1. Background
Vitamin D receptors are widely distributed throughout the body, particularly in smooth and skeletal muscles. Research on vitamin D indicates its involvement in a variety of disturbances and diseases beyond bone metabolism in both mothers and neonates. These include pregnancy complications, such as low birth weight, preterm birth, gestational diabetes, preeclampsia, and postpartum hemorrhage. Additionally, vitamin D is associated with conditions, such as infantile eczema, asthma, infections, chronic kidney diseases, overactive bladder syndrome, pelvic floor muscle disorder, metabolic syndrome, and autoimmune disorders (1-4).
Today, vitamin D deficiency in both mothers and neonates is linked to severe outcomes in newborns. According to a recent scoping review by Palacios et al. (5), some studies have shown that vitamin D deficiency is associated with preterm birth and hyperbilirubinemia, while some others have found no significant association. Another study suggested that vitamin D is not correlated with term neonatal hyperbilirubinemia (NH) (6). Accumulating evidence indicates that vitamin D may be linked to hyperbilirubinemia in both term and preterm neonates. However, the existing findings are subject to debate.
Generally, NH is a prevalent condition worldwide, affecting approximately 80% of preterm and 60% of term neonates. Various factors have been proposed as potential causes of NH, including blood group (ABO and Rh) incompatibility, glucose-6-phosphate dehydrogenase (G6PD) deficiency, breastfeeding jaundice, sepsis, low birth weight, and prematurity (7). The role of vitamin D deficiency in the onset and severity of NH has been a subject of speculation, and its involvement in hyperbilirubinemia has not been thoroughly explored. The impact of vitamin D on NH remains a contentious issue. While there have been few studies investigating the association of vitamin D with NH, they have not specifically addressed NH in term newborns.
Our understanding of the association between vitamin D and extra-skeletal diseases, particularly NH, is still limited. It appears that additional research is needed to validate the existing findings. A potential correlation may exist between bilirubin and vitamin D levels, given that both are metabolized in the liver, albeit via two distinct and separate pathways. Changes in the production and metabolism of one could potentially influence the metabolism of the other (8). However, this remains a hypothesis that requires further investigation.
2. Objectives
