1. Background
After heart murmurs, chest pain is the second most common reason for visiting cardiologists and emergency departments. However, chest pain in children is more often associated with non-cardiac disorders, such as musculoskeletal issues involving the cartilage and ribs, trauma, muscle strain, or respiratory causes like bronchitis and pulmonary infections (1). The prevalence of chest pain is reported to be approximately 10% among school-aged children (2). Cardiac-related chest pain in children is generally rare and potentially dangerous (3). In children, chest pain can typically be categorized as either cardiac or non-cardiac. Non-cardiac chest pain is often described as recurrent, substernal chest pain that is not believed to be related to the heart (4). Additionally, chest pain in children and adolescents is frequently related to anxiety and depression caused by recent stressors in personal or family life.
Anxiety is an unpleasant and vague feeling, often accompanied by symptoms from the nervous system. It serves as a warning sign and creates responses in humans similar to fear, though fear is a response to a specific, external threat. If anxiety becomes intense and prolonged, it can be detrimental, playing a significant role in the development of psychosomatic diseases, such as coronary heart disease, hypertension, angina, and other psychosomatic disorders (5). Anxiety is not specific to any time or culture; it is an experience that begins at birth and continues throughout life, arising in response to new experiences such as starting school, employment, or other novel situations (6). Anxiety disorders are also among the most common mental health conditions in children, with prevalence rates between 14% and 19%. Children with anxiety disorders face a higher risk of substance use, suicide, and psychiatric disorders during adolescence and adulthood (7).
Furthermore, chest pain stemming from anxiety in children and adolescents can be related to rapid breathing, which leads to changes in blood gases (respiratory alkalosis) and causes coronary vessel constriction, resulting in pain. Examining the psychological and emotional causes of chest pain in children is essential. A psychological cause should be considered when other physical causes of chest pain have been thoroughly ruled out. In adolescents, these pains are more common in females and are often associated with recent emotional stress or the recent diagnosis of a physical illness. Chest pain with psychological origins is also more common in families with a history of heart disease or where a family member recently passed away due to a heart condition. Once physical causes are ruled out, reassuring the parents and child that no serious illness exists can significantly reduce their pain and anxiety (8).
In various studies, anxiety and depression have been identified as the most common mental disorders among these patients. In one study, 36% of individuals who reported heart problems and complained of chest pain were found to have no cardiac issues but were suffering from depression, while 30% had psychological issues linked to somatic complaints (5). The study by Derakhshanpour et al. indicated a prevalence of anxiety disorders in 14.14% of children and adolescents, significantly affecting their functionality and efficiency (9). Assessing children’s problems is a complex process that often encompasses multiple aspects of the child’s functioning, with the best evaluations carried out by a team of therapists using appropriate and diverse methods (10).
2. Objectives
Since anxiety is prevalent in many children and often presents as chest pain, and as no study on this topic has yet been conducted on children in Iran, we were motivated to conduct this study. Our goal is to compare anxiety levels in children with non-cardiac chest pain with a control group visiting the specialized cardiology clinics in Mashhad. We hope that the findings from this study will assist in identifying anxiety-related issues in children and aid healthcare providers, pediatricians, and families in recognizing these symptoms and managing them effectively.
3. Methods
This case-control analytical study was conducted on 62 children with non-cardiac chest pain who visited specialized cardiology clinics in Mashhad from April to July 2024. The patients were compared with 62 controls. The sample size for this study was determined based on Uzunoglu et al.’s study (11) using the formula for means, resulting in 62 participants per group. Sampling was conducted through convenience sampling. Inclusion criteria included experiencing chest pain within the past month, being between 8 and 15 years old, the child and parents having literacy skills, and holding Iranian nationality. Participants with a known mental disorder, intellectual disability, or a known systemic disease were excluded. After explaining the research objectives to the children and their parents and assuring them of their freedom to participate or withdraw at any time, informed written consent was obtained from all participants by the researcher.
