1. Introduction
Diabetes mellitus (DM) represents a series of chronic metabolic conditions, biochemically characterized by hyperglycemia resulting from insulin deficiency due to pancreatic β-cell damage (type 1 DM) or peripheral tissue insulin resistance (type 2 DM) (1). Additionally, several other specific types of DM have been classified under a broad category termed maturity-onset diabetes of the young (MODY) (2). Type 2 diabetes mellitus (T2DM), also called non-insulin-dependent DM, is associated with insulin resistance and progressive non-autoimmune β-cell dysfunction (3). While T2DM has long been the most prevalent form of DM among young adults (formerly called adult-onset diabetes mellitus), an increasing trend of T2DM and prediabetic dysglycemia has been noticeably observed among children and adolescents in recent years. Whether it is DM or prediabetes, exposure to chronic hyperglycemia increases the risk of microvascular and long-term macrovascular complications. It is noteworthy that reductions in mortality among people with DM, associated with current antidiabetic medications, will increase the lifetime accumulation of T2DM complications and morbidities worldwide (4). All these issues, plus the fact that the atherosclerotic process may originate in childhood and adolescence, highlight the necessity of obesity and DM screening among children (5-7) (Table 1). Given the importance of DM and obesity, this narrative review aimed to address the optimal screening and control of childhood obesity as the main strategies for dealing with the comorbidities of T2DM.
| Condition | Description |
|---|---|
| Diabetes mellitus (DM) | A series of chronic conditions characterized by hyperglycemia as a result of insulin deficiency from pancreatic β-cell damage (T1DM) or peripheral tissue insulin resistance (T2DM). |
| T2DM | It is the non-insulin-dependent DM which relates to insulin resistance and progressive non-autoimmune β-cell dysfunction. It has been increasingly observed among children and adolescents. |
| Maturity-onset diabetes of the young (MODY) | A category that encompasses several specific types of diabetes, classified under MODY. |
| Complications of chronic hyperglycemia | Exposure to chronic hyperglycemia rises the risk of microvascular such as retinopathy, neuropathy, and nephropathy as well as long-term macrovascular complications, including ischemic heart disease, peripheral vascular disease, and cerebrovascular diseases. |
| Mortality reduction and T2DM complications | Reductions in mortality associated with current antidiabetic medications can increase the lifetime accumulation of T2DM complications and morbidities worldwide. |
| Necessity of obesity and diabetes screening | The atherosclerotic process may originate in childhood and adolescence, highlighting the importance of screening for obesity and diabetes among children. |
| Strategies for dealing with T2DM comorbidities | Optimal screening and control of childhood obesity are emphasized as the main strategies for dealing with comorbidities of T2DM. |
The Overview of Diabetes Mellitus and Associated Complications
2. Methods
To conduct this narrative review, we performed a thorough search across multiple reliable databases, including PubMed, Web of Science, and Scopus, utilizing relevant keywords such as obesity, DM, patients, and treatment. This approach aimed to gather a comprehensive understanding of the connection between obesity and T2DM in patients. The search encompassed articles from the inception of each database to ensure a comprehensive understanding.
3. Results
In many patients, T2DM may take years to become symptomatic. Many individuals with this disorder, as well as those with poorly controlled prediabetes and DM, experience few symptoms for a large portion of their lives (8). Accordingly, it is undeniable that screening for prediabetes and childhood obesity (as a major risk factor) is a significant intervention opportunity to prevent the future development of DM and its lifelong health consequences (9).
3.1. The Definition of Prediabetes and Diabetes
Prediabetes is a condition characterized by mild elevations in plasma glucose levels that are not high enough to warrant a diagnosis of T2DM. This period of progressive abnormal glucose homeostasis is currently diagnosed by the following three criteria (10):
- Glycated hemoglobin A1c (HbA1c) 5.7%-6.4% (39 - 47 mmol/mol); or
- Fasting plasma glucose (FPG) 100 to 125 mg/dL (5.6-6.9 mmol/L), which is more specifically labeled as impaired fasting glucose (IFG); or
- 2-hour postprandial plasma glucose level of 140 to 199 mg/dL (7.8-11 mmol/L) following a 75-gram oral glucose tolerance test (OGTT), which is termed impaired glucose tolerance (IGT).
