1. Background
Children with T1DM and their mothers are at increased risk of depressive symptoms; moreover, maternal depression may contribute to the development of depressive symptoms in children by creating a stressful family environment (1).
Japanese mothers who had newly diagnosed diabetic children responded with shock, defensive retreat and increased anxiety. During this process, the degree of their isolation was shown as trauma. Although many mothers had a strong reaction and had depression, weight loss, pain and feeling of exhaustion, they adapted to the diagnosis at the end of the first year (2).
Parents of children with T1DM may experience a grief reaction at diagnosis similar to that normally associated with bereavement; however, little is known concerning their long-term emotional adaptation. Chronic sorrow, a sustained but intermittent grief reaction is identified in adults with diabetes but has not been previously explored in relation to parents (3).
Children with diabetes are at the risk of psychological disorders, also evidence supports that mothers of children with T1DM experience psychological distress. These parents reported stress associated with the responsibility required to manage T1DM on a daily basis and fears of hypoglycemia. One of the only longitudinal studies of depressive symptoms in mothers of children with T1DM found that after a period of initial adjustment, mothers seem to experience an increase in depressive symptoms and overall psychological distress with durational of illness (4).
Depending on the specific cancer, children are treated with a combination of radiotherapy, chemotherapy and surgery. However, treatments are complex and aggressive potentially compromising quality of life for children and their parents; moreover, a previous study showed increased anxiety and depression in parents after diagnosis (5).
Despite improved survival statistics, cancer remains a potentially life threatening condition and poses a major challenge to both child and family. During the course of treatment, most children experience unpleasant physical side effects. Behavioral and emotional problems have also been identified. There is a considerable risk of late effects. These include reduced linear growth, compromised endocrine and sensory functions and damages to cardiac and reproductive systems. In addition to the effects on children, adverse consequences for parents as well as immediate and long-term physical and mental health effects have been reported (6).
Many parents report elevated levels of depression and anxiety, especially in the months immediately after diagnosis; however, for most parents, this decreases over time. Mothers experience great changes in their lives because of staying in hospital with their children, perhaps giving up or reducing the hours they spend at work as well as learning how to manage the child’s medical care at home (7).
2. Objectives
Although parental psychological health, especially mothers as a main child health provider, has a major role in child treatment and follow-up, there are a few studies on evaluation of psychological health among them. We did not find similar study in Iran. Therefore, we conducted this study to compare psychological health in parents of children with chronic disease to assess the prevalence of psychological disorders according to type of childhood disease. We selected T1DM and Leukemia as two common and chronic diseases in childhood.
3. Patients and Methods
Psychological sequels were examined in 130 Leukemic children, children with diabetes and control and their parents group. The major dependent variables were symptoms of anxiety and posttraumatic stress, family functioning and social support.
This study was conducted as a cross-sectional analytical study. The study population was mothers whose children were referred to endocrinologic and hematologic clinics or emergency department of Hazrat Aliasghar children’s Hospital, affiliated to Iran University of Medical Sciences and Health Services. In two groups (case groups), children had a diagnosis of type I diabetes mellitus (group 1 or T1DM) or different types of leukemia (group 2 or Leukemic). As a control group, mothers of children referred to emergency department of the hospital with diagnosis of non-chronic diseases (including metabolic or malignant ones), mainly diagnosed as common cold, influenza or similar infections and gastroenteritis were studied. In each group, sampling was performed using a simple non-random (available samples) method using a consecutive sample. Time frame of the study was midsummer to early autumn (August to October, 2011). In each group, 30 mothers were studied.
Demographic and medical variables included:
1. Mothers’ age.
2. Mothers’ education: high school diploma or lower education and university education.
3. Mothers’ marital status: married and others (including single mothers, separated, divorced and widows).
4. Mothers’ employment: employed and unemployed.
5. Family outcome: Low, middle and high income.
6. Number of children in the family.
7. Age of indicated child and age of onset of disease (in T1DM and Leukemic groups).
8. Health insurance: covered and not covered.
9. Mothers’ history of previous known psychiatric disorders in Axis I or treatment with psychiatric medications.
We used Symptom Checklist-90-Revised (SCL-90-R) in the three groups of mothers as an instrument for screening mental disorders. Symptom Checklist-90-Revised is one the most widely studied measures in adult inpatient and outpatient psychiatric and non-psychiatric populations and its reliability and validity were proven in many studies. This checklist consisted of 90 items, using a 5-point Likert scale. The SCL-90-R is a paper-and-pencil instrument, completed in 12 - 15 minutes. The SCL-90-R measures psychiatric conditions in 9 subscales, including somatization (SOM), obsessive-compulsive (O-C), interpersonal sensitivity (I-S), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR), and psychoticism (PSY). It contains subscales as additional items as well. Reliability of subscales was reported between 0.80 and 0.97 in test-retest evaluations. Nasr et al. (2004) standardized the instrument in Iran (8). We used raw scores to compare psychological status of mothers.
