1. Background
Acute diarrhea is a significant cause of severe illness worldwide, particularly affecting children under the age of five. According to World Health Organization (WHO) statistics (1), it accounts for an estimated 1.3 million deaths annually, making it one of the leading causes of illness and mortality globally. Children under two years old are particularly vulnerable to this condition, which carries high rates of morbidity and mortality (2). In developing countries, children under three often experience at least three episodes of diarrhea each year (3). Notably, diarrhea is a leading cause of death among children under five, responsible for up to 25% of all pediatric deaths, with the highest prevalence in Africa and Southeast Asia (4).
One common complication of severe diarrhea is dehydration, which can lead to serious consequences such as shock, renal failure, electrolyte imbalance, and even death if not promptly identified and treated with fluid replacement (5). Proper and timely fluid replacement is crucial to preserving health and reducing the risk of mortality, especially in young children. Therefore, it is essential to monitor and promptly recognize early signs of dehydration to facilitate timely intervention and mitigate the likelihood of severe complications. Rapid identification of dehydration and implementation of appropriate intervention and treatment measures present significant challenges in clinical practice.
2. Objectives
This study aims to identify risk factors and develop a scoring system with an appropriate cutoff to estimate the likelihood of dehydration in children suffering from acute diarrhea.
3. Methods
3.1. Study Design and Data Collection
This case-control study included 34 children diagnosed with acute diarrhea and dehydration as cases, and 137 children diagnosed with acute diarrhea without dehydration as controls. The participants were admitted to the Gastroenterology Department of Can Tho Children's Hospital, the largest specialized pediatric hospital in the Mekong Delta region, southern Vietnam, between November 2022 and October 2023.
The inclusion criteria for cases were children aged 2 months to 5 years diagnosed with acute diarrhea and assessed for dehydration according to WHO guidelines. "Acute diarrhea" was defined as the passage of unusually loose or watery stools three or more times in a 24-hour period, with a maximum duration of 14 days. Dehydration was assessed based on signs such as restlessness or irritability, lethargy or reduced level of consciousness, sunken eyes, slow or very slow skin pinch return, thirstiness or eager drinking, or poor drinking ability. Patients with immunological abnormalities or chronic conditions were excluded.
Children with acute diarrhea who did not display enough symptoms to be classified as having moderate or severe dehydration were included in the control group. The age and gender of the children in the control group were matched to those of the cases.
The sample size was calculated using the following formula:
Where:
- n is the minimum sample size.
- α is the type I error rate; choosing (α = 0.1) gives (
- β is the type II error rate; choosing (β = 0.2) gives (
- p1 = 0.8125 is the proportion of children with vomiting in the acute diarrhea with dehydration group, based on a study by author L. Vorlasane conducted in 2023 (6).
- P2 = 0.529 is the proportion of children with vomiting in the acute diarrhea without dehydration group, based on a study by author L. Vorlasane conducted in 2023 (6)).
- With
- The case-to-control ratio is 1: 4.
Substituting these values into the formula, we obtain n = 33. Therefore, the sample size for the patient group is 33, and the sample size for the control group is 132. In actuality, 34 children participated as cases and 137 children as controls during data collection for the study. The study will involve invitations to participate extended to all children who meet the inclusion criteria for both the cases and controls and who have been admitted to the Gastroenterology Department at Can Tho Children's Hospital. To start, data on age and gender will be gathered to evaluate similarities. Subsequently, information on body temperature, frequency of vomiting and watery stools per day, and nutritional status will be collected and compared to determine risk factors. Ultimately, a scoring system with a suitable cut-off will be created based on these risk variables to estimate the possibility of dehydration in children suffering from acute diarrhea.
3.2. Statistical Analysis
Data were entered and analyzed using Statistical Package for Social Sciences (SPSS) software version 18.0 (International Business Machines Inc., Armonk, NY, USA). For qualitative data, frequencies and percentages were calculated; for quantitative variables, mean values and standard deviations were determined. The difference between two mean values was assessed using the Student's t-test, also known as the t-test. The comparison of two qualitative variables was performed using the Chi-square test. Logistic regression was employed to determine associations among the surveyed variables. Predictive criteria were established using receiver operating characteristic (ROC) curves and the area under the ROC curve (AUC). The predictive scoring system's sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), and positive likelihood ratio (LR+) were determined.