Individuals meeting any of these three diagnostic criteria are at high risk of an inevitable progression to T2DM and should be counseled about ways to decrease their risk of morbidity and mortality later in life (10).
3.2. The Major Lifestyle-Related Risk Factor
Early diagnosis of prediabetes or type 2 diabetes mellitus (T2DM) in children and adolescents is vital due to distinct characteristics such as hastened insulin secretion deterioration and the swift advancement of comorbidities compared to adults. Therefore, risk-based screening is essential for detecting asymptomatic young individuals for timely and appropriate management (11). Most modifiable risk factors for T2DM are environmental and lifestyle-related. The significant lifestyle-related factor contributing to the emergence of T2DM is the global surge in overweight and obesity among children in recent decades. Indeed, obesity is a prevalent condition and a recognized risk factor for various medical ailments (5).
The definition of obesity is based on body mass index (BMI), which is calculated by dividing weight in kilograms (kg) by height in meters squared (m²) for both children and adults. However, the precise definitions are not directly equivalent. Among adults, the World Health Organization defines a BMI in the range of 25-30 kg/m² as overweight and a BMI ≥30 kg/m² as obesity. Nevertheless, the definition of obesity among children is more statistical because BMI varies considerably with age in childhood. Therefore, the BMI of a child is generally compared with the BMI of a reference pediatric population of the same sex and age (5).
The evaluation of an overweight or obese child should include obtaining a comprehensive medical history and examining the trends of growth charts based on the child’s weight, height, and BMI trajectories to reveal the severity, duration, and timing of obesity onset. Obesity and overweight are defined using weight-for-length percentiles for infants younger than 2 years and BMI percentiles for children older than 2 years. The criterion for overweight is a BMI in the 85th-95th percentile, and for obesity, it is a BMI ≥95th percentile. Furthermore, physical examination frequently may reveal the presence of other supporting findings resulting from insulin resistance and metabolic syndrome, such as an increased waist-to-hip and waist-to-height ratio, striae distensae, acanthosis nigricans, and skin tags (10, 12, 13).
According to the United Kingdom Clinical Practice Research Datalink (CPRD), obese children and young adults are projected to have a fourfold higher risk of developing T2DM compared to individuals with a normal BMI (14). This risk can increase even more in adulthood. It is estimated that obese people, in general, have approximately a sevenfold greater risk of DM compared to those of healthy weight (15).
3.3. Global Trends of Childhood Obesity
The occurrence of childhood obesity varies depending on factors such as country of residence, age, and ethnicity. Considering that some studies controversially show the absence of a significant increase in childhood obesity (16), we reviewed some of the most recent and comprehensive statistical studies from different countries. The National Health and Nutrition Examination Survey (NHANES), spanning from 1999 to 2018, observed a concerning upward trend in childhood obesity rates among 35,907 children aged 2-19 in the United States. During this period, the average BMI rose from 19.87 kg/m² to 20.71 kg/m². Moreover, the prevalence of overweight, obesity, and severe obesity (BMI ≥ 120% of the 95th percentile) increased from 14.1% to 16.1%, 14.7% to 19.2%, and 3.9% to 6.1%, respectively (17).
The prevalence of obesity among children and adolescents in Iran has notably increased. Between 2000 and 2016, the obesity rates for boys and girls aged 5 - 9 rose from 6% and 4.9% to 13.1% and 9.8%, respectively. Similarly, for those aged 10-19, the obesity rates increased from 3.9% for both boys and girls in 2000 to 9.3% and 8.1% in 2016, respectively (18). A systematic review covering articles from 1977 to 2017 examined obesity prevalence among Iranian students aged 6 - 20. Across 160 studies involving 481,070 individuals, the prevalence of overweight and obesity based on BMI was found to be 12% (13% in girls, 11% in boys) and 11% (8% in girls, 11% in boys), respectively (19).
