1. Introduction
In 1882 Müller H described a bronchial adenoma after autopsy (1, 2). Bronchial adenoma is a neoplasm that arises from the mucus gland of the bronchi or the cells lining the excretory ducts of these glands (3). There is a 40% incidence of malignancy (3). Lymph node metastasis is more frequent (15%) than distant blood-borne metastasis (3). Bronchial adenoma is the least frequent primary tumor of the lung which occurs five times more common in males and with the greatest incidence in adult age (2-4). Incidence rate of primary lung tumors is in a wide range between 0.6% to 6.9% (4-6). This tumor is usually undiagnosed especially in children due to the clinical presentation similar to pneumonia or asthma (recurrent respiratory symptoms), and usually patients are diagnosed several years after the onset of symptoms which may worsen the prognosis (7). Only 15% of the patients are asyptomatic. Tumors may be originated in the trachea, main bronchus or in the lobes of bronchi, although the right main bronchus is more commonly involved (3). There are two types of MEC according to the degree of malignancy.
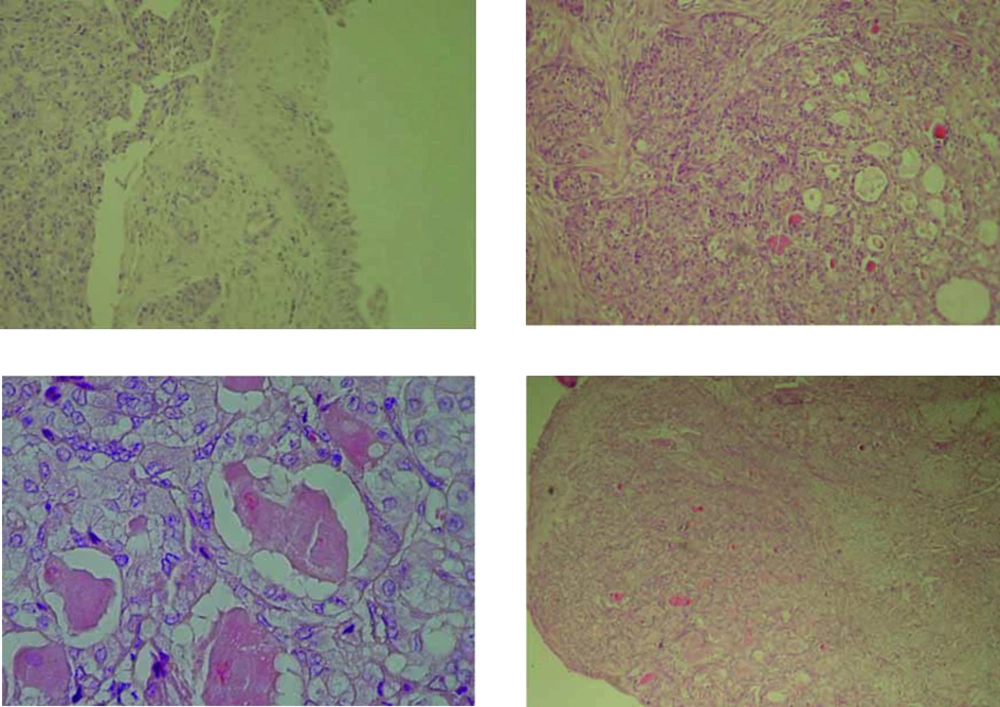
1) Low grade: Well-delineated endobronchial polypiod tumor covered with a thin mucosa macroscopically. In microscopic view, heterogenicity with dominant glandular base and mocoid content could be seen. This type of MEC presents with benign forms and there has only been one child in the international literature who has presented malignant form of the disease.
2) High grade: Infiltrating in macroscopic view. Microscopic findings show predominancy of epidermoid elements with atypia, hyperchromatism and high mitotic activity in these tissues. In the pediatric age, only two cases have been reported with this type of MEC.
Early bronchoscopy for patients with unilatral wheeze, repeated chest infections, non-productive cough, and haemoptysis is recommended (8, 9). Most bronchial adenomas are diagnosed with a combination of chest radiography, CT scan and bronchoscopy. Primary resection of a segment, lobe, or total lung, according to the degree of involvement is recommended. This may be done thoracoscopically or via thoracotomy, depending on the location and extent of the lesion (3). In this article we report a 4-year-old boy with bronchial adenoma who presented chronic cough and was diagnosed through Trans Bronchial Biopsy (T.B.B).
2. Case Presentation
The patient was a four-year-old boy, referring to our hospital with chronic cough, wheezing and dyspnea since 2 months before that. His cough and wheezing had gradually intensified during those two months. Physical examination findings were as below:
The left lung sound was decreased in auscultation. He didn’t have fever or any symptom of respiratory infection. There were no other significant findings in signs and symptoms.
Laboratory findings included a white blood cell count of 8900/mm3 with 56% of polymorphonuclear cell and 42% lymphocyte, red blood cell count 4160000/mm3, hemoglobin 10.3 g/dl and PLT 720000 and one-hour sedimentation rate (ESR) was 74 mm/hour. CRP was negative. Tuberculin skin test (TST) was done for him which was negative.