The data collection tool in this study was a questionnaire consisting of two sections: (1) Demographic information, including age, gender, and parental living arrangements; (2) the Spence Children’s Anxiety Scale (SCAS), which has separate versions for the child (45 items) and the parent (38 items). Scoring is based on a 4-point Likert scale ranging from never (0) to always (3), assessing six subscales: Separation anxiety, social phobia, obsessive-compulsive, panic/agoraphobia, generalized anxiety, and fear of physical injury. The minimum score is 0, and the maximum is 114, with higher scores indicating greater anxiety. A cut-off score of 35 and above is used for diagnosing anxiety. The SCAS Scale’s reliability for general anxiety has been reported as 0.92, and for subscales, it ranges from 0.60 to 0.82 (12). In Iran, Mousavi et al. reported reliability for the SCAS, with Cronbach’s alpha coefficients ranging from 0.62 to 0.89, and confirmatory factor analysis validated the six factors of the questionnaire (13). In this study, Cronbach’s alpha was calculated at 0.89.
Control group participants were selected from children visiting the pediatric cardiology clinic for sports participation clearance, innocent heart murmurs, or routine check-ups. Before enrollment, all children underwent a comprehensive cardiac evaluation by a pediatric cardiology specialist, including medical history, physical examination, electrocardiography, and echocardiography. The SCAS was completed by both the child and parent in a separate room at the clinic for both the chest pain and control groups.
Data analysis was performed using SPSS software version 22. For quantitative data, mean and standard deviation were reported, while for qualitative data, frequency and percentage were presented in tables. Inferential statistics included the chi-square test for qualitative variables and, for normally distributed continuous variables, the independent t-test, and the Mann-Whitney test for non-normally distributed data. A significance level of P < 0.05 was set for all analyses.
4. Results
The study compared mean total anxiety scores and subscale scores between children with non-cardiac chest pain and a control group, as shown in Table 1. Findings indicated that the case group had significantly higher mean total anxiety scores, averaging 45.81 compared to 23.44 in the control group (P < 0.001). This significant difference suggests a substantial psychological impact of non-cardiac chest pain on children. Additionally, the subscale scores revealed notable disparities, with the case group scoring higher on various anxiety dimensions, including social phobia (6.94 vs. 3.71), separation anxiety (8.69 vs. 4.42), and generalized anxiety (8.44 vs. 4.53).
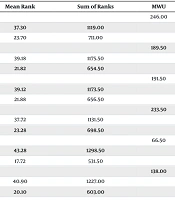
Table 2 focused on boys with non-cardiac chest pain in comparison to a control group. Boys in the case group had a total anxiety score of 45.93, compared to 22.33 for the control group, with significant differences observed across all subscales (P < 0.001). The subscale scores highlighted disparities, especially in social phobia (6.53 vs. 3.60), separation anxiety (8.80 vs. 4.43), and generalized anxiety (8.63 vs. 4.17).
| Anxiety and Its Subscales | Mean ± SD | Mean Rank | Sum of Ranks | MWU | P-Value a |
|---|---|---|---|---|---|
| Panic/agoraphobia | 971.5 | < 0.001 | |||
| Case | 6.94 ± 4.12 | 77.83 | 4825.5 | ||
| Control | 3.71 ± 3.21 | 47.17 | 2924.5 | ||
| Separation anxiety | 759.5 | < 0.001 | |||
| Case | 8.69 ± 4.21 | 81.25 | 5037.5 | ||
| Control | 4.42 ± 3.07 | 43.75 | 2712.5 | ||
| Physical injury fears | 1041 | < 0.001 | |||
| Case | 6.56 ± 3.61 | 76.71 | 4756 | ||
| Control | 3.85 ± 2.94 | 48.29 | 2994 | ||
| Social phobia | 1061 | < 0.001 | |||
| Case | 6.66 ± 3.72 | 76.39 | 4736 | ||
| Control | 3.84 ± 2.50 | 48.61 | 3014 | ||
| Obsessive compulsive | 529.5 | < 0.001 | |||
| Case | 8.52 ± 4.26 | 84.96 | 5267.5 | ||
| Control | 3.08 ± 2.89 | 40.04 | 2482.5 | ||
| Generalized anxiety | 693 | < 0.001 | |||
| Case | 8.44 ± 3.19 | 82.32 | 5104 | ||
| Control | 4.53 ± 2.81 | 42.68 | 2646 | ||
| Total score | 472.5 | < 0.001 | |||
| Case | 45.81 ± 15.53 | 85.88 | 5324.5 | ||
| Control | 23.44 ± 12.79 | 39.12 | 2425.5 |
a P < 0.05 is considered statistically significant.