The objective of this study was to compare the vitamin D levels of mothers and their healthy term neonates with physiological and out of physiological NH. Additionally, the study aimed to explore the relationship between vitamin D and NH and to provide insights into the severity of NH.
3. Methods
3.1. Study Design and Setting
This case-control study was conducted at Golestan Hospital, Tehran, Iran from October 2020 to June 2024.
3.2. Participants
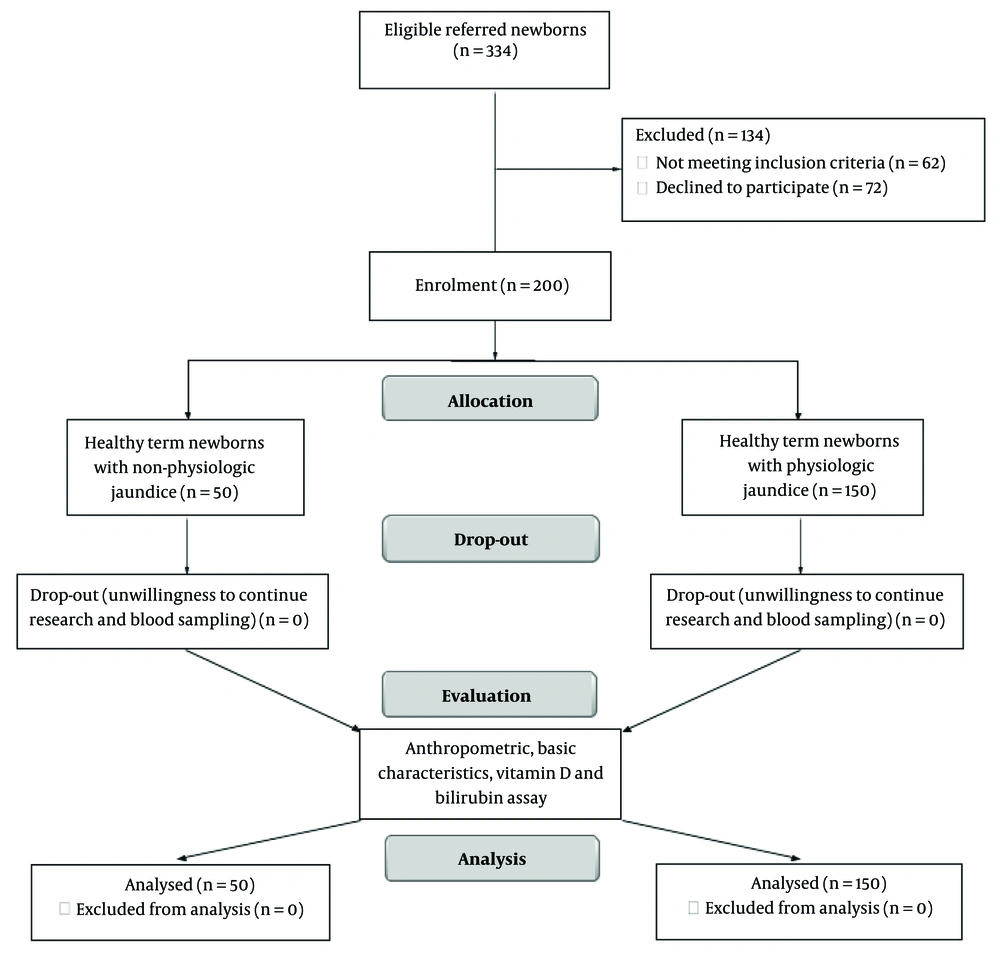
This study enrolled 200 term neonates using simple convenience sampling methods. The inclusion criteria were healthy term newborns (born after 37 weeks of gestation), who were breastfeeding and did not have any congenital anomalies or hypothyroidism. The exclusion criteria included preterm newborns, newborns with ABO and Rh incompatibility, G6PD deficiency, asphyxia, sepsis, meconium aspiration, low birth weight, and prematurity. Mothers with renal and hepatic diseases, diabetes, and those taking anticonvulsant medications were also excluded from the study.
The control of confounders and matching of groups was achieved through the restriction of subjects, stratification of pooled data, and matching of the basic characteristics of the participants. By restricting the subjects to two groups with a gestational age of more than 37 weeks and excluding preterm newborns, confounding variables were minimized. Factors, such as age, time of referral to the hospital, geographic area, and source population, were chosen as ‘matching criteria’ to ensure similarity between the control and case groups. The main confounders were eliminated through careful consideration of the inclusion and exclusion criteria and strict adherence to the study’s enrollment criteria. Additionally, the basic characteristics (gender, age, weight, height, Body Mass Index (BMI), mothers’ education, gravidity, and delivery type) were matched between the two groups. For effect modification, pooled variables were categorized to stratify variables, which were then compared and analyzed. Upon using the following formula and considering a dropout rate of 20%, at least 40 newborns were considered for the case group and 120 newborns for the control group.
where P˳ = 30%, OR = 2, α = 5%, β = 10% and C = 3. There were no dropouts due to loss of follow-up in this study. Ultimately, 200 neonates were enrolled. Overall, 150 newborns with bilirubin levels within the physiological range were designated as the control group, and 50 newborns with bilirubin levels outside the physiological range were classified as the case group (as depicted in Figure 1, the study’s flow diagram).
