1. Background
Developmental dysplasia of the hip (DDH) is one of the most common abnormalities in infants and children (1, 2). In these patients, the head of the femur has an abnormal relationship with the hip and does not fit properly next to the pelvic bone, which can manifest as subluxation, dysplasia, and dislocation (3). Dysplasia is a condition characterized by increased obliquity and decreased concavity of the acetabulum with a normal Shenton’s line on radiographs. This condition can cause problems and complications, such as joint instability and multiple dislocations (2, 4, 5).
If left untreated, hip dysplasia may lead to dislocation, and the child may have an abnormal gait and, as a result, hip pain (6). If the dislocation persists, the current gold standard is fluoroscopy-guided closed reduction followed by spica cast immobilization under general anesthesia for 6 to 12 months (7). However, even with early treatment, the success rate of closed reduction for DDH is highly variable, ranging from 40% to 90% in studies (8). Open reduction with or without pelvic and femoral osteotomy is considered for cases where closed reduction has failed and for patients with late manifestations (8, 9).
Two common open approaches include the medial approach or the anterior approach. The application of the medial approach is restricted in younger children because it limits the ability to perform a pelvic osteotomy or capsulectomy at the same time, if necessary. In addition, the blood supply to the femoral head is more at risk, and therefore the popularity of this method has decreased (7, 10). Most researchers prefer the modified Smith-Petersen anterolateral approach, which allows for simultaneous pelvic osteotomy and capsulorrhaphy (11). Cases of severe hip dislocations that fail even after open reduction have been reported. Re-dislocation after open reduction has ranged from 0 to 14% in various studies (7).
Failure of open reduction is a serious complication. Complications associated with DDH surgical treatment include joint subluxation, subluxation-redislocation, implant loosening, avascular necrosis (AVN) of the femoral head, lower limb length discrepancy, infection, joint stiffness, non-union of the osteotomy line, sciatic nerve injury, and graft problems (12, 13). Successful treatment of DDH, as well as monitoring of surgical complications, can be assessed based on radiographs and clinical assessments (13). The rate of successful treatment of DDH with open reduction has varied in different studies, and previous studies have paid less attention to the importance of capsulorrhaphy.
2. Objectives
The present study aimed to investigate the clinical and radiological results of anterior open reduction in DDH patients.
3. Methods
3.1. Study Design and Participants
This retrospective descriptive-analytical study was conducted on 36 DDH patients undergoing surgical treatment with open reduction at Golestan Hospital, Ahvaz, from 2022 to 2024. Inclusion criteria were a definitive diagnosis of idiopathic DDH undergoing open reduction surgery, and age between 8 months and 8 years at the time of surgery with a minimum follow-up of 9 months. Patients with a follow-up of less than 9 months, concomitant neuromuscular diseases, teratologic dislocations, and failure of previous open reduction were exclusion criteria. Patients with previous closed reduction were not excluded from the study.
All reductions were anterior, with adductor release, and all were performed with capsulorrhaphy. However, some cases also required derotational osteotomy and shortening of the femur and Salter osteotomy of the pelvis. All eligible patients underwent clinical and radiological examinations before surgery and at least 9 months after open reduction.
3.2. Clinical Evaluation of Patients
Clinical evaluation of patients was performed using McKay’s criteria: (1) Excellent (stable joint, painless, no lameness, negative Trendelenburg sign, and full joint movements); (2) good (stable joint, painless, slight lameness, and slight reduction of joint movements); (3) moderate (stable joint, painless, positive Trendelenburg sign, and limited joint movements); (4) poor (unstable joint with pain or pain and positive Trendelenburg sign).
Radiographic evaluation of patients was performed using Severin’s score, Acetabular Index (AI), central edge angle (CEA), and the International Hip Dysplasia Institute (IHDI) classification. Preoperative radiographs were available for all patients and were used to determine the AI and the degree of hip dislocation based on the Tonnis grading system. Radiographic evaluation of treatment results was performed based on Severin’s classification using the patients’ last follow-up radiographs. The presence of osteonecrosis of the femoral head was assessed using the Kalamchi and MacEwen classification criteria.
