1. Introduction
Headache is one of the most common neurologic complaints of children. Headache syndromes can be classified as; acute, subacute, or chronic (1-4). The vast majority of children complaining of headaches have chronic symptoms for months or years. The most common cause of chronic headache syndromes is migraine (1, 2). However, when a diagnosis is uncertain, there are many other possible etiologies besides migraine and primary headaches that need to be considered (5). The overall prevalence of non-migraine headaches is 10%-25%. A comprehensive history taking, physical and neurological examination, and appropriate diagnostic testing if indicated, will enable the physician to distinguish migraine and tension headaches, from those of secondary etiology (6).
2. Case Presentation
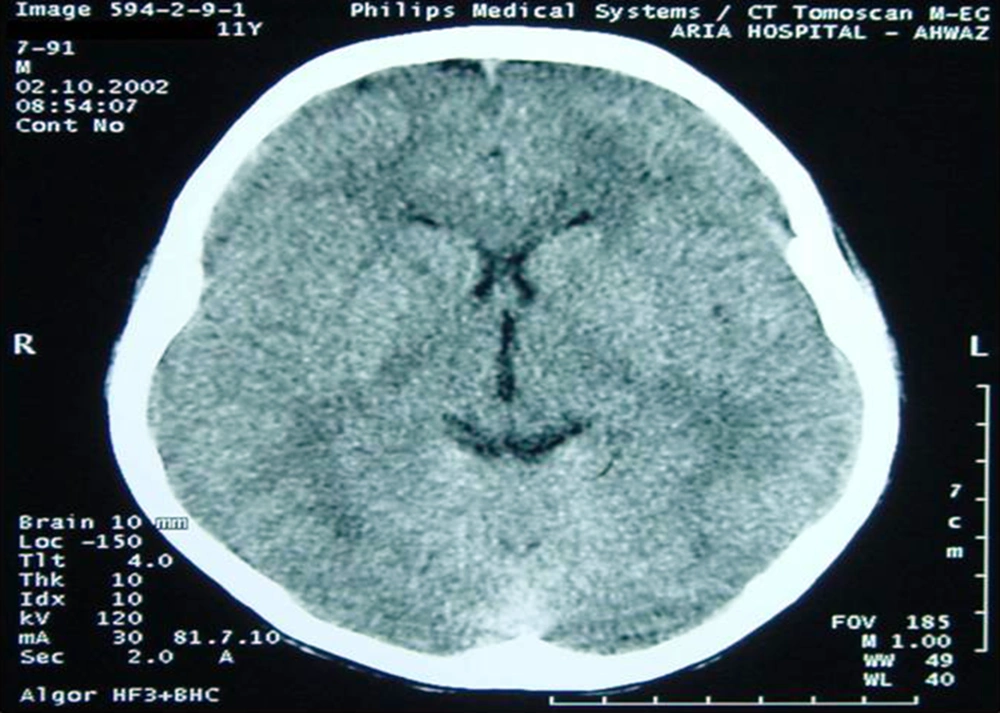
A 12-year-old boy was admitted with a history of headache and vomiting. He had experienced headache for at least four months. He described his headache as; continuous, non-pounding, felt in the frontal and retro-orbital areas, pain which was worst in the mornings, and it showed no response to over the counter analgesics. On occasion, he experienced nausea and vomiting in the morning. He had no symptoms of fever, vertigo, ataxia or limb weakness. He had also lost about 5-6 kg in weight. His behavior had not changed and he had not experienced any major changes in his environment. There was a history of migraine headache in his mother, and his father was on the staff of the city's veterinary organization. On admission, a physical examination revealed an ill-appearing boy, but in no acute distress. His temperature was 37.2°C, blood pressure 110/70 mmHg, pulse rate 96 beats per minute, and respirations 20 per minute. The remainder of his physical examination was normal. A detailed neurologic examination of the boy was completely normal. His investigations showed; Hb: 13.5 gr/dL, WBC: 4 900 (N: 60%, L: 30%), negative Widal test, normal electroencephalogram (EEG), and normal brain CT scan (Figure 1). However, a retention cyst was found in the sphenoid sinus of the paranasal sinuses CT scan (Figure 2). On otolaryngologic consultation he was diagnosed with sinusitis, and the child was treated with cefixime, prednisolone and nasal beclomethasone, but he showed no signs of improvement. On further investigation, a positive Wright test of 1/320 and 2-mercaptoethanol (2ME) of 1/160 were found. After a diagnosis of brucellosis, he was treated with gentamicin and doxycycline, furthermore, his headache diminished after 10 days of this treatment. After three weeks of treatment, drug reactions in the form of photosensitivity and skin rashes appeared and his medications were changed to oral trimetoprim-sulfamethoxazole and rifampin. By the completion of treatment the boy had no headache, and in a follow-up CT scan of the paranasal sinuses, the retention cyst in the sphenoid sinus had disappeared (Figure 3).
