Dear Editor,
We are writing this letter regarding the importance of Pseudomonas aeruginosa (P. aeruginosa) colonization in patients with Cystic Fibrosis (CF) lung disease and the significance of new therapeutic approaches, including the development of different innovative aerosol formulations. P. aeruginosa is the main cause of chronic airway infection in this complex inherited disease, as confirmed by an interesting study of one of your articles published in this journal (1). This bacterium is also difficult to eradicate (since the chronic infection is established) and the development of resistance to the antibiotic treatment is also frequent. In the same article, Khalilzadeh et al. reported that P. aeruginosa had the highest susceptibility to ciprofloxacin, followed by amikacin, ceftazidime and ceftriaxone (1). Interestingly, our research group already has some results regarding this antimicrobial agent. We are working on the development of innovative formulations, such as microspheres intended to the treatment of P. aeruginosa infection in CF patients. These microspheres are obtained by the spray drying method and prepared with polymers (e.g. chitosan) at different concentrations and loaded with antimicrobial agents such as ciprofloxacin. The polymeric formulations allow the controlled release of the drug and may improve the patients’ compliance by reducing the number of administrations per day. The work is currently under way to optimize the characteristics of these microparticles in order to allow their pulmonary administration. In addition, an experimental design has been used to optimize the size on the basis of some formulation and operational variables.
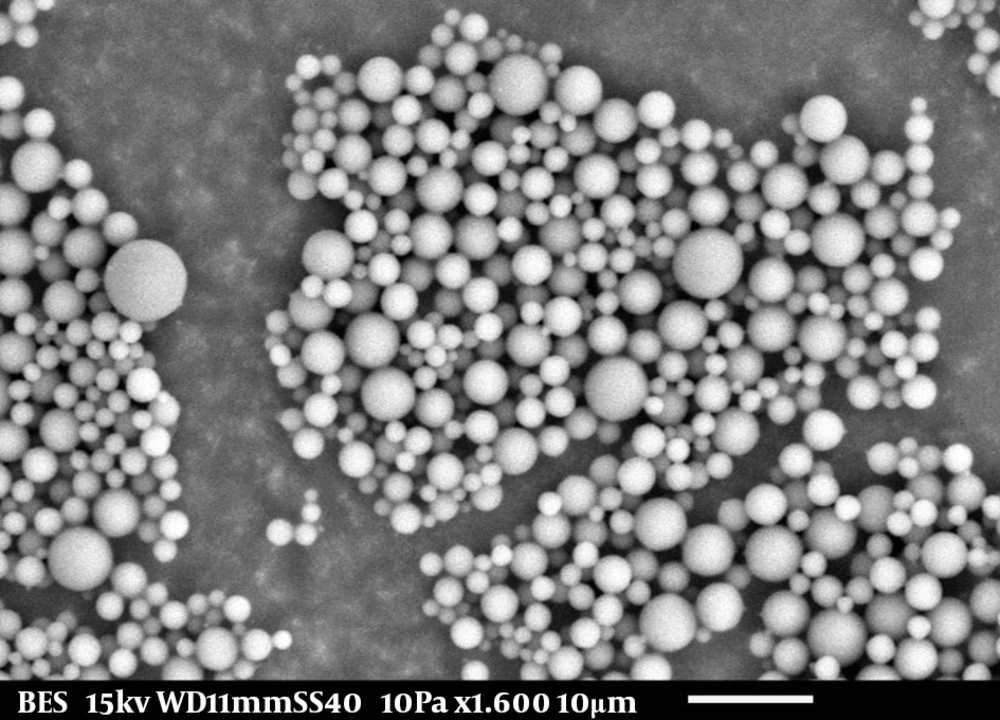
As previously reported by some authors, the particles administered to the airways have to present some specific properties. One of the most important characteristic is the size of these particles which should be comprised between 1 µm and 5 µm (2). In our research, particle size was determined by laser diffractometry and the results were confirmed with optical, fluorescence and scanning electron microscopy (SEM), which provided additional insight on agglomerate formation and morphology. The obtained size was within the optimal interval for pulmonary administration, with higher diameters for higher polymer concentrations. Regarding morphology, the microspheres were spherical with smooth surfaces (Figure 1). We have also confirmed the ability of these particles to incorporate drugs such as ciprofloxacin and levofloxacin. Regarding levofloxacin, a Phase 2b trial of Levofloxacin (inhaled) formulation demonstrated reduction of P. aeruginosa in sputum and improvements in lung function and the Phase 3 trial is complete (3).
In our research work, drug content was evaluated by UV/VIS spectrophotometry and the formulations presented encapsulation efficiency values between 42% and 91%. These innovative formulations may represent a new therapeutic approach for CF patients because they may target specific regions of the respiratory tract as well as reducing the systemic toxicity and the frequency of drug administration. Possessing the appropriate physical properties, they facilitate the dispersion of therapeutic agents in the inhaled air, reduce the deposition in the oropharynx and may modulate the release kinetics.
In addition, we would like to take this opportunity to report the importance of the nebulised antibiotic therapy. Some studies reported that using inhaled drugs for prophylaxis may decrease some complications in these patients (1, 4). In our recent published review, we reported some data about the use of anti-pseudomonal inhaled antibiotics in the eradication of early and chronic infection, to treat acute exacerbations or for prophylaxis. We also mentioned other formulations such as dry-powder formulations and liposomes that are under clinical trials or already available for the patients and also present some interesting advantages (5).
Finally, we would like to point out that “innovative treatment of CF lung disease” is an important issue under investigation, aiming the improvement of the quality of life and life expectancy of these patients.