1. Background
Congenital lung malformation (CLM) is a rare condition with high incidence of mortality and morbidity. Presentations of congenital lung disease are various depending on their time of detection. Antenatal manifestations of the disease include intrathoracic mass, pleural effusion, fetal hydrops, oligohydramnios, or polyhydramnios. Newborn patients present respiratory distress, stridor, bubbly secretions in mouth, inability to swallow, failure to pass the nasogastric tube, inability to establish an airway, cardiac failure, cyanosis, and poor respiratory effort. Finally in later childhood/adulthood, the disease manifests recurrent infection, hemoptysis, hemothorax, bronchiectasis, bronchopleural fistula, steroid-resistant airway obstruction, cardiac failure, malignant transformation, cyanosis, coughing on drinking, accidental finding of mass or hyper lucent area on chest radiograph, and air embolism (1).
CLM is often discovered incidentally on routine prenatal ultrasound or postnatal imagings. The prognosis depends on the size of lesion and the degree of functional impairment caused by the lesion. Small lesions could remain asymptomatic for a while after birth. Malformations consist of abnormal structures in the pulmonary airway, sacs (alveoli), blood vessels, and lymphatic drainage. Malformations develop in several forms, ranging from pulmonary agenesis, total absence of lung parenchyma with no bronchial or vascular supply, to pulmonary aplasia, an undeveloped bronchus that is open only to a blind pouch with no evidence of pulmonary vasculature or lung parenchyma, and finally, pulmonary hypoplasia, a rudimentary bronchus and lung, with a dwindled number and size of alveoli, airways, and vessels. Bronchogenic cysts are considerably the most common cystic lesions of the middle mediastinum.
Their main manifestations are recurrent infection, wheezing, atelectasis, and air trapping due to partial or complete airway compression in the late childhood. Pulmonary sequestration refers to a nonfunctioning lung parenchyma, separated from the tracheobronchial tree with an anomalous systemic arterial supply.
In spite of major progressions in detection of fetal lung abnormalities using ultrasound imaging and fetal anomaly scanning, detection of CLM in antenatal period is still difficult. Moreover, identifying an intrathoracic anomaly in the antenatal period is suggestive for further investigations and the possibility for intrauterine therapy. In addition, an early detection offers the opportunity of early postnatal surgical intervention. Many of these lesions can be detected around 20 weeks of gestation; but, diaphragmatic hernias and pleural effusion somehow present later in pregnancy (1).
2. Objectives
This study aimed to report and investigate the features and prognoses of CLM patients, admitted to the Pediatric Pulmonary Ward of Masih Daneshvari Hospital in an 8-year period (from 2002 to 2010).
3. Materials and Methods
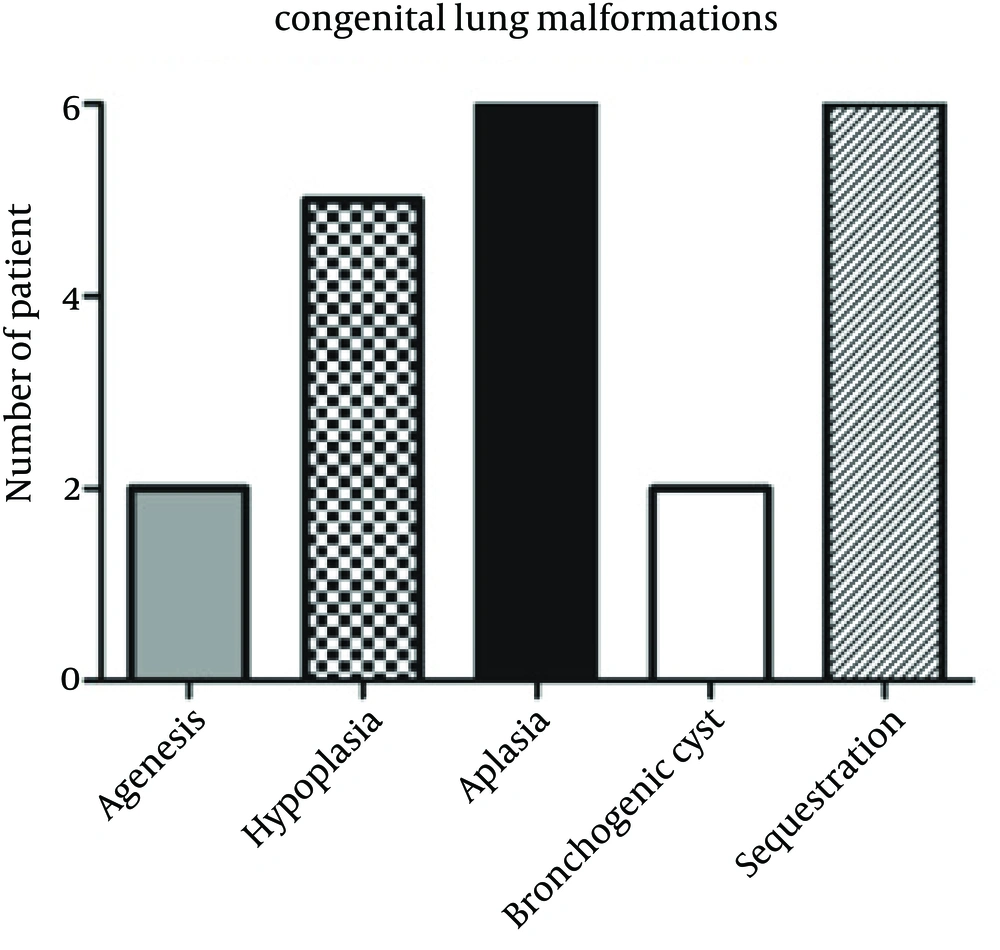
This was a retrospective study evaluating the medical records of 21 patients (12 females, nine males) with mean age of 7.3 years (ranging from 1 month to 16 years.). All patients were histopathologically diagnosed with CLM. Patients' demographic data including age, sex, and clinical signs and symptoms were recorded. To confirm the diagnoses, patients underwent bronchoscopy, angiography and some other diagnostic procedures. Patients were divided into several subgroups based on their malformations and types of involvements including agenesia, hypoplasia, aplasia, bronchogenic cyst and sequestration. This study was conducted on children hospitalized in the Pediatric Pulmonary Department of Masih Daneshvari Hospital during an 8-year period.