In China, consistent rises in mean BMI across all age groups have been documented. Based on data from the China National Nutrition Surveys (CNNSs) spanning from 1992 to 2019, the prevalence of overweight and obesity among children aged 6-17 increased from 3.9% to 11.1% and 1.8% to 7.9%, respectively (20). A comprehensive study conducted by the Childhood Obesity Surveillance Initiative (COSI) across European countries from 2007 to 2017 showed varying trends in overweight and obesity prevalence. Southern European countries such as Greece, Italy, Portugal, Slovenia, and Spain displayed predominantly decreasing trends among boys and girls. In contrast, Northern and Eastern European countries showed more stable patterns in obesity prevalence. Compared to many countries globally, several European nations appear to have effectively implemented policies and interventions to combat the rise in overweight and obesity (21).
3.4. Challenges in Childhood Obesity and Diabetes Management
To address obesity, interventions targeting caloric intake and energy expenditure imbalances are crucial. Recommending appropriate caloric intake based on non-obesogenic foods like fruits, vegetables, whole grains, nuts, legumes, lean meats, fish, and poultry, while limiting unhealthy obesogenic foods such as sugary drinks and processed snacks, is essential. Additionally, reducing sugar-sweetened beverage consumption, increasing physical activity, and minimizing screen time (time spent on TV, video games, and mobile phones) are effective strategies for sustainable weight loss and improving BMI (5, 22).
Recommended policy and regulatory approaches to prevent childhood obesity include taxation on sugar-sweetened beverages and energy-dense foods, informing consumers through nutrition labeling, school-based initiatives to influence diet and physical activity behaviors, and media and marketing efforts to improve public awareness of a healthy lifestyle (11, 23). However, the entertainment industry can also reinforce negative stereotypes of obese people through negative portrayals and underrepresentation. This aspect of the media is important because obesity stigma and poor mental health outcomes increase the risk of obesity (24).
The prevalence of obesity differs across various societal groups, as highlighted in a narrative review by Iguacel et al. The study explores the association between social vulnerabilities and childhood obesity, identifying low socioeconomic status, parental unemployment, belonging to minority or migrant groups, and adverse childhood experiences (such as parental separation, exposure to violence, sexual abuse, maternal smoking, and unsafe living environments) as risk factors for childhood overweight and obesity (25). Contrary to previous findings, a study conducted across urban and rural areas of 30 provinces in Iran revealed that obesity prevalence is higher among individuals with high socioeconomic status (26). Whether obesity is caused by good or bad socioeconomic conditions, it is clear that obesity poses substantial health and economic burdens on society (27).
Screening is vital for managing obesity and DM. Prediabetes, often asymptomatic, requires risk-based screening for early detection and timely intervention in children with dysglycemia to prevent or delay comorbidities and chronic complications in adulthood. While the incidence of T2DM in children, often associated with obesity, is increasing, the United States Preventive Services Task Force (USPSTF) statement indicates insufficient evidence to evaluate the benefits and risks of screening for T2DM in asymptomatic children and adolescents (28, 29). In our view, this recommendation could have been different if risk factors, comorbidities, and chronic adulthood complications of T2DM were considered more widely. Thus, targeting children with obesity and other mentioned risk factors obligates healthcare providers to offer appropriate advice regarding dietary and lifestyle interventions for their parents (5).
Apart from risk-based screening, it appears that risk-based treatment of DM is expanding nowadays. Recently, beyond the drugs used for glycemic control and weight loss (such as metformin, liraglutide, thiazolidinediones, sulfonylureas, sodium-glucose cotransporter 2 inhibitors, ozempic and mounjaro, and insulin) for T2DM patients, the initial trial findings of a promising study by Billon et al. have shown amazing results on metabolism-boosting and increasing muscle gain among mice without any exercise by a newly developed compound called SLU-PP-332 (30, 31).