The CEA was measured to assess residual acetabular dysplasia, and the Severin score was calculated based on AP pelvic radiography to evaluate radiographic findings (presence of femoral head and femoral neck abnormalities or subluxation). The IHDI criterion was used to assess the exact location of the femoral head in front of the acetabulum joint before and after reduction, according to the pelvic radiography before and after open reduction. The AVN screening was based on X-rays, and MRI screening was performed only for patients with clinical or radiological signs of AVN.
Regarding the suture material used in capsulorrhaphy, a 1.0 Vicryl suture was utilized, and the tension was applied only to the extent necessary to remove the redundant capsule, without exerting any pressure on the femoral head. Additionally, a Salter osteotomy was performed in all cases.
3.3. Statistical Analysis
Statistical analysis was performed using SPSS software Version 22 (IBM, Chicago, USA). The quantitative and qualitative variables were indicated as mean ± SD and number (%), respectively. Kolmogorov-Smirnov and Shapiro-Wilk tests were used to test for the distribution. Differences were compared using the paired t-test. A P-value of less than 0.05 was considered statistically significant. A post-hoc power analysis was performed to assess the adequacy of the sample size for detecting changes in radiological parameters before and after open reduction in DDH patients. With 36 paired observations, a two-tailed paired-samples t-test with an alpha level of 0.05 achieved a power > 0.99, confirming the sample size was sufficient. Furthermore, an a priori power analysis indicated that only 15 patients would be required to detect a large effect size (d = 0.8) with 80% power. Therefore, the current sample size is adequate to detect meaningful radiological improvements postoperatively.
4. Results
The mean age of participants was 34.36 ± 16.34 months. The minimum and maximum ages were 12 months and 96 months, respectively. 88.89% of patients were girls (n = 32). The frequency of unilateral left or right hip dysplasia in patients undergoing open reduction was 30.56% and 25%, respectively. The frequency of femoral osteotomy zero and one were both 50% (n = 18). During the clinical evaluation of patients based on McKay’s criteria, excellent, good, and moderate results were seen in 44.44%, 50%, and 5.56%, respectively. More details are provided in Table 1.
| Variables | Results |
|---|---|
| Age (mean ± SD) | 34.36 ± 16.34 |
| Sex | |
| Girl | 32 (88.89) |
| Boy | 4 (11.11) |
| Frequency of hip dysplasia involvement | |
| Right (unilateral) | 9 (25) |
| Left (unilateral) | 11 (30.56) |
| Bilateral (right) | 7 (19.44) |
| Bilateral (left) | 9 (25) |
| Femoral osteotomy | |
| 0 | 18 (50) |
| 1 | 18 (50) |
| Clinical evaluation based on McKays criteria | |
| Excellent | 16 (44.44) |
| Good | 18 (50) |
| Moderate | 2 (5.56) |
| Poor | 0 |
Demographic and Clinical Features of Patients a
The preoperative CEA was zero for all but one patient. This value was 14 for one patient. Therefore, before surgery, the mean CEA was 0.39 ± 2.33. After open reduction, the mean was 33.56 ± 8.12. The results indicate the beneficial effect of open reduction on the CEA (P = 0.001).
Based on our results, before and after surgery, the mean values of the acetabulum angle were 39.67 ± 4.37 and 24.28 ± 5.90, respectively. This indicated the beneficial effect of surgery in reducing the acetabulum angle (P = 0.001). After surgery, all patients had Tonnis grade 1 (Table 2). Based on the grading of the proximal femoral metaphysis position before surgery, grade 2, grade 3, and grade 4 were found in 5.56%, 16.67%, and 77.78% of patients, respectively. After surgery, all patients were grade 1. A Cohen’s d of 5.56 indicates an extremely large effect size, reflecting a dramatic improvement in CEA post-surgery, and a Cohen’s d of 2.97 indicates a very large effect size, suggesting a substantial improvement in acetabular angles post-surgery. For the Tonnis Scale and proximal femoral metaphysis grading, we calculated Cramer’s V (0.958 and 0.972, respectively) based on dichotomized McNemar’s tests, reflecting very strong associations due to the complete shift to grade 1 post-surgery.