4. Results
Out of 21 patients, two were diagnosed with agenesis, five with hypoplasia, six with aplasia, two with bronchogenic cyst, and six with sequestration (Figure 1). All patients were symptomatic at the time of diagnostic workup. The most common clinical signs and symptoms were respiratory distress and recurrent pulmonary infection. Children's age at the time of diagnosis was indicative of delayed diagnosis. A few patients were treated symptomatically, and the rest were under follow up with conservative treatment. None had developed hydrops in their fetal period (Table 1). Two cases underwent surgery due to pulmonary sequestrations in the middle and inferior lobes and both were discharged on the same day with good general conditions (Table 1). One patient expired from hypoplasia complicated with congenital heart disease. In the follow up, two surgical cases showed excellent improvements and became asymptomatic in the following month (Table 1). Six patients with the diagnosis of pulmonary sequestration underwent angiography before surgery and based on the angiography results, were categorized into intra- and extra-pulmonary subdivisions. Two patients had intralobar sequestration and were good candidates for pulmonary resection. After the operation, they became asymptomatic. Table 1 presents the course of CLM in our patients.
| Patients, No. | Clinical Course |
|---|---|
| Agenesis, 2 | 2 patients were symptomatic. Symptoms were managed conservatively, good outcome |
| Hypoplasia, 5 | One died of pulmonary hypertension and cardiac complication, four managed conservatively with good outcome |
| Aplasia, 6 | 6 patients were symptomatic. Symptoms managed conservatively with good outcome |
| Bronchogenic cysts, 2 | 2 managed conservatively with good outcome |
| Sequestration, 6 (2 intralobar, 4 extralobar) | 2 intralobar: managed surgically with excellent outcome. 4 extralobar: managed conservatively with good outcome |
The Course of 21 patients with Congenital Lung Malformations
5. Discussion
CLM is a relatively rare disease, caused by incomplete development of lungs. Most patients present pulmonary symptoms such as recurrent pulmonary infections and respiratory distress. However, patients with small lesions may remain asymptomatic. Therefore, in this research we presented the information of only 21 cases after 8 years of consecutive study of CLM cases in a referral pulmonary and thoracic surgery center.
Pathophysiological effects of CLMs on the fetus and mother could be detected by prenatal ultrasound (2). Development of hydrops (skin edema, pleural effusion, ascites, and pericardial effusion) is usually associated with poor fetal outcome (3). However, in our study, we did not have any case of hydrops requiring emergent surgery. Apparently, hydrops is a rare manifestation of CLM. A fetus with hydrops will be at an increased risk of fetal or neonatal demise, if fetal lobectomy or other proper interventions are not performed. In this regard, Harrison and Adzick suggested removal of lesions through hysterectomy or thoracotomy with trivial adverse effect of premature contractions and labor (4).
Vena caval, oesophageal and cardiac compression could induce fetal hydrops that manifests itself with ascites, pleural and pericardial effusions, and skin and scalp edema. Besides, fetal hydrops causes placentomegaly and resulted endothelial injury due to poorly perfused mega-placental tissue, releasing vasoactive factors. Although angiography was performed in many of our cases, no patient with Vena cava compression and hydrops was detected.
Three of our patients had expanding congenital intrathoracic lesions that ended in pulmonary hypoplasia due to compression of the developing lung. The hypoplastic lung was inadequate for normal gas exchange owing to an insufficient number of airway and vascular branches and vaso-muscular hypertrophy. This incident could induce pulmonary hypertension with persistent fetal circulation (4). Unfortunately, one of our patients with hypoplastic lung developed pulmonary hypertension in our workups and died of cardiac complication.