3.3. Ethical Approval
This study has been approved by the Ethics Committee in Biomedical Research of Can Tho University of Medicine and Pharmacy, Can Tho City, Vietnam under Decision No. 22.139.SV/PCT-HĐĐĐ dated November 30, 2022. The patients' families were fully informed about the study's aims and scope and were required to complete a consent form before the patients' participation. Every detail pertaining to research participants is kept totally confidential. The researchers processed and collected data in an unbiased and truthful manner.
4. Results
4.1. General Characteristics of the Study Subjects
This study included 34 children with acute diarrhea and dehydration and 137 children with acute diarrhea without dehydration who were admitted to the gastroenterology department of Can Tho Children's Hospital between November 2022 and October 2023. Table 1 shows that there were no statistically significant differences (P > 0.05) in the characteristics of the dehydration and non-dehydration groups, including average age, age group distribution, and gender.
| Characteristic | Cases Group (n = 34) | Controls Group (n = 137) | P-Value |
|---|---|---|---|
| Age, mo | 0.359 | ||
| Mean | 14.24 ± 6.95 | 16.29 ± 12.56 | |
| ≤ 24 | 30 (88.2) | 117 (85.4) | 0.789 |
| > 24 | 4 (11.8) | 20 (14.6) | |
| Sex | 0.244 | ||
| Male | 24 (70.6) | 81 (59.1) | |
| Female | 10 (29.4) | 56 (40.9) |
a Values are expressed as mean ± SD or No. (%).
4.2. Risk Factors for Dehydration in Children with Acute Diarrhea
In comparison to the controls, the patients experienced higher temperatures, more frequency of diarrhea per day, and more frequency of vomiting per day; this difference was statistically significant (P < 0.05) (Table 2). Acute diarrhea with dehydration was related to the following factors: Fever (OR 1.802, 95% CI 1.703 - 3.024, P = 0.026), frequency of diarrhea per day (OR 1.744, 95% CI 1.432-2.125, P < 0.001), frequency of vomiting per day (OR 1.242, 95% CI 1.102 - 1.399, P < 0.001), and weight-for-age > +2SD (OR 3.293, 95% CI 1.151 - 9.422, P = 0.026) (Table 3).
| Characteristics | Case Group (n = 34) | Control Group (n = 137) | P-Value |
|---|---|---|---|
| Weight for age | 0.233 | ||
| < -2SD | 1 (2.9) | 13 (11.2) | |
| -2SD - +2SD | 28 (82.4) | 114 (83.2) | |
| > +2SD | 5 (14.7) | 10 (7.3) | |
| Temperature | 38 ± 0.72 | 38.24 ± 0.72 | 0.023 |
| Frequency of diarrhea per day | 6.39 ± 3.15 | 10.15 ± 3.77 | < 0.001 |
| Frequency of vomiting per day | 2.99 ± 3.04 | 4.76 ± 3.53 | 0.001 |
a Values are expressed as mean ± SD or No. (%).
| Related Factors | Logistic Regression Model | ||
|---|---|---|---|
| OR | 95%CI | P-Value | |
| Temperature, °C | 1.802 | 1.703 - 3.024 | 0.026 |
| Frequency of diarrhea per day | 1.744 | 1.432 - 2.125 | < 0.001 |
| Frequency of vomiting per day | 1.242 | 1.102 - 1.399 | < 0.001 |
| Weight for age > +2SD | 3.293 | 1.151 - 9.422 | 0.026 |
4.3. Initial Steps in Developing a Scoring System to Predict Dehydration
As indicated in Table 4, a new scoring system, known as the KVAD (K: Kelvin, V: Vomit, A: Avoirdupois, D: Diarrhea) score, has been developed based on the findings of logistic regression analysis. Simultaneously, the initials K and V stand for the first names of the two authors who collaborated to create this scoring system. The KVAD score was developed to predict the likelihood of dehydration in children with acute diarrhea, evaluated based on the following criteria:
- The risk of dehydration increases by 1.802 times relative to the controls for every 1°C increase in temperature, and it was given a weight of 2 points.