| Variables | Before Surgery | After Surgery | P-Value | Effect Size |
|---|---|---|---|---|
| Radiological evaluation based on changes in acetabular angles (°) | 39.67 ± 4.37 | 24.28 ± 5.90 | 0.001 | 2.97 b |
| CEA (°) | 0.39 ± 2.33 | 33.56 ± 8.12 | 0.001 | 5.56 b |
| Tonnis Scale | ||||
| 1 | 1 (2.78) | 36 (100) | 0.958 c | |
| 2 | 7 (19.44) | 0 | ||
| 3 | 2 (5.56) | 0 | ||
| 4 | 26 (72.22) | 0 | ||
| Grading the position of the proximal femoral metaphysis | ||||
| Grade 1 | 0 | 36 (100) | 0.972 c | |
| Grade 2 | 2 (5.56) | 0 | ||
| Grade 3 | 6 (16.67) | 0 | ||
| Grade 4 | 28 (77.78) | 0 |
Radiological Evaluation of Developmental Dysplasia of the Hip Patients Before and After Open Reduction a
The AVN was assessed according to the criteria of Kalamchi and MacEwen on at least 9-month follow-up radiographs. In 35 cases (97.22%), no specific radiological changes in the bone were observed (stage zero). One patient (2.78%) was stage one, which indicates minor painful changes in the bone.
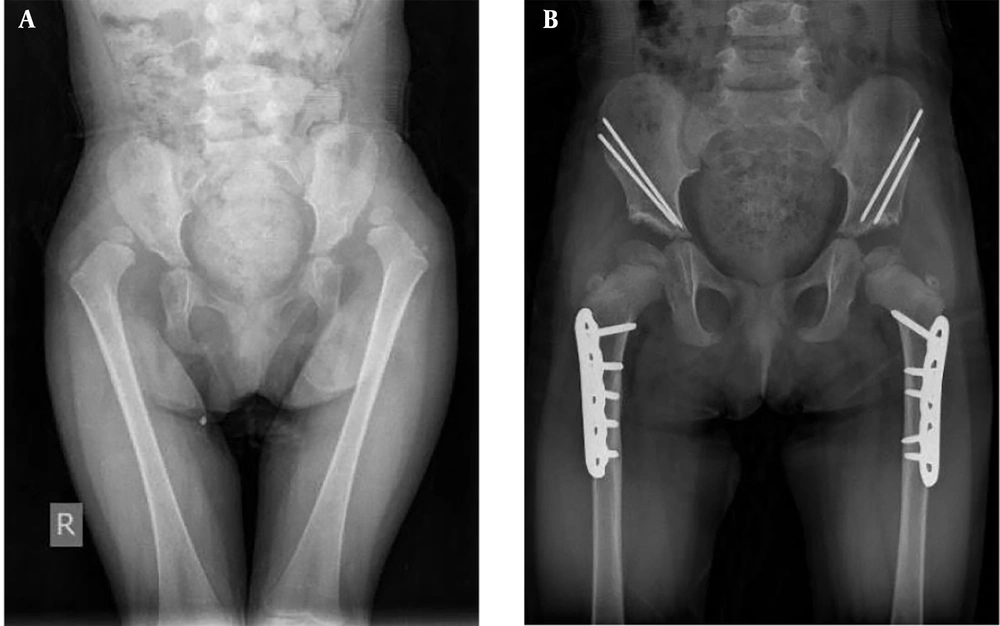
Figure 1A and B show the patient’s radiographic images before and after the open reduction procedure. This patient with bilateral DDH underwent Salter and femoral osteotomy on both sides. The clinical criteria for this patient were good after surgery.