| Groups | Mean ± SD | Mean Rank | Sum of Ranks | MWU | P-Value a |
|---|---|---|---|---|---|
| Panic/agoraphobia | 246.00 | 0.002 | |||
| Case | 6.53 ± 4.07 | 37.30 | 1119.00 | ||
| Control | 3.60 ± 3.07 | 23.70 | 711.00 | ||
| Separation anxiety | 189.50 | < 0.001 | |||
| Case | 8.80 ± 4.66 | 39.18 | 1175.50 | ||
| Control | 4.43 ± 2.67 | 21.82 | 654.50 | ||
| Physical injury fears | 191.50 | < 0.001 | |||
| Case | 6.73 ± 3.49 | 39.12 | 1173.50 | ||
| Control | 3.47 ± 2.89 | 21.88 | 656.50 | ||
| Social phobia | 233.50 | 0.001 | |||
| Case | 6.60 ± 3.52 | 37.72 | 1131.50 | ||
| Control | 3.80 ± 2.12 | 23.28 | 698.50 | ||
| Obsessive compulsive | 66.50 | < 0.001 | |||
| Case | 8.63 ± 2.77 | 43.28 | 1298.50 | ||
| Control | 2.87 ± 2.64 | 17.72 | 531.50 | ||
| Generalized anxiety | 138.00 | < 0.001 | |||
| Case | 8.63 ± 3.52 | 40.90 | 1227.00 | ||
| Control | 4.17 ± 2.18 | 20.10 | 603.00 | ||
| Total score | 106.00 | < 0.001 | |||
| Case | 45.93 ± 15.99 | 41.97 | 1259.00 | ||
| Control | 22.33 ± 10.88 | 19.03 | 571.00 |
a P < 0.05 is considered statistically significant.
In Table 3, the analysis shifted to girls with non-cardiac chest pain compared to a control group. The total anxiety score for girls in the case group was 45.69, significantly higher than the control group’s score of 24.47, with significant differences noted across all subscales (P < 0.001). The subscale scores for social phobia (7.31 vs. 3.81), separation anxiety (8.59 vs. 4.41), and generalized anxiety (8.25 vs. 4.88) further indicated elevated anxiety levels among girls with chest pain.
| Scores and Groups | Mean ± SD | Mean Rank | Sum of Ranks | MWU | P-Value a |
|---|---|---|---|---|---|
| Panic/agoraphobia | 237.50 | < 0.001 | |||
| Case | 7.31 ± 4.20 | 41.08 | 1314.50 | ||
| Control | 3.81 ± 3.38 | 23.92 | 765.50 | ||
| Separation anxiety | 193.50 | < 0.001 | |||
| Case | 8.59 ± 3.82 | 42.45 | 1358.50 | ||
| Control | 4.41 ± 3.44 | 22.55 | 721.50 | ||
| Physical injury fears | 331.50 | 0.015 | |||
| Case | 6.41 ± 3.76 | 38.14 | 1220.50 | ||
| Control | 4.22 ± 2.99 | 26.86 | 859.50 | ||
| Social phobia | 297.00 | 0.004 | |||
| Case | 6.72 ± 3.96 | 39.22 | 1255.00 | ||
| Control | 3.88 ± 2.85 | 25.78 | 825.00 | ||
| Obsessive compulsive | 198.50 | < 0.001 | |||
| Case | 8.41 ± 5.35 | 42.30 | 1353.50 | ||
| Control | 3.28 ± 3.13 | 22.70 | 726.50 | ||
| Generalized anxiety | 227.00 | < 0.001 | |||
| Case | 8.25 ± 2.90 | 41.41 | 1325.00 | ||
| Control | 4.88 ± 3.29 | 23.59 | 755.00 | ||
| Total score | 144.00 | < 0.001 | |||
| Case | 45.69 ± 15.33 | 44.00 | 1408.00 | ||
| Control | 24.47 ± 14.46 | 21.00 | 672.00 |
a P < 0.05 is considered statistically significant.