- The risk of dehydration rises by 1.744 times with each episode of liquid stool compared to the controls, and it was given a weight of 2 points.
- The risk of dehydration rises by 1.242 times for every vomiting episode compared to the controls, and it is worth one point.
- Dehydration is 3.293 times more likely to occur in children admitted for acute diarrhea with weight-for-age > +2SD than in the controls; this risk is given a weight of 3 points.
| Criteria | Points |
|---|---|
| Increase in temperature for each 1OC | 2 |
| For each episode of diarrhea | 2 |
| For each episode of vomiting | 1 |
| Weight for age > +2SD | 3 |
Abbreviations: K, Kelvin; V, vomit; A, avoirdupois; D, diarrhea.
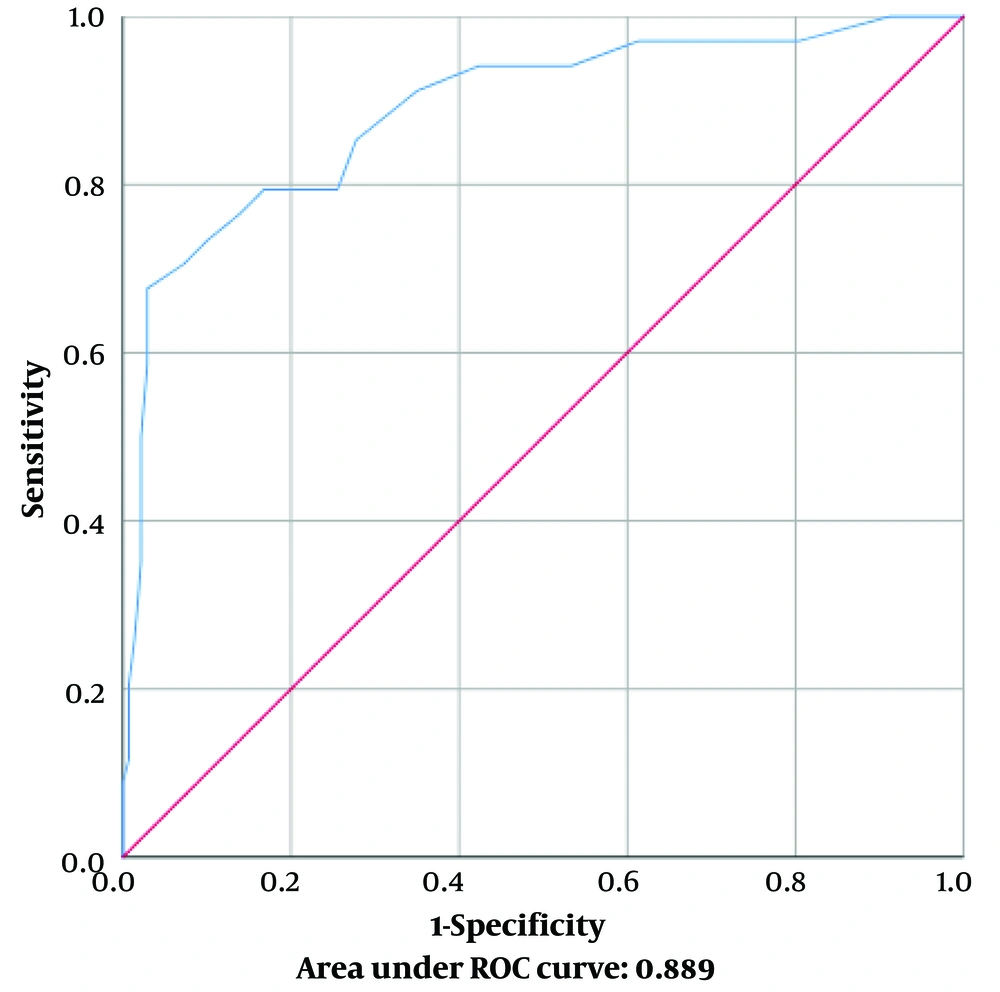
Then, the total score was calculated from the above variables. With an AUC of 0.889, the ROC curve, as shown in Figure 1, demonstrated the association between the sensitivity (true positive rate) and false positive rate of the KVAD score in identifying the severity of dehydration in children with acute diarrhea. As shown in Table 5, a score of 21 was the best cut-off point for determining if dehydration was present in children with acute diarrhea, with a sensitivity of 79.4% and specificity of 85.4%.