3.3. Vitamin D and Bilirubin Assays
Bilirubin levels were estimated using the Jendrassik-Grόf FS method, a photometric test for assessing bilirubin in serum. The 25-hydroxy vitamin D levels were measured using ELISA kits (Pishtaz Teb Company, Tehran, Iran). The intra-assay and inter-assay variation coefficients were 3.4% and 15.8%, respectively, with a sensitivity of 1.98. Blood samples were collected from all mothers and their newborns between the 3rd and 5th days postpartum. These samples were then sent to the Golestan Hospital Laboratory and stored at -20˚C. Bilirubin levels of ≤ 12 ng/dL were considered within the physiological range. Vitamin D levels were categorized as follows: Deficiency (< 20 ng/mL), insufficiency (20 - 29 ng/mL), and optimal (≥ 30 ng/mL) (8).
3.4. Main Outcome Measures
The main outcome measure of the study was defined as the relationship between the vitamin D levels of newborns and their mothers and the bilirubin status of the subjects.
3.5. Statistical Analysis
Quantitative data were presented as frequency and percentage, while qualitative data were expressed as mean and standard deviation (SD). Differences between variables in each group were compared using the chi-square test and Student’s t-test. The Pearson’s linear correlation test was utilized to determine the correlation between bilirubin status and both laboratory variables and general data. Variables that showed significant differences between the two groups were included in three regression models to identify predictors.
Model one examined the neonatal vitamin D versus maternal vitamin D, adjusted for neonatal anthropometric characteristics (such as gender, weight, height, age, and bilirubin level) and maternal anthropometric characteristics (such as age, weight, height, BMI, delivery type, gravidity, and education). Model two analyzed the neonatal bilirubin level versus maternal vitamin D, adjusted for neonatal gender, weight, height, age, and vitamin D, as well as maternal age, weight, height, BMI, delivery type, gravidity, and education. Model three compared the newborns’ bilirubin levels versus the newborns’ vitamin D levels, adjusted for neonatal gender, weight, height, and age, as well as maternal age, weight, height, BMI, delivery type, gravidity, education, and vitamin D. A Multivariate logistic Regression analysis was used to assess the risk factors for hyperbilirubinemia by calculating the odds ratio (OR) at a 95% confidence interval (CI). Data analyses were performed using SPSS version 24, and a P-value of less than 0.05 was considered statistically significant.
3.6. Ethics Statement
Informed consent was obtained from the mothers, and all participants’ information was kept confidential. This study received ethical approval from the Ethics Committee of AJA University of Medical Sciences (Tehran, Iran) (IR.AJAUMS.REC.1400.192).
4. Results
In this study, a total of 200 subjects were analyzed, with 50 newborns in the case group and 150 newborns in the control group. The subjects included 103 boys (51.5%) and 97 girls (48.5%). The mean age of mothers in the case group was 28.5 ± 2.5 years, and the mean age of their newborns was 4.5 ± 0.59 days. Meanwhile, in the control group, the mothers’ mean age was 27.5 ± 3.75 years, and the mean age of their newborns was 4.5 ± 0.58 days. Based on the findings, the mean bilirubin level was 14.66 ± 1.05 ng/dL in the case group and 9.55 ± 1.28 ng/dL in the control group. The demographic characteristics of both groups are presented in Table 1. There was no significant difference in terms of anthropometric characteristics between the two groups.