Table 4 presented results for children aged 8 to 12 with non-cardiac chest pain. The case group had a total anxiety score of 48.00, significantly higher than the control group’s 22.34, with all subscales showing significant differences (P < 0.001). The subscale scores demonstrated considerable differences, including social phobia (7.18 vs. 3.40), separation anxiety (9.55 vs. 4.49), and generalized anxiety (8.68 vs. 4.34).
| Scores and Children | Mean ± SD | Mean Rank | Sum of Ranks | MWU | P-Value a |
|---|---|---|---|---|---|
| Panic/agoraphobia | 463.5 | < 0.001 | |||
| Case | 7.18 ± 4.37 | 58.97 | 2594.50 | ||
| Control | 3.40 ± 2.92 | 33.86 | 1591.50 | ||
| Separation anxiety | 339.5 | < 0.001 | |||
| Case | 9.55 ± 4.18 | 61.78 | 2718.50 | ||
| Control | 4.49 ± 3.16 | 31.22 | 1467.50 | ||
| Physical injury fears | 471.5 | < 0.001 | |||
| Case | 7.16 ± 3.64 | 58.78 | 2586.50 | ||
| Control | 3.85 ± 2.89 | 34.03 | 1599.50 | ||
| Social phobia | 479 | < 0.001 | |||
| Case | 6.77 ± 3.68 | 58.61 | 2579.00 | ||
| Control | 3.45 ± 2.52 | 34.19 | 1607.00 | ||
| Obsessive compulsive | 256.5 | < 0.001 | |||
| Case | 8.66 ± 4.59 | 63.67 | 2801.50 | ||
| Control | 2.81 ± 2.54 | 29.46 | 1384.50 | ||
| Generalized anxiety | 310 | < 0.001 | |||
| Case | 8.68 ± 3.16 | 62.45 | 2748.00 | ||
| Control | 4.34 ± 2.78 | 30.60 | 1438.00 | ||
| Total score | 183.5 | < 0.001 | |||
| Case | 48.00 ± 15.78 | 65.33 | 2874.50 | ||
| Control | 22.34 ± 12.68 | 27.90 | 1311.50 |
a P < 0.05 is considered statistically significant.
Table 5 evaluated children aged 13 to 15 with non-cardiac chest pain against a control group. The case group had a total anxiety score of 40.44, significantly higher than the control group’s score of 26.87, with a P-value of 0.008. While social phobia (6.33 vs. 4.67) did not show significant differences (P = 0.135), other subscales showed significant differences in separation anxiety (6.61 vs. 4.20, P = 0.022), generalized anxiety (7.83 vs. 5.13, P = 0.027), and obsessive-compulsive behaviors (8.17 vs. 3.93, P = 0.002).
| Scores and Children | Mean ± SD | Mean Rank | Sum of Ranks | MWU | P-Value a |
|---|---|---|---|---|---|
| Panic/agoraphobia | 93.00 | 0.135 | |||
| Case | 6.33 ± 3.50 | 19.33 | 348.00 | ||
| Control | 4.67 ± 3.94 | 14.20 | 213.00 | ||
| Separation anxiety | 72.00 | 0.022 | |||
| Case | 6.61 ± 3.62 | 20.50 | 369.00 | ||
| Control | 4.20 ± 2.86 | 12.80 | 192.00 | ||
| Physical injury fears | 101.50 | 0.229 | |||
| Case | 5.11 ± 3.16 | 18.86 | 339.50 | ||
| Control | 3.87 ± 3.20 | 14.77 | 221.50 | ||
| Social phobia | 110.00 | 0.381 | |||
| Case | 6.39 ± 3.93 | 18.39 | 331.00 | ||
| Control | 5.07 ± 2.09 | 15.33 | 230.00 | ||
| Obsessive compulsive | 50.50 | 0.002 | |||
| Case | 8.17 ± 3.42 | 21.69 | 390.50 | ||
| Control | 3.93 ± 3.75 | 11.37 | 170.50 | ||
| Generalized anxiety | 74.50 | 0.027 | |||
| Case | 7.83 ± 3.28 | 20.36 | 366.50 | ||
| Control | 5.13 ± 2.90 | 12.97 | 194.50 | ||
| Total score | 63.00 | 0.008 | |||
| Case | 40.44 ± 13.87 | 21.00 | 378.00 | ||
| Control | 26.87 ± 12.98 | 12.20 | 183.00 |
a P < 0.05 is considered statistically significant.
