1. Introduction
Johnson-Blizzard syndrome is an extremely rare autosomal recessive disorder that affects multiple organ systems. This condition affects both genders equally, and its precise prevalence is unknown, but it is estimated to occur in approximately 1 in 250,000 live births. The UBR1 gene located on chromosome 15q15.2 is currently recognized as the causative gene in this syndrome (1). This syndrome has a wide spectrum of clinical features, including nasal alae hypoplasia, scalp defects, sensorineural hearing loss, hypothyroidism, mental and growth retardation, exocrine pancreatic insufficiency, imperforate anus, dental problems, cardiac anomalies, urogenital abnormalities, microcephaly, abnormal hair patterns, and short stature (2). The most prominent feature of this syndrome is exocrine pancreatic insufficiency, which presents in nearly 81.8% of all Johnson-Blizzard syndrome (JBS) cases upon literature review (2). Pancreatic failure and hypothyroidism can be the main risk factors for mental and growth retardation in these patients (3).
2. Case Presentation
We present the case of a 5-year-old male patient who was referred to the pediatric gastroenterology clinic for management of fecal incontinence and growth delay. Informed and written consent for the publication of patient information has been obtained from the patient's parents.
2.1. Past Medical History
The patient had a history of imperforate anus, which required surgical correction at birth. He was the first child born to non-consanguineous parents.
2.2. Physical Examination
On initial evaluation, the patient's height was 87 cm and weight was 8 kg, both below the 3rd percentile for age (Z-score: < -3). His head circumference was 45 cm. Physical examination findings included hypoplasia of the alae nasi (beak-shaped nose), microcephaly, an abnormal frontal hairline pattern, and dental anomalies (Figure 1). Behavioral assessment revealed intellectual disability.
2.3. Para Clinical Evaluation
Twice, sweat tests were normal, but the elastase activity and trypsin activity tests in the stool were abnormal. The patient's pancreatic insufficiency was confirmed through these abnormal stool elastase and trypsin activity tests. Total protein, albumin, and other liver function tests, renal function tests, serum electrolytes, thyroid function tests, and blood sugar were within the normal range. Echocardiography, abdominal ultrasound, and chest X-ray (CXR) were normal. Anorectal manometry was performed and found to be normal.
2.4. Auditory System Evaluation
The following diagnostic tests were performed: Otoscopy examination, tympanometry, acoustic reflex, auditory brainstem response (ABR), and distortion product otoacoustic emissions (DPOAE).
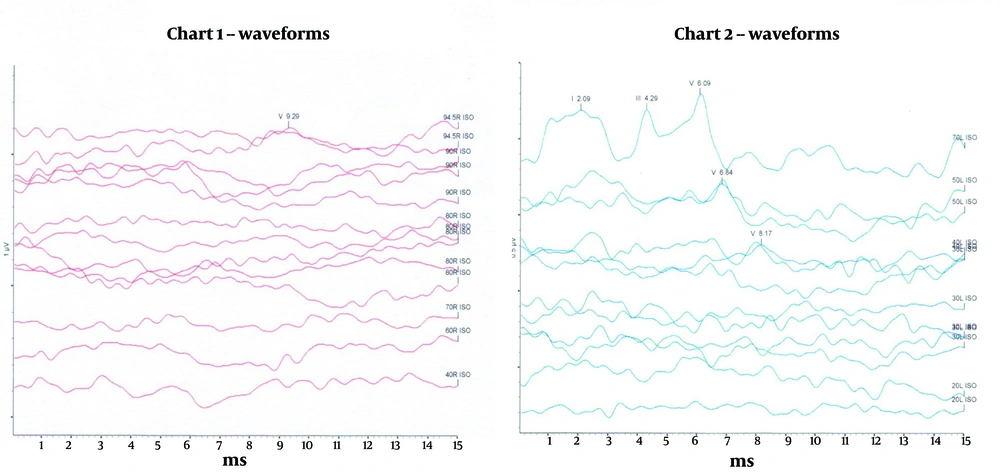
2.5. Auditory Brainstem Response
BR is a non-invasive electrophysiological test that evaluates the integrity of auditory pathways from the cochlea to the brainstem. It involves placing electrodes on the scalp and earlobes to record the brain's response to auditory stimuli, such as clicks or tone bursts. The results, displayed as waveforms, provide insights into the auditory nerve and brainstem's ability to transmit sound signals effectively. This test is particularly useful for determining the degree and type of hearing loss, identifying the location of damage, and assessing auditory nerve and brainstem functionality. The ABR is widely used for hearing screening in infants and children and for diagnosing neurological conditions like acoustic neuroma. Its non-invasive nature and independence from patient cooperation make it suitable for all age groups, especially for individuals unable to respond actively during the test (4).
