1. Background
Chronic constipation in childhood is a widespread issue affecting children globally, with prevalence rates varying from 0.7% to 29.6% (1). The majority of these cases, over 90%, are identified as functional constipation, which is marked by symptoms such as abdominal pain, infrequent bowel movements, and fecal incontinence (2). The chronic nature of this condition and its interference with daily life significantly impact various aspects of a patient's quality of life, including physical, social, familial, and psychological facets (3).
Research has linked chronic functional constipation to interruptions in preschool education, difficulties in forming social connections, especially with peers, and cognitive disturbances (4, 5). Review articles have further highlighted a considerable occurrence of atypical behavioral patterns, including aggression, irritability, sleep disruptions, and temper tantrums among children dealing with chronic functional constipation (6). Moreover, a connection has been noted between defecation habits and the severity of behavioral issues in children, particularly those of preschool age (7). Notably, an increasing severity and frequency of behavioral problems have been directly correlated with the lengthening intervals between effective bowel movements (8).
Despite these insights, numerous questions about the specific behavioral disorders and their contributing factors in children with chronic functional constipation remain unanswered.
2. Objectives
This study aimed to examine behavioral disorders in children with chronic functional constipation and identify the primary factors influencing these conditions.
3. Methods
3.1. Study Design
This case-control study was conducted on children and adolescents aged 2 to 18 with chronic functional constipation who visited the gastroenterology clinic of Bahrami Children's Hospital in Tehran between 2019 and 2020. The inclusion criteria were children and adolescents aged 2 to 18 years presenting with two or more of the following symptoms for over two months: Defecation frequency of two times a week or less, incontinence of once a week or more, avoidance of defecation (withholding), history of painful defecation, and fecal impactions detected in the rectum. The exclusion criteria encompassed identifying any underlying organic causes either at the onset or during the treatment process by the pediatric gastroenterologist. Individuals with pre-existing chronic conditions, internal, neurological (chronic or acute), acute neurological diseases as reported by the parents, those diagnosed with mental retardation, and families wishing to withdraw from the study were excluded.
3.2. Study Population
The control group consisted of children who visited the gastroenterology clinic of the hospital for reasons other than chronic functional constipation.
Functional constipation was defined as a defecation frequency of fewer than three times per week without a palpable abdominal or rectal mass and without any organic causes for constipation found during the physical examination (9). The exclusion criteria for the study included children with constipation due to neurological, hormonal, medicinal, dietary, metabolic, and anatomical causes, patients with diseases unrelated to constipation, those with other chronic and acute diseases, and cases of mental retardation as reported by parents and confirmed by a specialist doctor or documented in the medical record.
3.3. Data Collection
Data was gathered using a questionnaire overseen by the project manager. The questionnaire comprised two sections: The first section collected demographic information about the child, including age, gender, and reason for referral. The second section focused on detailing the child's condition, clinical assessments, and results from paraclinical tests for children with ongoing hard stools or irregular bowel movements lasting more than two weeks. Additionally, the Strengths and Difficulties Questionnaire (SDQ) was administered, consisting of two parental versions and a self-report version for adolescents aged 11 years and older. This questionnaire is divided into two forms: One for children under 11 years, filled out by their parents due to the children's inability to complete it independently, and a self-report form for those over 11 years and teenagers. The SDQ assesses behavioral symptoms in children and adolescents through 25 questions, evaluating five emotional aspects: Emotional symptoms (5 items), conduct problems (5 items), hyperactivity/inattention (5 items), peer relationship problems (5 items), and prosocial behavior (5 items). Each psychological attribute is rated on a scale from 0 to 10, with a score of 0 representing the most favorable outcome for emotional, conduct, hyperactivity, and peer relationship areas. (These four attributes contribute to a total difficulties/overall stress score ranging from 0 - 40.) Conversely, prosocial behavior is scored oppositely, where a score of 10 indicates the least difficulty. Furthermore, the parental version of the questionnaire is rated from 0 to 13 (normal), 14 to 16 (borderline), and 17 to 40 (abnormal), while the adolescent version ranges from 0 to 15 (normal), 16 to 19 (borderline), and 20 to 40 (abnormal). In research by Ghanizadeh and Izadpanah on the Persian version of the SDQ, the self-report scales showed good internal consistency, achieving a final Cronbach’s alpha reliability coefficient of 0.628 (10). They also confirmed adequate convergent and discriminant validity for the questionnaire. Gender, age, and overweight status were examined as potential factors influencing behavioral issues. Overweight was determined by a body mass index for age exceeding 1 standard deviation above the World Health Organization (WHO) Growth Reference median.