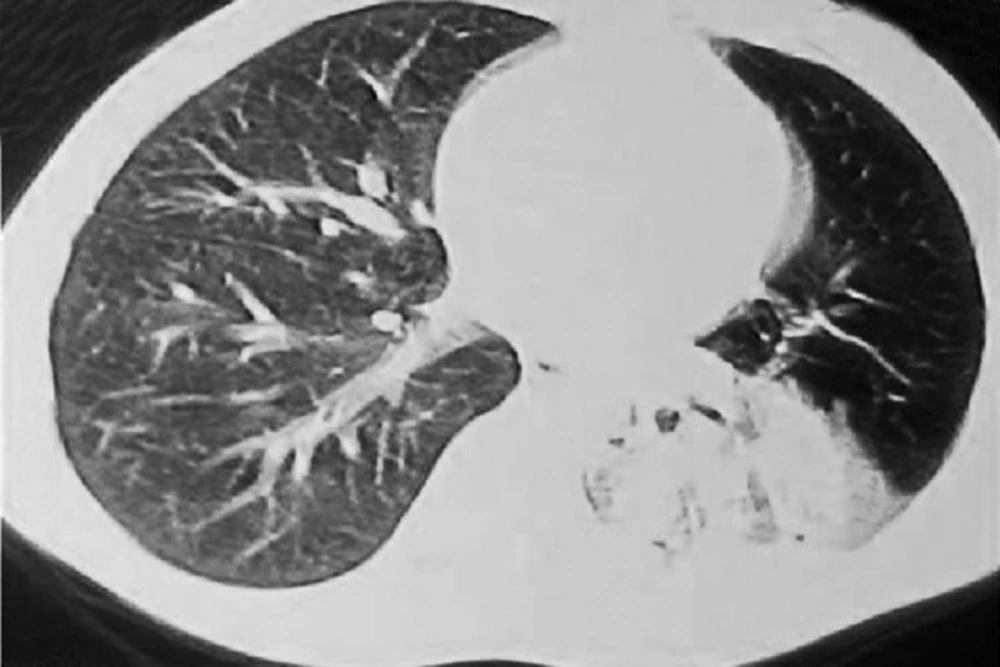
Chest radiography showed consolidation in left lower lobe (Figure 1). Chest computerized tomography (CT) scan detected peripheral bronchus dilation and left lung was found to be radio opaque diffusely (Figure 2). According to the clinical and radiological signs, with suspicion of foreign body aspiration, bronchoscopy was performed and foreign body was not detected but the cough still continued. After a month chest CT scan was repeated and this time it showed pulmonary consolidation in superior segment of the left lower lobe in lateral and basal segments (Figure 3). After these findings the patient referred to our hospital, for further evaluation.
Based on previous findings in our center, rigid bronchoscopy was performed which showed creamy colored mass with smooth surface at left lower lobe so T.B.B (Trans Bronchial Biopsy) was done for him. After T.B.B histopathological examination of the biopsy, it demonstrated low grade Mucoepidermoid carcinoma (Figure 4). Patient underwent left lower lobectomy with safe margin. In follow-up visits during two years his general conditions grew better and no specific sign and symptom detected.
3. Conclusions
In children, primary lung tumors are rare (10). Mucoepidermoid tumors of the lung are the rarest variants of bronchial adenomas, being slightly more common in female patients (11, 12). These lesions are believed to arise from the excretory ducts of the submucosal bronchial glands, and are located in the main stem bronchus or proximal portion of a lobar bronchus (11, 13, 14). Symptoms, when present, are due to partial or complete airway obstruction and include cough, wheezing, and dyspnea. Chest radiographs may show nodular masses, areas of lung consolidation, and partial or complete atelectasis (15). Because no characteristic features distinguish these tumors from bronchogenic carcinoma and other benign lesions, bronchoscopy and biopsy are especially helpful in establishing the diagnosis (14, 16). Mucoepidermoid carcinoma of the lung (formally called bronchial adenoma) consists 5% to 10% of these tumors (17, 18). This tumor is a common salivary type of primary tumors in lung after adenoid cystic carcinoma (19). Genetic study demonstrated that reciprocal chromosomal translocations including t (1;11) (p22;q13), t (11;19) (q14-21; p12), and t (11; 19) (q21;p13) are associated with these tumors. Chromosome 11 in the first translocation appears to be altered resulting in up-regulation of the cyclin D1 gene and over expression of cyclin D1. The t (11;19) (q21;p13) encodes a novel fusion product, capable of disrupting the Notch signaling pathway (20).
A review of the literature indicates that 54 cases of bronchial MEC in children have been reported. Most common age is middle age and distribution in male and female is equal (21). Common locations of these tumors are endobronchial, lobar, segmental and subsegmantal bronchus. A tumor histopathologically is divided into two groups: Low grade and high grade. Low-grade tumors are mostly endobronchial (12) low grade MECs are noninvasive but metastasis in lymph node has been reported (10). Most common symptoms in these patients are cough, Dyspnea, wheezing, pneumonia, and hemoptysis. Though fever, chest pain, fatigue, weight loss and chills also might be seen (19). Radiological findings usually are lobar infiltration, Atelectasis and Bronchiectasis (10). Common differential diagnoses are recurrent pneumonia, asthma and foreign body aspiration. Patients are often misdiagnosed and receive empirical antibiotics besides bronchodilator for treatment of pneumonia and asthma (21). Our patient had history of recurrent lower respiratory tract infection with suggestion of foreign body aspiration. In a study by Kim et al. (22), among 12 cases, the prevalence of atelectasis was 33%. Our patient had chest radiograph demonstrating atelectasis in left lower lobe, and rigid bronchoscopy was performed to detect foreign body aspiration. Complete treatment was performed by surgery and lobectomy. Surgical excision is the treatment of choice. These tumors may relapse locally, but complete resectable tumors have excellent prognosis.
In conclusion, in case of recurrent pneumonia and persistent respiratory symptoms with persisted lung infiltration in children, rare primary tumors of lung including MEC should be considered as one of the differential diagnoses and imaging is needed. In the patients with lung atelectasis which does not improve with conservative treatments, bronchoscopy and endoscopic biopsy seems necessary to confirm the diagnosis.