| Variables | Case Group | Control Group | P-Value |
|---|---|---|---|
| Neonates | |||
| Gender | 0.68 | ||
| Boy | 27 (54) | 76 (51) | |
| Girl | 23 (46) | 74 (49) | |
| Age (d) | 4.5 ± 0.59 (3 - 5) | 4.5 ± 0.58 (3 - 5) | 0.96 |
| Weight (kg) | 3.43 ± 0.49 (2.7 - 4.2) | 3.41 ± 0.53 (2.9 - 4.3) | 0.93 |
| Height (cm) | 51.1 ± 1.67 (48 - 54) | 52 ± 1.63 (47 - 55) | 0.87 |
| Bilirubin (ng/dL) | 14.66 ± 1.05 (13.1 - 19) | 9.55 ± 1.28 (7.3 - 11.7) | 0.001 |
| Mothers | |||
| Age (y) | 28.5 ± 2.5 (22 - 33) | 27.5 ± 3.75 (18 - 36) | 0.15 |
| Weight (kg) | 65.12 ± 8.63 (47 - 83) | 63.5 ± 9.21 (47 - 90) | 0.25 |
| Height (cm) | 163.8 ± 5.25 (154 - 175) | 162.8 ± 4.92 (152 - 174) | 0.27 |
| BMI before pregnancy | 24.3 ± 3.66 (18 - 31) | 24.06 ± 3.73 (17 - 36) | 0.81 |
| BMI pregnancy (kg/m2) | 29.27 ± 3.49 (22.49 - 35.69) | 29.1 ± 3.58 (21.61 - 37.73) | 0.85 |
| Weight gain (kg) | 13.5 ± 2.21 (8 - 19) | 13.72 ± 2.07 (8 - 20) | 0.49 |
| Gravid | 1 | ||
| 1 | 20 (40) | 60 (40) | |
| 2 | 29 (58) | 87 (58) | |
| 3 | 1 (2) | 3 (2) | |
| Education | 0.07 | ||
| < Diploma | 18 (36) | 67 (45) | |
| Diploma | 17 (34) | 16 (11) | |
| > Diploma | 15 (30) | 67 (45) | |
| Delivery | |||
| Cesarean | 42 (84) | 110 (73) | |
| Vaginal | 8 (16) | 40 (27) | 0.14 |
The main variables that showed significant differences were evaluated in three regression models to identify the predictors. A Multivariate logistic Regression analysis was employed to assess the risk factors for hyperbilirubinemia, based on OR at a 95% CI (Table 2). A direct correlation was observed between the vitamin D levels of newborns and their mothers in both the case group (r = 0.74, P = 0.01) and the control group (r = 0.77, P = 0.01). Moreover, a significant negative correlation was found between the newborns’ bilirubin levels and the vitamin D levels of newborns and their mothers in the case group (r = -0.34, P = 0.02 and r = -0.21, P = 0.04, respectively). Additionally, a significant negative correlation was detected between the newborns’ bilirubin levels and the vitamin D status of newborns and their mothers in the control group (r = -0.41, P = 0.01 and r = -0.42, P = 0.01, respectively).
| Variables and Correlation | Correlation Coefficient (r) | 95 % CI for (r) Lower to Upper | P-Value b |
|---|---|---|---|
| Case | |||
| Newborn vit D vs. maternal vit D c | 0.74 | 0.544 to 0.857 | 0.01 |
| Newborn Bilirubin vs. maternal vit D d | -0.21 | -0.453 to 0.046 | 0.04 |
| Newborn Bilirubin vs. newborn vit D e | -0.34 | -0.548 to 0.052 | 0.02 |
| Control | |||
| Newborn vit D vs. maternal vitamin D c | 0.77 | 0.67 to 0.89 | 0.01 |
| Newborn Bilirubin vs. maternal vit D d | -0.42 | -0.54 to -0.27 | 0.01 |
| Newborn Bilirubin vs. newborn vit D e | -0.41 | -0.54 to -0.26 | 0.01 |
Correlation Analysis Among Bilirubin with Vitamin D of Babies and Their Mothers in Both Groups a
Newborns in the case group exhibited significantly lower mean vitamin D levels compared to those in the control group (27.8 ± 10.04 ng/mL vs. 33.9 ± 9.39 ng/mL). Furthermore, they were approximately twice as likely to have vitamin D insufficiency compared to those in the control group (crude OR = 2.63 at 95% CI: 1.35 - 5.1; adjusted OR = 1.98 at 95% CI: 0.9 - 2.1; P = 0.006). Mothers in the case group exhibited lower vitamin D levels compared to those in the control group (20.56 ± 10.2 ng/mL vs. 26 ± 8.92 ng/mL). They were also approximately twice as likely to have vitamin D insufficiency when compared to mothers in the control group (crude OR = 2.98 at 95% CI: 1.39 - 6.4; adjusted OR = 1.95 at 95% CI: 0.89 - 2; P = 0.001).