3.4. Ethical Considerations
Given the involvement of human participants, written consent was obtained from all individuals participating in the study. Participation was entirely voluntary, without any form of coercion. All information gathered through the questionnaire was kept confidential and not disclosed under any circumstances. Participants were thoroughly informed about the research topic and received detailed explanations regarding their participation, ensuring they had ample time to make an informed decision. It was also made clear that their participation was optional, and choosing not to participate would not affect their access to standard services. As the study included children who were not capable of making legal decisions, consent was obtained from their legal guardians, typically the child's father. The research was carried out with the approval of the ethics committee of Tehran University of Medical Sciences under the ethics code IR.TUMS.CHMC.REC.1399.166.
3.5. Statistical Analysis
For the statistical analysis, results were presented as mean ± standard deviation (SD) for quantitative variables and summarized as frequency (percentage) for categorical variables. Continuous variables were compared using the t-test or Mann-Whitney test, depending on whether the data deviated from a normal distribution or if the assumption of equal variances was not met across study groups. Categorical variables were analyzed using the chi-square test or Fisher’s exact test as required. P-values of ≤ 0.05 were considered indicative of statistical significance. The analysis was conducted using SPSS software, version 23.0 for Windows (IBM, Armonk, New York).
4. Results
The study included 107 children diagnosed with chronic functional constipation and 107 control participants without this condition. Analysis of various behavioral components using the SDQ between the cases and controls showed that children with chronic functional constipation had significantly higher average scores for emotional symptoms (0.85 ± 0.81 vs. 0.55 ± 1.03, P = 0.019), peer relationship problems (1.76 ± 2.23 vs. 0.76 ± 1.18, P = 0.001), and prosocial behavior (8.12 ± 1.87 vs. 7.42 ± 1.64, P = 0.002). However, no significant differences were observed in the scores for conduct problems (0.93 ± 0.81 vs. 1.00 ± 0.72, P = 0.478) and hyperactivity/inattention (3.11 ± 5.48 vs. 2.41 ± 3.12, P = 0.252) between the two groups.
When comparing behavioral problems between the case and control groups by age (Table 1), significant differences were found in the mean scores for peer relationship problems among children aged 5.1 to 8.0 years. Moreover, children over 8.0 years with chronic constipation had higher average scores for hyperactivity/inattention and prosocial behavior. This indicates that older children with chronic constipation are more likely to exhibit problems with hyperactivity/inattention and prosocial behavior, suggesting age is a critical factor for such issues.