5. Discussion
The present study aimed to investigate the clinical and radiological results of open arthroplasty in patients with DDH. Radiological evaluation of patients based on the Tonnis criteria showed that the values of the acetabular angle before and after the surgery were 39.67 ± 4.37 and 24.28 ± 5.96, respectively (P = 0.001). The CEA before and after the operation was 0.39 ± 2.33 and 33.56 ± 8.12, respectively. The results indicate a significant effect of the operation on the CEA. Before open reduction, Tonnis grades 1, 2, 3, and 4 were reported in 2.78%, 19.44%, 5.56%, and 72.22% of patients, respectively.
Based on our findings, the mean age of patients was 34.3 ± 16.4 months. In the study by Gunel et al. and Turkozu et al., the mean age was 25.6 months (range 12 - 44 months) and 12.1 months (range 3 - 18 months), respectively (14, 15).Based on the grading of the proximal femoral metaphysis position before surgery, grades 2, 3, and 4 were found in 5.56%, 16.67%, and 77.78% of patients, respectively.
In our study, during the clinical evaluation of patients based on McKay’s criteria, excellent, good, and moderate results were reported in 44.44%, 50%, and 5.56%, respectively. In the study by Turkozu et al., which aimed to evaluate the results of the open reduction technique with an internal approach in 3 - 18 month-old infants, the study included 28 hip operations from 19 patients. Based on McKay’s criteria, 78.6% and 21.4% were excellent and good, respectively (15). Piskin et al. have reported 82.5% excellent and 17.5% good outcomes in their case series of 40 hips (16).
Similar to our findings, Sener et al. reported final clinical results that were excellent in 52.9%, good in 29.4%, moderate in 11.8%, and poor in 5.9% of hips (17). The results of our study showed that the mean values of the acetabular angle before open reduction treatment were 39.67 ± 4.37 degrees, and the acetabular angle decreased after the surgery to 24.28 ± 5.96 degrees. The study conducted by Gunel et al. showed that the hip was evaluated using the AI for the development of AVN and re-dislocation. Based on clinical findings, 97.3% of patients had excellent and good results. The acetabulum angle decreased from 45 degrees preoperatively to 21 degrees in the early postoperative period and improved to 18 degrees at the last follow-up (14).
A wide range of AVN incidence values between 0% and 67% have been reported in studies (18-20). In our study, the incidence of AVN was 2.78% during the 9-month follow-up. In the studies by Turkozu et al. and Cummings et al., the incidence of AVN was 10.7% and 13%, respectively (15, 21). Gardner et al. also showed that the overall rate of AVN at 5 years follow-up was 32.9%, with type 2 AVN accounting for the majority of these cases (19).
The lower incidence of AVN observed in our study compared to most previous reports, despite similar surgical techniques, may be attributed to several factors. These include stricter patient selection criteria, differences in perioperative management, postoperative care protocols, and subtle variations in the execution of surgical steps, such as gentle soft tissue handling and minimizing vascular compromise. Additionally, the consistency and experience of the surgical team may have contributed to these favorable outcomes, even if not explicitly measured. On the other hand, for a number of patients, the follow-up period was at least 9 months, which is not enough time to fully investigate necrosis and re-dislocation of the femoral head, and this is one of the limitations of our study.
5.1. Conclusions
Open reduction was associated with significant improvements in the AI and CEA. Moreover, our findings indicate a low rate of AVN (2.78%) and satisfactory short-term outcomes after open reduction. With open reduction, no re-dislocation was observed. It is recommended that further multicenter studies with larger sample sizes and longer follow-up be conducted to confirm these results. Therefore, examining clinical or radiological outcomes for patients with DDH treated with open reduction may help physicians make more informed decisions about patient management strategies.
5.2. Limitations
The limitations of the present study lie in its single-center retrospective design, which may introduce selection bias, as well as the small patient sample size and relatively short follow-up period.