Furthermore, the pooled vitamin D levels in newborns and their mothers were categorized to minimize the impact of confounding variables. After this stratification, the specific variables within each stratum were re-analyzed. In the case group, the frequency of vitamin D deficiency and insufficiency in newborns was found to be 14 (28%) and 10 (20%) cases, respectively. In contrast, in the control group, there were 15 (10%) cases of deficiency and 20 (13.3%) cases of insufficiency, and the difference was statistically significant (P = 0.007). In the case group, the frequency of vitamin D deficiency and insufficiency in mothers was 30 (60%) and 10 (20%) cases, respectively. In the control group, these frequencies were lower, with 53 (35.3%) cases of deficiency and 26 (17.3%) cases of insufficiency (P = 0.006). Additionally, the vitamin D levels of both newborns and their mothers were significantly lower in the case group compared to the control group (P < 0.05) (Table 3). It appears that the vitamin D levels in both newborns and their mothers played a significant role in NH.
| Variables | Case Group | Control Group | Crude OR 95% CI (Lower - Upper) | Adjusted OR 95% CI (Lower - Upper) | P-Value |
|---|---|---|---|---|---|
| Neonates vitamin D (ng/mL) | 27.8 ± 10.04 (12 - 50) | 33.9 ± 9.39 (9 - 65) | 2.63 (1.3 - 5.1) | 1.98 (0.9 - 2.1) | 0.006 |
| < 20 | 14 (28) | 15 (10) | 0.007 | ||
| 20 - 30 | 10 (20) | 20 (13.3) | |||
| > 30 | 26 (52) | 115 (76.7) | |||
| Maternal vitamin D (ng/mL) | 20.56 ± 10.2 (8 - 45) | 26 ± 8.92 (9 - 55) | 2.98 (1.39 - 6.4) | 1.95 (0.89 - 2) | 0.001 |
| < 20 | 30 (60) | 53 (35.3) | 0.006 | ||
| 20 - 30 | 10 (20) | 26 (17.3) | |||
| > 30 | 10 (20) | 71 (47.4) |
5. Discussion
The objective of this study was to evaluate the ongoing debates regarding the relationship between NH and the vitamin D status of neonates and their mothers and to propose a research agenda to clarify areas of uncertainty. The frequency of vitamin D deficiency and suboptimal levels was significantly higher in cases of non-physiological NH. Additionally, a significant negative correlation was observed between the newborns’ bilirubin level and the vitamin D status of newborns and their mothers, with this correlation being more pronounced in the case group.
5.1. Correlation of Maternal Vitamin D Status with the Newborns’ Vitamin D Levels and Neonatal Hyperbilirubinemia
Vitamin D deficiency and insufficiency are common in neonates born to mothers who also have vitamin D deficiency. Nonetheless, the correlation between the vitamin D status of newborns and their mothers is a subject of debate. Some studies have found no significant relationship between the vitamin D status of neonates and the vitamin D level of their mothers (8). On the other hand, some studies have reported a significant correlation between the vitamin D status of neonates and the vitamin D level of their mothers (9). In this regard, a previous study demonstrated a correlation between the vitamin D levels of mothers and their neonates. Interestingly, this correlation was found to be stronger in full-term newborns compared to preterm ones (10). Moreover, Mohaghegh et al. (11) discovered a significant correlation between the vitamin D levels of mothers and their neonates. Interestingly, this relationship was stronger in mothers with preeclampsia compared to those with normal pregnancies. Additionally, our study demonstrated a correlation between the vitamin D levels of neonates and their mothers.