| Items and Groups | Age (y) | P-Valueb | P-Value c | ||
| ≤ 5 | 5 - 8 | ≥ 8 | |||
| Emotional symptoms | 0.14 | ||||
| Case | 1.00 ± 0.80 | 0.34 ± 0.15 | 1.05 ± 0.65 | 0.224 | |
| Control | 0.85 ± 1.30 | 0.60 ± 1.27 | 0.32 ± 0.62 | 0.112 | |
| Conduct problems | 0.52 | ||||
| Case | 1.17 ± 2.39 | 0.15 ± 0.36 | 1.23 ± 0.43 | 0.326 | |
| Control | 1.30 ± 0.73 | 0.88 ± 0.74 | 1.02 ± 0.64 | 0.456 | |
| Hyperactivity/inattention | 0.001 | ||||
| Case | 2.39 ± 1.56 | 1.15 ± 1.64 | 3.41 ± 1.00 d | 0.002 | |
| Control | 2.45 ± 0.88 | 2.36 ± 1.75 | 1.72 ± 1.59 | 0.045 | |
| Peer relationship problems | 0.002 | ||||
| Case | 1.35 ± 0.89 | 3.23 ± 4.00 d | 0.42 ± 1.76 | 0.036 | |
| Control | 1.35 ± 0.93 | 0.60 ± 1.41 | 0.67 ± 0.85 | 0.012 | |
| Prosocial behavior | 0.02 | ||||
| Case | 8.51 ± 1.25 | 7.00 ± 2.92 | 8.35 ± 0.93 d | 0.012 | |
| Control | 7.95 ± 1.66 | 7.26 ± 1.90 | 7.35 ± 1.15 | 0.336 | |
a Values are expressed as mean ± SD.
b Inter-group comparison.
c Between-group comparisons.
d P ≤ 0.05 in comparing two groups with and without chronic constipation.
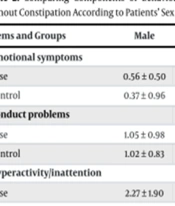
Gender analysis (Table 2) revealed that peer relationship problems were more common among male patients with chronic constipation than boys in the control group. Within the chronic constipation group, peer relationship issues were more frequently observed in males, whereas females displayed more challenges with prosocial behavior. Thus, gender also acts as a determinant for behavioral disturbances in children with chronic functional constipation.
| Items and Groups | Male | Female | P-Value b | P-Value c |
|---|---|---|---|---|
| Emotional symptoms | 0.22 | |||
| Case | 0.56 ± 0.50 | 1.10 ± 0.94 | 0.123 | |
| Control | 0.37 ± 0.96 | 0.67 ± 1.06 | 0.236 | |
| Conduct problems | 0.48 | |||
| Case | 1.05 ± 0.98 | 0.82 ± 0.60 | 0.422 | |
| Control | 1.02 ± 0.83 | 1.00 ± 0.62 | 0.729 | |
| Hyperactivity/inattention | 0.31 | |||
| Case | 2.27 ± 1.90 | 2.23 ± 1.40 | 0.546 | |
| Control | 2.47 ± 1.56 | 1.95 ± 1.58 | 0.145 | |
| Peer relationship problems | 0.01 | |||
| Case | 2.74 ± 2.82 d | 0.87 ± 0.81 | 0.002 | |
| Control | 0.84 ± 1.55 | 0.97 ± 0.89 | 0.146 | |
| Prosocial behavior | 0.11 | |||
| Case | 7.07 ± 2.02 | 9.07 ± 1.04 | 0.012 | |
| Control | 7.60 ± 1.46 | 7.29 ± 1.75 | 0.247 |
a Values are expressed as mean ± SD.
b Inter-group comparison.
c Between-group comparisons.
d P ≤ 0.05 in comparing two groups with and without chronic constipation.
Table 3 illustrates a comparison of behavioral issues between the case and control groups based on overweight status. A notable prevalence of hyperactivity/inattention was observed in overweight patients with chronic constipation compared to overweight children in the control group. Among children with chronic constipation, those who were overweight demonstrated more hyperactivity/inattention problems than their normal-weight counterparts. Therefore, overweight status significantly correlates with hyperactivity/inattention issues in children experiencing chronic constipation.