| Points | Sensitivity (Se) | Specificity (Sp) | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Positive Likelihood Ratio (LR+) |
|---|---|---|---|---|---|
| 18 | 0.852 | 0.737 | 0.446 | 0.952 | 3.245 |
| 19 | 0.794 | 0.751 | 0.442 | 0.936 | 3.199 |
| 20 | 0.794 | 0.737 | 0.428 | 0.935 | 3.022 |
| 21 | 0.794 | 0.854 | 0.574 | 0.943 | 5.439 |
| 22 | 0.764 | 0.883 | 0.619 | 0.937 | 6.547 |
| 23 | 0.735 | 0.912 | 0.675 | 0.932 | 8.394 |
| 24 | 0.676 | 0.927 | 0.696 | 0.92 | 9.267 |
5. Discussion
In this study, a similarity in the age distribution of pediatric patients with acute diarrhea was observed in both the disease and control groups. Most cases of acute diarrhea were predominantly concentrated in the age group under 24 months, with no significant difference between the two groups. Notably, the proportion of dehydrated cases in acute diarrhea was 88.2% and 85.4% for children with and without dehydration, respectively, indicating consistency in age distribution among children with acute diarrhea. These findings align with previous research by Zhu et al. in 2016, focused on Children under 5 Years of Age in Wuhan City, China, where the rate of children with diarrhea under 24 months old was reported as 86.9% (7). The study by the author Tor A. Strand et al. in Bhaktapur city near Kathmandu, Nepal highlights a similar trend, with an incidence rate of diarrhea in the group of children under 24 months old reported as 80.6% (8). Regarding the gender ratio in both groups of children with acute diarrhea, including both the case group and the control group, there is a tendency towards a higher male ratio. In the group of children with acute diarrhea and dehydration, the proportion of males was 70.6%, while in the group of children with acute diarrhea without dehydration, the proportion of males was 59.1%. Compared to previous studies by the author Muziburrahman et al. in Bolo and Wawo's Public Health Center Area, Bima District, Indonesia, in 2020, the proportion of males in cases of acute diarrhea accounts for 61.76% (9). In this study, the male-to-female ratio is 1.59/1. This result is also consistent with the study conducted by the author Mahmud et al., on 13 361 children under the age of 5 who were admitted to the hospital between January 2008 and December 2017 in Dhaka, Bangladesh, where the male-to-female ratio was reported as 1.59/1 (10). Boys are often more prone than girls to become sick, both more quickly and with greater severity. This is true not only for acute diarrhea but also for other infectious diseases (11, 12).
In terms of clinical characteristics, the majority of children with acute diarrhea have weight-for-age within the normal range, accounting for a high proportion of 83%. A notable observation in our study is that children with dehydrated acute diarrhea often exhibit a higher average body temperature compared to the non-dehydrated group, with an average of 38.24 ± 0.72°C. The frequency of diarrhea episodes and vomiting in the group of children with dehydrated acute diarrhea is also higher, at 10.15 ± 3.77 times and 4.76 ± 3.53 times, respectively. These results align with the findings of Zodpey's works performed on children under 5 years old in Nagpur, India. The author emphasizes the issue of dehydration in children with diarrhea, concluding an increase in the frequency of diarrhea episodes and vomiting compared to cases without dehydration (13).
In the logistic regression analysis to determine factors related to the degree of dehydration, this study demonstrates a correlation between the degree of dehydration and factors such as temperature, number of diarrhea episodes per day, number of vomiting episodes per day, and weight-for-age > +2SD. These results align with a previous study by Zodpey et al., which also noted an association between dehydration status and the frequency of vomiting and diarrhea episodes per day (13). After identifying factors related to the degree of dehydration, we developed a new predictive tool by constructing a scoring system called the KVAD score. In this scoring system, we assigned weights to relevant factors, including assigning 2 points for each degree increase in temperature above 37°C, 2 points for each diarrhea episode per day, 1 point for each vomiting episode per day, and 3 points for weight-for-age > +2SD.