5. Discussion
The findings of our study provide compelling evidence for a significant association between non-cardiac chest pain and elevated anxiety levels in children and adolescents. The mean total anxiety scores in the case group reached 45.81, sharply contrasting with the control group's mean of 23.44 (P < 0.001). This substantial difference not only underscores the psychological burden associated with non-cardiac chest pain but also highlights the necessity of recognizing these symptoms as potentially rooted in anxiety disorders.
Our results are consistent with previous research, particularly that of Kenar et al. (14), which identified a similar correlation between non-cardiac chest pain and heightened anxiety levels in children in Turkey. Such consistency across studies indicates that the psychological implications of non-cardiac chest pain are not isolated phenomena but rather represent a broader clinical concern that warrants attention.
The impact of non-cardiac chest pain on psychological health cannot be overstated. In our study, anxiety scores varied significantly across several subscales, including fear of open spaces, separation anxiety, and general anxiety. These findings reveal a multifaceted nature of anxiety disorders in this population. Fear of open spaces, for instance, is particularly troubling because it may limit children's activities, leading to social withdrawal and further exacerbating feelings of anxiety. Separation anxiety, prevalent among younger children, suggests that these individuals may have difficulty coping with situations where they are away from their primary caregivers, potentially leading to heightened distress when experiencing physical symptoms such as chest pain.
The interplay between physical symptoms and psychological distress is complex; physical ailments can amplify anxiety symptoms, while anxiety can manifest as physical complaints, creating a vicious cycle that complicates diagnosis and treatment. Our findings align with the work of Uzunoglu et al. (11), who established a connection between anxiety, depressive disorders, and chest pain in pediatric populations. This correlation highlights the necessity for healthcare professionals to conduct comprehensive psychiatric evaluations in conjunction with cardiac assessments. Such evaluations can facilitate early identification of underlying psychological issues, ultimately leading to improved patient outcomes.
Moreover, the existing literature emphasizes the importance of understanding the psychological implications of non-cardiac chest pain. A comprehensive approach to patient care that includes both physical and psychological assessments can help healthcare providers develop more effective management strategies. Recognizing the interplay between these two domains is crucial for tailoring interventions that address both the physical symptoms of chest pain and the underlying psychological issues contributing to anxiety.
A noteworthy aspect of our study is the observed gender differences in anxiety levels among children with non-cardiac chest pain. Boys exhibited a total anxiety score of 45.93 compared to a control group score of 22.33, while girls scored 45.69 against a control group average of 24.47, with P-values below 0.001 in both instances. This finding aligns with existing literature that indicates a higher prevalence of anxiety disorders in females, as discussed in Asher and Aderka The pronounced anxiety levels observed in girls, particularly in subscales such as fear of open spaces and separation anxiety, further support the hypothesis that females may be more susceptible to anxiety-related conditions (15). Bal et al. (16) concluded that the level of anxiety in girls was significantly more severe than in boys, which is in line with the findings of the present study.
The gender disparities observed in our study are significant for several reasons. Firstly, they highlight the need for tailored interventions that consider the unique experiences and vulnerabilities of boys and girls. The higher anxiety levels in girls may necessitate specific therapeutic approaches that address their distinct emotional and psychological needs. Secondly, understanding these gender differences can assist healthcare providers in anticipating comorbid conditions, evaluating the severity of symptoms, and implementing diverse therapeutic interventions. It is essential for healthcare providers to be cognizant of these differences and ensure that treatment plans are adaptable to the needs of both genders.