| Items and Groups | Overweight | P-Value b | P-Value c | |
|---|---|---|---|---|
| No | Yes | |||
| Emotional symptoms | 0.31 | |||
| Case | 0.80 ± 0.83 | 1.12 ± 0.61 | 0.225 | |
| Control | 0.55 ± 1.09 | 0.54 ± 0.73 | 0.256 | |
| Conduct problems | 0.42 | |||
| Case | 0.87 ± 0.85 | 1.25 ± 0.44 | 0.456 | |
| Control | 1.05 ± 0.72 | 0.81 ± 0.66 | 0.323 | |
| Hyperactivity/inattention | 0.003 | |||
| Case | 2.01 ± 1.61 | 3.60 ± 0.50 d | 0.001 | |
| Control | 2.19 ± 1.63 | 2.18 ± 1.55 | 0.226 | |
| Peer relationship problems | 0.02 | |||
| Case | 1.87 ± 2.44 | 1.12 ± 0.34 | 0.032 | |
| Control | 0.64 ± 1.63 | 2.18 ± 1.55 | 0.039 | |
| Prosocial behavior | 0.46 | |||
| Case | 8.05 ± 2.01 | 8.50 ± 0.73 | 0.723 | |
| Control | 7.32 ± 1.74 | 7.77 ± 1.18 | 0.656 | |
a Values are expressed as mean ± SD.
b Inter-group comparison.
c Between-group comparisons.
d P ≤ 0.05 in comparing two groups with and without chronic constipation.
5. Discussion
The potential influence of digestive disorders, particularly functional constipation, on the physical and psychological aspects of life quality in both childhood and adulthood, is well-documented. However, study outcomes have varied widely, mainly due to differences in the evaluation tools used, the age groups assessed, and the handling of background factors, especially confounders. Despite these variations, multiple studies agree on the profound impact of chronic functional constipation in children on psychological, behavioral, and cognitive facets. As evidenced in our research, constipation is strongly linked to various behavioral disorders, such as emotional issues, peer relationships, and prosocial behavior, but it has a lesser effect on conduct problems and hyperactivity/inattention. It has been noted that the evaluation tool utilized to measure behavioral dimensions significantly influences the detected behavioral patterns, all indicating the substantial impact of chronic constipation on these behaviors.
Karami et al., in a case-control study of children with functional constipation, identified a relationship between the condition and quality of life, noting a decrease in quality of life among children affected by this disorder (11).
El-Sonbaty et al., in 2019 (5), conducted psychological assessments using the Pediatric Symptom Checklist - 17, which includes internalizing and externalizing behavioral domains. Their findings revealed significant differences in these domains between children with and without functional constipation. Similarly, a study by Wang et al. in 2013 (12), which employed the Chinese versions of the PedsQL™ 4.0 Generic Core Scale and the Family Impact Module (FIM), showed that scores for physical, emotional, social, and school functions were significantly lower in children with functional constipation compared to their healthy counterparts. Additionally, Dos Santos et al., in 2021 (6), found a correlation between functional constipation and emotional symptoms and conduct problems using the SDQ questionnaire. Demographic characteristics might also play a role in the variability observed in behavioral pattern evaluations of these patients.
The pathophysiological mechanisms underlying the association between functional constipation and behavioral changes are not entirely clear but are believed to be multifactorial. Current understanding suggests that this relationship may be influenced by various neuropsychological factors, such as stress disorders, anorectal dysfunction, enteric nervous system defects, and central brain activity abnormalities (13). Previous research indicates that constipation might develop secondarily to other underlying psychological disorders that are closely related to the behavioral aspects of patients (13). The concept of a brain-gut axis has been proposed to explain the connection between chronic functional constipation and various behavioral disorders, particularly in children. Moreover, emerging evidence supports the existence of common links between the developmental pathways of the central and enteric nervous systems (14, 15). Overall, like other chronic conditions, the persistence of digestive disorders, especially functional constipation, may gradually disrupt the behavioral patterns of affected children.
Factors such as age, gender, and body weight may also influence the relationship between constipation and behavioral changes, as seen in this study. Some behavioral components appear to be affected by factors including older age, gender, and overweight status. Given the inherent differences in behavioral patterns among boys and girls, obese and non-obese children, and children and adolescents (16-18), it is reasonable to expect these factors to impact behavioral changes following chronic constipation.
5.1. Conclusions
In summary, chronic functional constipation in childhood can negatively impact various behavioral patterns, including emotional symptoms, peer relationships, and prosocial behavior, with variations observed based on the patient's gender, age, and body weight.