The ABR consists of five primary waves, each originating from specific neurogenic sites within the auditory pathway. Wave I comes from the distal part of the auditory nerve, wave II from the proximal part, wave III from the cochlear nucleus, wave IV from the superior olivary complex, and wave V from the inferior colliculus and lateral lemniscus fibers. The amplitude of these electrical impulses is small compared to the brain's background activity, requiring amplification and averaging to accurately capture neural events in response to sound stimuli. The results reveal the delay in milliseconds and the amplitude in microvolts of each wave peak. The ABR test helps determine hearing thresholds and assess the health of auditory pathways beyond the cochlea. Notably, as stimulus intensity decreases, most ABR waves disappear, except for wave V, which remains stimulated at intensity levels of 5 to 20 dB relative to behavioral hearing thresholds, indicating normal hearing when tracked up to 20 dB (5).
2.6. Distortion Product Otoacoustic Emissions
The DPOAE assesses cochlear health by evaluating the function of outer hair cells. It is a quick and non-invasive test that involves delivering two distinct tones into the ear canal. The cochlea’s outer hair cells generate a response called otoacoustic emission if they are functioning properly. This emission is recorded by a microphone placed in the ear canal. The DPOAE is instrumental in detecting early-stage cochlear damage caused by noise exposure, ototoxic drugs, or congenital factors. It is particularly useful in newborn hearing screening programs and in differentiating sensorineural from conductive hearing loss (4).
2.7. Flow Diagram: Diagnosis and Management of Johnson-Blizzard Syndrome
2.7.1. Introduction to the Disease
- Rare autosomal recessive disorder
- Symptoms: Exocrine pancreatic insufficiency, hypothyroidism, structural defects, sensorineural hearing loss, imperforated anus
2.7.2. Patient Introduction
5-year-old child presenting with:
- Growth retardation
- Exocrine pancreatic insufficiency
- History of imperforate anus
2.7.3. Physical Examination
- Height and weight below the 3rd percentile
- Physical findings: Hypoplasia, microcephaly
2.7.4. Para Clinical Evaluation
- Normal sweat tests
- Abnormal elastase and trypsin activity tests
- Anemia
2.7.5. Auditory System Evaluation
2.7.5.1. Diagnostic Tests Performed
- Auditory brainstem response
- Distortion product otoacoustic emissions
2.7.5.2. Auditory Brainstem Response Test Results
- Profound sensorineural hearing loss in the right ear
- Mild sensorineural hearing loss in the left ear
2.7.6. Treatment
- Pancreatic enzyme replacement therapy
- Biofeedback therapy for fecal incontinence
- Bilateral hearing aid
2.7.7. Follow-up and Outcomes
- Weight increase one month after treatment
- Significant improvement of hearing status
- Resolution of anemia
3. Discussion
Johnson-Blizzard syndrome is an extremely rare autosomal recessive disorder that affects multiple organ systems. The clinical features of JBS are wide-ranging, including nasal alae hypoplasia, scalp defects, sensorineural hearing loss, hypothyroidism, mental and growth retardation, exocrine pancreatic insufficiency, imperforate anus, dental problems, cardiac anomalies, urogenital abnormalities, microcephaly, abnormal hair patterns, and short stature (2). Sensorineural hearing loss (SNHL) is one of the clinical features of JBS. The prevalence of SNHL is equal in both genders, and most cases in JBS have been reported to be bilateral (6, 7), making the unilateral hearing loss in this case particularly rare. The patient presented with profound sensorineural hearing loss in the right ear and mild sensorineural hearing loss in the left ear, a rare presentation not commonly documented in the literature. This case provides an important contribution to the understanding of the auditory manifestations in JBS, suggesting that unilateral hearing loss may still be a part of the syndrome’s wide spectrum (8).