Insufficient vitamin D supplements, high BMI, and weight gain are the primary causes of maternal vitamin D deficiency. These factors may influence both gestational and neonatal outcomes. However, the existing findings on this subject are contradictory (12). A cohort study established an association between maternal vitamin D deficiency and NH (13). Moreover, a study conducted in Iran revealed that 58.4% of pregnant women were deficient in vitamin D. This deficiency was found to be associated with various feto-maternal outcomes, including cesarean section, maternal hypertension, neonatal respiratory infection, and NH. Therefore, it appears that maternal vitamin D deficiency could potentially pose a risk to the health of newborns (14). Three meta-analysis studies have indicated that vitamin D supplementation can reduce NH and neonatal hospitalization. Consequently, the early use of vitamin D supplements during pregnancy is recommended (15-17).
5.2. Relationship Between Neonatal Vitamin D Status and Neonatal Hyperbilirubinemia
Generally, NH is a prevalent condition among neonates, with multiple factors contributing to its occurrence. However, the relationship between vitamin D status and NH remains uncertain and subject to debate. A case-control study involving 60 term neonates, including 30 term icteric neonates and 30 healthy control neonates, found no association between vitamin D status and NH (6). In this study, the vitamin D levels of mothers were not measured. However, another case-control study involving 60 term neonates (30 neonates with NH and 30 neonates without NH) and their mothers found that vitamin D levels were significantly lower in neonates with NH. This suggests a potential relationship between the vitamin D status and NH (8). It should be noted that the two aforementioned studies were only conducted on two groups of newborns, including those with and without NH. However, they did not employ an appropriate statistical test (Pearson’s linear correlation test) to evaluate the relationship. In contrast, our study examined vitamin D levels in 50 neonates with non-physiological NH and 150 neonates with physiological NH, as well as their mothers.
Moreover, another study revealed that 71% of neonates in a jaundice clinic were deficient in vitamin D. It was suggested that the appropriate and timely administration of vitamin D supplements could potentially reduce hospitalization rates and instances of NH (18). Additionally, Bhat et al. (19) discovered that newborns with bilirubin levels outside the physiological range had lower vitamin D levels compared to those with bilirubin levels within the physiological range. This study, which involved 100 neonates and their mothers (50 subjects with physiological NH and 50 subjects with non-physiological NH), found a negative correlation with NH that was outside the physiological range; the findings of this research were consistent with our study. However, our study demonstrated a significant negative correlation between the vitamin D status and NH in both groups, with this correlation being more pronounced in the case group.
Additionally, a cross-sectional study involving 100 neonates found that the prevalence of vitamin D deficiency was 38% in newborns. Furthermore, a significant association was observed between the vitamin D status of newborns and NH (20). A meta-analysis found that newborns with NH had lower vitamin D levels compared to those without NH. The study suggested that newborns with lower vitamin D levels were at a higher risk for NH. It was also indicated that the observed differences in bilirubin levels could be attributed to varying levels of vitamin D (21). Overall, pediatricians and healthcare professionals should be cognizant of the impact of vitamin D deficiency on NH and communicate this to parents. It is advisable to create an informative leaflet that simplifies these instructions. This leaflet could be then disseminated among general practitioners and mothers. Such a leaflet, while simple, could serve as an effective measure to enhance vitamin D consumption in infants and could be implemented as a reliable guideline (22).
A limitation of this study was its focus on infants from a single geographic area. Results may vary across different populations, potentially leading to inconsistent findings. Future research should aim to include diverse populations from various regions. The purpose of the current study was to consolidate the existing evidence and provide a clear interpretation of the issue. However, further research is necessary to strengthen our understanding and scientific knowledge on this topic. It is recommended that a randomized clinical trial with a sufficient number of subjects be conducted to assess the impact of vitamin D supplementation on the severity of NH and its treatment to help validate these findings.
5.3. Conclusions
Based on the findings of this study, the level of vitamin D was significantly lower in newborns with non-physiological NH compared to those with physiological NH. Moreover, a significant negative correlation was observed between the newborns’ bilirubin levels and the vitamin D status of both newborns and their mothers. This correlation was more pronounced in cases of non-physiological NH. This suggests that vitamin D levels in both newborns and their mothers might play a crucial role in NH. This study could serve as an initial step towards understanding the causes of NH and improving its treatment.