3. Discussion
Headache is one of the most common neurologic complaints of children (1-4). The most frequent cause of chronic headache syndromes is migraine; other causes of this syndrome are tension headaches, sinus headaches, ocular headaches, temporomandibular joint disease, epilepsy, trauma, and other inflammatory or infectious diseases (1, 2, 5). Our patient had a chronic daily headache, and although there was a history of migraine in his mother, the patient described his headache as continuous, with no pounding, it also had no response to migraine medications, and these symptoms did not correlate with a migraine diagnosis, therefore, further investigations were conducted. Other important diagnoses for chronic daily headache are increased intracranial pressure and tumors (1-3), but these were ruled out by neuroimaging. A CT scan revealed a retention cyst in the child’s sphenoid sinus. Only a very small percentage of mucoceles occur in the sphenoid sinus, and imaging plays a key role in the diagnosis of sphenoid mucoceles in patients who present with headaches. CT and MRI imaging showed rounded or partially rounded expansion of the sinus. Headaches occur in 15% of patients with chronic sinusitis and usually there is no fever. The most common accompanying symptoms are; rhinorrhea, post-nasal discharge, cough, sneezing, wheezing, and headache (7). Although our patient had no typical complaints of sinusitis, but based on the presence of a retention cyst in the sphenoid sinus (mucocele), sphenoid sinusitis was an appropriate diagnosis for the patient. As no improvement was achieved after conventional treatment of sinusitis for common pathogens, the patient was hospitalized for further evaluation. On evaluation, a positive serology of brucellosis; Wright test titer of 1/320, and 2ME of 1/160, were found. Based on the titer of 2ME the boy was diagnosed with acute brucellosis. Brucellosis is a zoonotic disease. Although the patient denied consumption of unpasteurized dairy products and meats, his father was on the staff of the city's veterinary organization. In a classic presentation of brucellosis, there is a triad of fever, arthralgia/arthritis, and hepatosplenomegaly. However, brucellosis can involve any organ of the body and may have a range of different presentations. Brucellosis can involve the central nervous system (CNS) in less than 2% of cases, but neurobrucellosis usually has other signs and symptoms of CNS involvement, and we found no case reports with headache as the only presentation (8, 9). Although it would be a rare manifestation, we think that if there is any relationship between brucellosis and headache in our patient, sphenoid sinus involvement is the most likely explanation.
In the literature review we only found one case with similarities to ours, this was the case of a researcher working with strains of brucella isolated from marine mammals. He suffered from continuous headache, lassitude and severe sinusitis. His blood analysis for brucella antibodies gave positive rising titers and specific cultures, in addition, a PCR, performed on his blood, showed marine mammal subtypes of brucellosis. His symptoms were permanently resolved after treatment with rifampin and doxycycline (10). Positive results for brucellosis, presentation with headache and sinus involvement, and the resolution of findings with brucellosis treatment in both of these cases is worth noting. As specific culturing and brucellosis subtyping were not performed in our case, the possibility of atypical subtypes of brucellosis (like marine mammal strains) also being the cause of this unusual presentation in our case remain unknown, nevertheless, the work of our patient’s father in a veterinary organization raises the probability. In order to establish the link between brucellosis and sinusitis, further investigation would be needed.
Although migraine is the first diagnosis in any child with a chronic daily headache, if it does not respond to treatment, further evaluation for other possible etiologies is required. In our case there seems to be a relationship between chronic headache, paranasal sinus involvement, and brucellosis. To establish this causality more firmly, further investigation would be needed.