The KVAD Score and the WHO dehydration assessment scale approach the evaluation of dehydration from different perspectives. While the WHO scale relies on general indicators like general appearance, eyes, thirst, and skin turgor, the KVAD Score delves into specific physiological parameters such as body temperature variations, vomiting frequency, weight for age > +2SD, and loose stool frequency. In comparing the two methods, the KVAD Score's emphasis on quantitative analysis sets it apart. By assigning numerical values to each parameter and establishing a threshold for dehydration based on the total score, the KVAD Score provides a standardized and objective assessment framework. This quantitative precision enables healthcare providers to gauge dehydration severity more accurately, leading to more targeted interventions.
Moreover, the KVAD Score offers a comprehensive evaluation by considering multiple facets of dehydration. By encompassing various parameters, including body temperature, vomiting frequency, weight for age > +2SD, and loose stool frequency, this multifaceted approach ensures that no aspect of dehydration goes unnoticed, allowing for a more thorough assessment. The standardized scoring system of the KVAD Score further enhances its utility. By promoting consistency in assessment practices across different healthcare settings, it facilitates comparability of results and ensures uniformity in patient care. This standardization streamlines the assessment process, making it easier for healthcare providers to interpret results and make informed decisions regarding patient management.
Overall, the KVAD Score offers several advantages over the WHO dehydration assessment scale, including quantitative precision, comprehensive evaluation, and standardization. These features contribute to its effectiveness as a dehydration assessment tool and highlight its potential to improve patient care outcomes. Subsequently, we calculated the total score and conducted ROC curve analysis, calculating the AUC to assess the predictive ability of this model for the degree of dehydration. Next, we determined the cutoff point to achieve the highest sensitivity and specificity in predicting the dehydration status.
The KVAD scoring system demonstrates an AUC of 0.889 in the ROC curve analysis, indicating its effectiveness as a screening model applicable in clinical settings. The optimal cutoff point for predicting dehydration likelihood is determined to be 21 points, with a sensitivity of 79.4% and specificity of 85.4%. In comparison to a study by author Modi et al., conducted on 771 children under 5 years old at the rehydration unit of the International Center for Diarrhoeal Disease Research, Bangladesh in 2014, which utilized the inferior vena cava ultrasound method to predict dehydration in children, the KVAD score in this study not only exhibits higher sensitivity (79.4% vs. 67%) but also higher specificity (85.4% vs. 49%). Furthermore, the AUC of the KVAD score's ROC curve is 0.889, surpassing the AUC of the inferior vena cava ultrasound method ROC curve (0.6) (14).
When compared to the Gorelick score, performed on 220 children under 15 years old in Bangkok, Thailand by author Kanjanaphan et al in 2017, which has a sensitivity of 45.5%, specificity of 58%, and AUC of 0.52 (15), and the CDS score, with a sensitivity of 68% and specificity of 45% for moderate dehydration, conducted by Kimberly Pringle et al on children under 15 years old hospitalized in the pediatric department of three district hospitals, Kirehe, Rwinkwavu, and Butaro, in Rwanda (16), it becomes evident that the KVAD score in this study exhibits higher accuracy in predicting the likelihood of dehydration in children with acute diarrhea.
Overall, our KVAD scoring system can be applied in clinical practice to forecast the likelihood of dehydration, especially in primary healthcare settings, enabling the early detection of dehydration and timely implementation of fluid replacement interventions.
One of the limitations of this study is the relatively small sample size of the dehydration group. However, this was simply the first step in our research endeavor. We will continue to conduct further studies involving larger and more diverse groups of individuals across various locations to enhance the accuracy and applicability of the KVAD score. This incremental approach to research will allow us to refine the KVAD score, enabling healthcare providers to utilize it more effectively. Although our initial study had its constraints, it lays the groundwork for the development of a reliable dehydration assessment tool in the future.
In conclusion, the KVAD score represents the initial phase in the development of an effective and reliable screening tool to estimate the risk of dehydration in children with acute diarrhea.