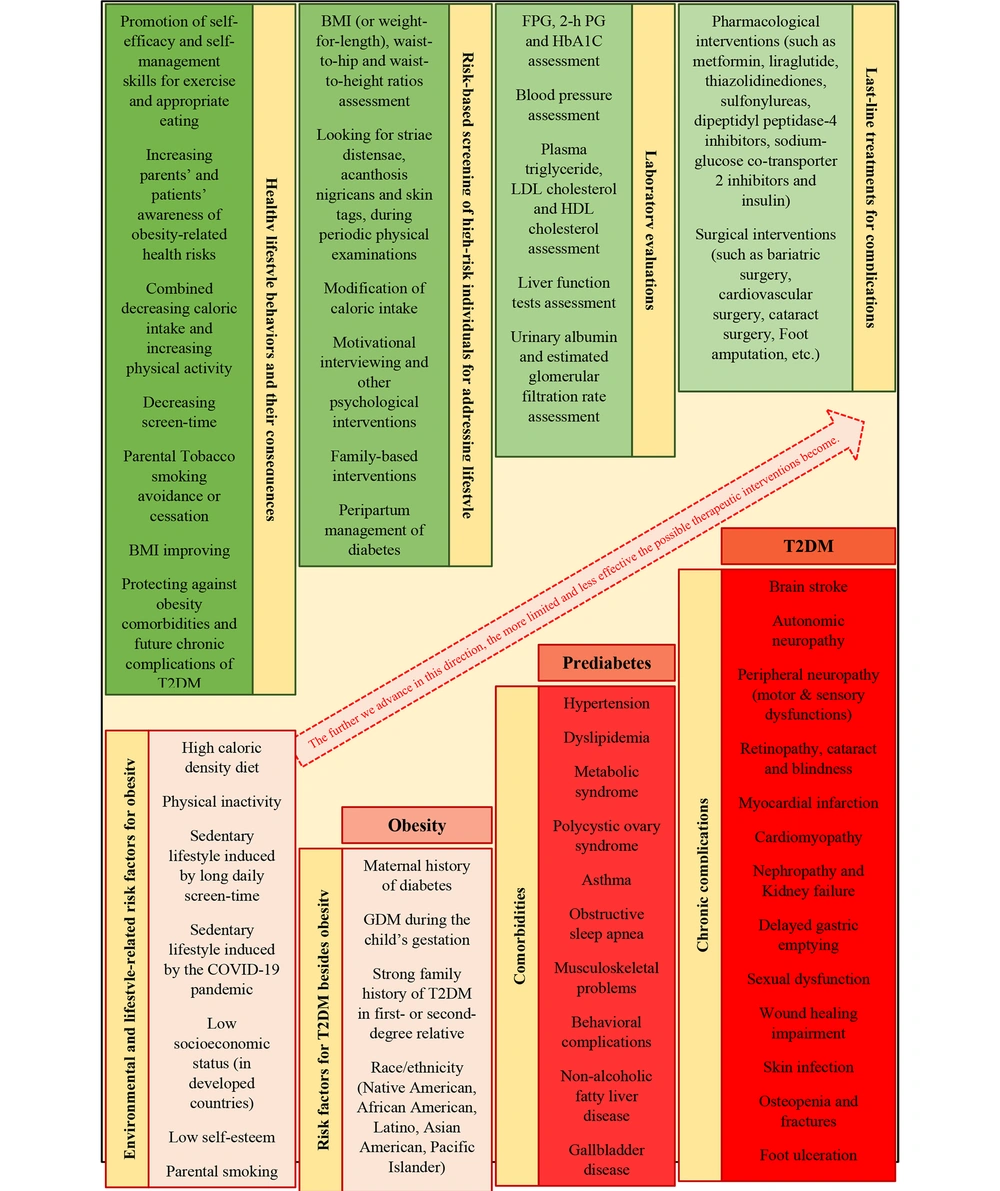
The realistic and comprehensive pathway from unhealthy lifestyle behaviors, obesity, and prediabetes, to life-disrupting DM-related complications is undoubtedly complex. However, we aim to provide an overview of this pathway and available effective therapeutic interventions at every stage in Figure 1 (10, 25).
4. Conclusions
According to this narrative review, we suggest that in the case of DM and obesity, the focus should be on the links between T2DM and its modifiable risk factors. Children’s lifestyle modification, whether through risk-based screening or risk-based treatment, is an impactful change that can be maintained for life and increase their life expectancy. It is noteworthy that reductions in mortality among people with DM, associated with current antidiabetic medications, will increase the lifetime accumulation of T2DM complications and morbidities worldwide. We believe that future studies are needed to examine the effects of systematic risk-based screening on these important issues in the modern world.