compensate behaviorally in the absence of the structure provided by school (40). The burden of COVID-19 on individuals with intellectual and neurodevelopmental disabilities should receive more attention from clinicians, scientists, and advocates. They should recognize and seek opportunities to mitigate the burden of COVID-19 on this community.
Our results did not confirm an association between parental psychiatric disorders and an increased risk of child-parent conflict or spouse conflict over the problems of the children. This finding may be due to the use of a self-report measure to assess parental psychopathology, or psychopathological symptoms may be underdiagnosed in some parents. Further studies are recommended to determine the precise relationship between these two conditions using more reliable assessment instruments.
5.1. Conclusions
In conclusion, the COVID-19 pandemic and its limitations are expected to result in a variety of consequences for children and adolescents. These consequences are particularly significant for youth with psychiatric disorders. Therefore, it is essential to support families with children and adolescents who have psychiatric disorders. The main objective of this research was to investigate the burden of the COVID-19 pandemic on these families. The most common challenges that parents faced were sleep problems, excessive use of media, and significant challenges with elearning. Inactivity, difficulty accessing psychiatrists and other therapists, and worsening of symptoms were the second most prevalent issues.
Based on these results, it is the responsibility of mental health professionals, scientists, and advocates to recognize the opportunity to alleviate the burden of COVID-19 on children and adolescents with psychiatric disorders and their families.
The findings should be interpreted in the context of several limitations. The sample size was relatively small; future research with a larger sample size is recommended. Moreover, the majority of the participants were women, which affects the generalizability of the findings. Another limitation of the study is the sampling method (i.e., convenience sampling); therefore, the findings should be generalized to other populations with caution. Finally, the study sample consisted of children and adolescents with psychiatric disorders, meaning the findings should be generalized to other age groups or healthy individuals with caution. These limitations should be addressed in future research.