Further analysis of anxiety levels across age groups revealed that children aged 8 to 12 exhibited particularly high anxiety scores, averaging 48.00, with significant differences across anxiety subscales. This finding is consistent with Vaughan et al., who indicated that separation anxiety is the most common anxiety disorder in this age range (17). The elevated levels of anxiety in younger children underscore the urgent need for early intervention strategies aimed at both children and their families. Early intervention is critical for preventing long-term negative outcomes associated with anxiety disorders. Studies have shown that untreated anxiety in childhood can lead to persistent issues in adolescence and adulthood, affecting academic performance, social relationships, and overall quality of life. Implementing programs that educate parents and caregivers about anxiety and its symptoms can be instrumental in facilitating timely interventions. Schools can also play a pivotal role in this process by incorporating mental health education into their curricula and providing resources for students struggling with anxiety.
Our research underscores the critical impact of family dynamics on children’s emotional health. The correlation between single-parent households and increased anxiety levels aligns with the findings of Arianpour and Abbasi (18), who noted that children facing familial disruptions, such as divorce or the death of a parent, tend to exhibit higher levels of anxiety, including separation anxiety and obsessive-compulsive behaviors. The influence of family structure on children's mental health is profound, as children often look to their caregivers for emotional support and stability. When this support is lacking due to familial strife, children may struggle to navigate their emotional landscapes, leading to heightened anxiety. Healthcare providers must consider the psychosocial environment when diagnosing and treating anxiety disorders in children. Engaging families in the treatment process can enhance the effectiveness of interventions. Providing resources for parents to better understand their children's emotional needs and teaching them how to foster a supportive environment can contribute to improved outcomes for children struggling with anxiety. Family therapy may also be beneficial in addressing underlying issues within the family unit that contribute to children's anxiety.
Rabner et al. (19) examined how worry is related to various anxiety symptoms in children and adolescents, focusing on its associations with separation anxiety disorder (SAD) and social anxiety disorder (Soc). The study involved 127 participants (aged 8 - 12 years for children and 13 - 18 years for adolescents) diagnosed with anxiety disorders. Findings showed that, although worry levels were relatively consistent across ages, its specific relationship with anxiety symptoms differed. Younger children showed a stronger association between worry and separation anxiety symptoms, while older participants exhibited a closer relationship between worry and social anxiety symptoms. This suggests that worry is a stable trait across age groups, though its effects may shift depending on age and anxiety type, highlighting its potential role in age-specific intervention strategies to better address anxiety symptoms.
The distinction between cardiac and non-cardiac causes of chest pain in pediatric patients is paramount in clinical practice. Given that most non-cardiac chest pain cases are idiopathic and linked to psychological factors, as highlighted in Kayali et al. (20), healthcare providers must remain vigilant in recognizing the potential for underlying anxiety disorders. Misinterpretation of chest pain as cardiac-related can lead to unnecessary anxiety for both the child and their family, potentially resulting in overdiagnosis and overtreatment. Proper training and education for healthcare providers regarding the psychosomatic aspects of chest pain in children are essential. Familiarizing providers with the signs and symptoms of anxiety disorders can facilitate appropriate referrals to mental health professionals. Early intervention can prevent the escalation of anxiety and improve the quality of life for children experiencing non-cardiac chest pain.
5.1. Conclusions
The study identified a significant difference in anxiety levels between children with non-cardiac chest pain and those in the control group across various age groups and subscales. Children with non-cardiac chest pain demonstrated notably higher total anxiety scores and more pronounced symptoms of social phobia, separation anxiety, and generalized anxiety. These findings underscore the psychological impact of non-cardiac chest pain, particularly in younger children and girls. The study emphasizes the necessity for targeted psychological interventions for children experiencing non-cardiac chest pain to address these elevated anxiety levels. Further research is recommended to explore the long-term psychological effects of such conditions.
5.2. Study Limitations
This study has several limitations. First, it did not account for pubertal status, which may influence anxiety, particularly in the 8- to 15-year-old age group. The observed higher anxiety levels in girls might be associated with the earlier onset of puberty, indicating a need for future studies to assess pubertal status. Additionally, environmental factors, such as family dynamics, were not examined, though they could potentially affect anxiety levels. Lastly, the use of convenience sampling limits the generalizability of the findings; future research should employ random sampling to enhance applicability and validity.