Reviewing existing literature, bilateral sensorineural hearing loss is the most prevalent auditory finding in JBS patients (1, 9, 10). The ABR results and DPOAE supported cochlear dysfunction in the right ear, consistent with sensorineural loss, while the left ear showed milder impairment. Tympanometry and acoustic reflex findings ruled out middle ear pathology. In this case, the combined use of ABR and DPOAE provided valuable insights into the patient's hearing impairment. The ABR offers information about the integrity of neural and brainstem pathways, while DPOAE assesses cochlear functionality. Together, they enable a thorough evaluation of the auditory system, guiding clinical interventions. The findings emphasize the need for detailed audiological assessments in patients with rare conditions like Johnson-Blizzard syndrome, as identifying specific hearing impairment characteristics can enhance early intervention and management, ultimately improving the patient's quality of life.
The management of JBS is multidisciplinary, involving specialists from gastroenterology, endocrinology, audiology, and developmental pediatrics. This patient’s growth retardation, intellectual disability, and exocrine pancreatic insufficiency are consistent with the typical phenotypic presentation of JBS. Pancreatic enzyme replacement therapy helped improve the patient’s nutritional status, though the patient’s growth parameters remained below the 3rd percentile. Biofeedback therapy for fecal incontinence also yielded noticeable improvement after one month of practice.
In this case report, potential biases and limitations include the reliance on clinical evaluation without genetic confirmation due to parental non-consent, which may limit the definitive diagnosis of Johnson-Blizzard syndrome. Additionally, the findings are based on a single case, making it challenging to generalize results to the broader population of JBS patients. The absence of long-term follow-up data on auditory outcomes and the lack of a control group for comparison further limit the conclusions that can be drawn about the prevalence and nature of unilateral hearing loss in this syndrome.
In conclusion, this case emphasizes the necessity of detailed audiological assessments in children with JBS, even in the absence of obvious hearing complaints, as early intervention is critical for their developmental outcomes. While bilateral SNHL remains the predominant form of hearing impairment in JBS, this report suggests that unilateral cases may occur, broadening the clinical spectrum of this complex disorder.
3.1. Key Findings
3.1.1. Auditory Brainstem Response Test Results
The ABR test revealed profound sensorineural hearing loss in the right ear and mild sensorineural hearing loss in the left ear (Figure 2). Bilateral symmetric hearing loss is more prevalent in children with JBS and correlates strongly with the presence of the syndrome, but unilateral hearing loss is very rare.
3.1.2. Associated Anomalies
Microcephaly, hypoplasia of the alae nasi, absence of permanent teeth, and scalp abnormalities.
3.1.3. Tympanometry and Acoustic Reflex
These tests assessed middle ear function, supporting the findings of normal middle ear function. It appears that JBS does not affect middle ear status.
3.1.4. Distortion Product Otoacoustic Emissions Results
The DPOAE was absent in the right ear and present in the left ear, supporting the finding of abnormal cochlear function in the right ear and normal cochlear function in the left ear.
3.2. Diagnose, Treatment and outcomes
Based on clinical evidence, a likely diagnosis was Johnson-Blizzard syndrome. However, a definitive diagnosis required genetic testing, which we requested for the patient. Unfortunately, the patient's parents did not consent to the genetic test. Therefore, the diagnosis of this syndrome was made solely based on clinical evidence and other evaluations. With a diagnosis of pancreatic insufficiency, the patient received pancreatic enzyme replacement therapy (Creon 25000) and multivitamins. We initiated biofeedback therapy to treat the patient's fecal incontinence. In the follow-up one month after the start of treatment, the patient's weight had increased, but it was still below the third percentile. The anemia had been corrected. The patient was prescribed bilateral hearing aids, which significantly improved his auditory status.