None of the patients had large mass at the time of diagnosis; thus, none of them developed cardiac deviation, hydrops, polyhydramnios or secondary pulmonary hypoplasia. Generally, there was no clear or superior prognostic factor in the patients other than size and type of the mass that called for prenatal counseling. Literally, progression or regression of mass, cardiac deviation, hydrops, polyhydramnios, pulmonary hypoplasia, and associated anomalies depends on the size of the mass. Altogether, large, bilateral and microcystic lesions tended to have poorer prognosis (4), which was compatible with our findings. On top of that, natural progression of these lung masses varies tremendously. Based on ultrasound imaging, congenital malformations could progress in size and develop hydrops, remain stable throughout pregnancy, or decrease in size and eventually disappear. Timing of regression is variable, but invariably tends to be in the mid-third trimester, usually between 32 to 34 weeks of gestation (4). We only had one patient with a mid-third trimester ultrasound finding of 2 cm mass, which regressed up until birth with no major complication other than lung hypoplasia. It is important to note that the treatment in the antenatal period aims to prevent fetal demise and irreversible lung injury. Treatment of polyhydramnios requires repetitive amniocentesis, indomethacin therapy, and video-endoscopic or ultrasonoguided placement of a thoracoamniotic shunt (3). Therefore, it was a wise decision to follow-up our patient with this mass, without performing a procedure during pregnancy until she was born.
Seven of 21 patients had CLM, but without hydrops. They survived well using planned delivery and immediate neonatal resuscitation. This seemingly-difficult fetal surgery has a reasonable chance of spontaneous regression. Therefore, fetal surgery is currently reserved only for those fetuses complicated with hydrops and an indisputable poor outcome (4). Fortunately, we managed our patients well without performing surgery.
Three of patients had lesions detected on prenatal ultrasound that resolved completely in the course of gestation. Notably, resolution of the ultrasound images in uterus may not necessarily imply the complete resolution of the primary pathology. On the other hand, normal radiographic findings do not preclude persistent findings of CT scan. Hence, all infants with an antenatal diagnosis of congenital lung malformations will require postnatal imaging to evaluate the lesions, even if they have apparently disappeared during pregnancy or if they are asymptomatic (4). In this regard, we performed post-natal evaluation on chest radiographs and CT scans in these three patients.
As mentioned in the results section, two cases underwent surgery with excellent outcome. As a matter of fact, surgical intervention is reserved only for patients with postpartum or postnatal respiratory distress. Nevertheless, symptomatic patients with respiratory distress underwent surgical resection. Neonatal pulmonary surgery is considered safe and unaltered, with no other life-threatening problems (4).
None of our patients were asymptomatic. Management of asymptomatic patients is controversial. Some authors consider close observation, whereas others recommend elective resection in every case because of the risks of recurrent infection, malignant transformation, pneumothorax, or sudden cyst enlargement. Early surgery could minimize further related morbidity and parental anxiety. Besides, alveolar multiplication continues in the first years of life, while compensatory lung growth after resection could be instigated in infants, but not in adults.
Two of our patients with congenital cystic adenomatoid malformation and bronchogenic cysts and intralobar sequestration were managed surgically while the rest were managed conservatively. Frequently in cases with bronchogenic cysts and intralobar sequestration, multiple abscesses develop in the resected lobes due to recurrent respiratory infections. In the meantime, early diagnosis and segmental resection could hinder the formation of abscesses and adhesions in these patients. Therefore, risks of pulmonary compression, infection and malignant degeneration, make surgical exploration imperative, even in asymptomatic patients (4).
We did not detect any genetic predisposition or positive family history in our patients. In some reports, involvement of one lung may still remain asymptomatic until older ages, when diagnosed incidentally (5). Although the exact etiology of CLM is unknown, genetic factors, viral infections and vitamin A deficiency during pregnancy could play a role in CLM progression (5, 6). Routine prenatal ultrasounds may help in early diagnosis of CLM after birth; however, differentiation of various subgroups of CLM requires other procedures such as neonatal CT scan and prenatal MRI. Controversy still exists regarding the perfect time and type of treatment. Our patients had a wide range of clinical manifestations; thus, we had to use concurrent lung CT to rule out other differential diagnoses such as foreign body aspiration, pneumonia, and end bronchial tuberculosis. Altogether, early diagnosis of the disease is of paramount importance in preventing complications and recurrent pulmonary infections. In our study, patients treated surgically showed significant improvement. Our result in this respect was in accord with Pikwer et al. outcomes, reporting surgery as the treatment of choice for such cases (7). Based on our study, surgery is considered a particularly safe procedure with the lowest morbidity and no mortality.
Antenatal diagnosed lesions should be monitored closely, because some need emergent surgery. Postnatal workup is extremely important, even in lesions detected to undergo regression in prenatal ultrasound. Considering the wide range of clinical manifestations from none to severe respiratory distress at birth, clinicians should consider the simultaneous use of chest X-ray, CT scan with contrast and MRI, for early diagnosis of the disease. Early diagnosis associates with more favorable treatment options, lower mortality and morbidity, and better prognosis. All of our patients were diagnosed postnatally because of their symptoms, turning surgery to the treatment of choice.