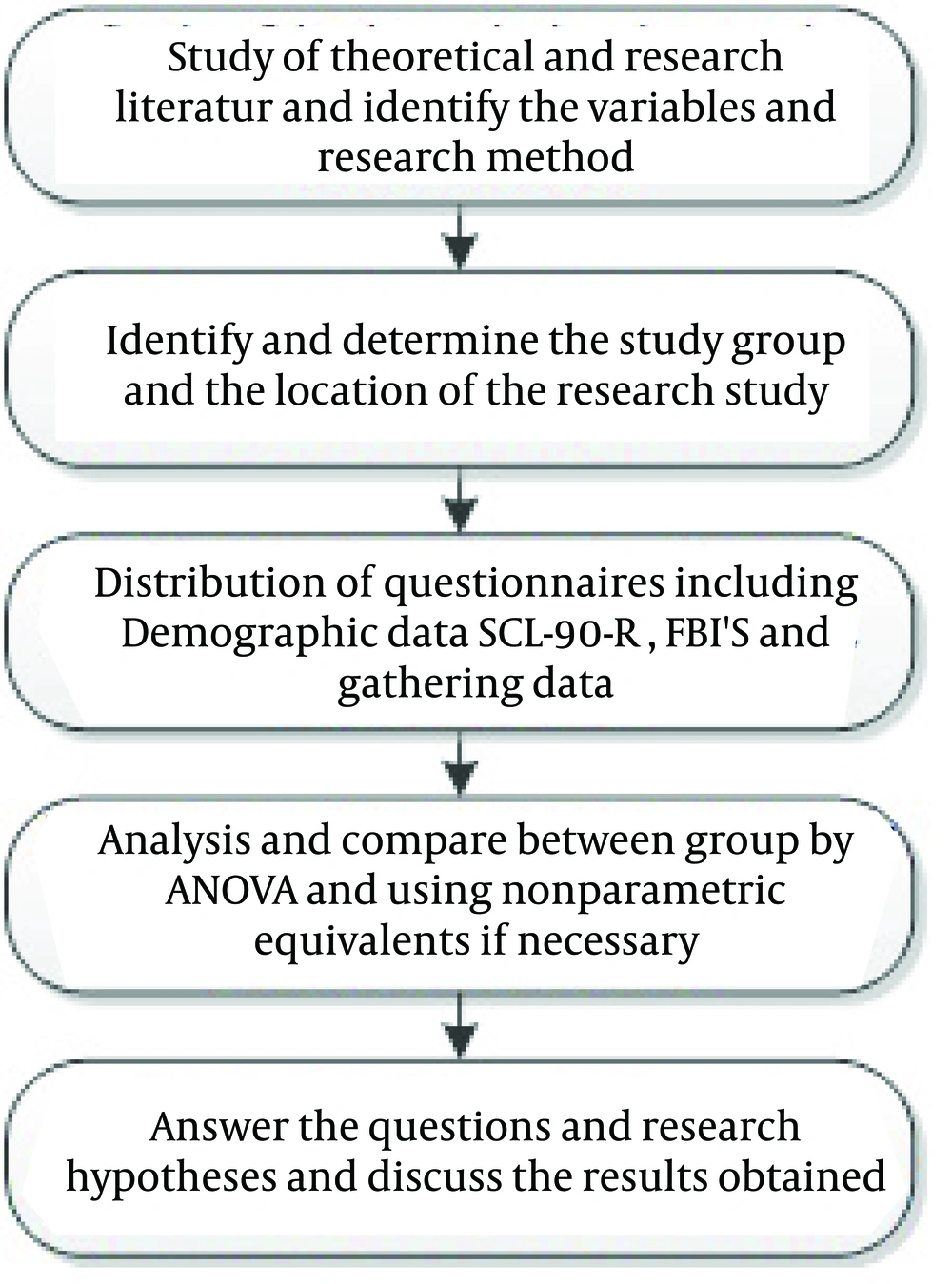
The second questionnaire used in the present study was the Family Experience Interview Schedule (FEIS), developed by Tessler and Gamache (9), as a revision of Family Burden Interview Schedule (FBIS) to evaluate the effectiveness of several important aspects of mental health services from a family member perspective (10). A short form of the questionnaire, consisting 41 items using Likert scale, developed and evaluated in a group of caretakers of patients with schizophrenia in Iran (11). The short form of the questionnaire consists of 8 domains; benefits and gratification, financial expenditure, assistance in daily living, supervision impact daily routines, affective response, feeling about patient and stigma. They showed that test-retest reliability of the short-form FEIS was 0.89 within a week and Cronbach’s α was 0.89 (11). Figure 1 shows the flowchart of the study.
Informed consent was obtained from all participants. Statistical analysis was performed using SPSS 19. To compare demographic variables between the groups, we used chi square/Fisher’s exact tests for categorical data and Kruskal-Wallis/Mann-Whitney tests for ordinal and ratio data. We used non-parametrical test due to non-homogeneity of variances and/or skewed distributions of data. In all cases of dimensional data, we used non-parametric tests as a result of different variances among groups. Type I error (α) was set at 0.05 and P < 0.05 considered as statistically significant difference.
4. Results
In each group, 30 mothers were studied (Table 1). Mothers in control group were younger, higher educated and more employed. Family outcome in control group was higher than the other groups. There were fewer children in control group and indicated children were younger than the others.
Psychiatric history of mothers; one mother in leukemic group and two in the control group had a history of previous depressive disorders. Only one mother in control group regularly used psychotropic medication.
The SCL-90-R: Median Global Severity Index (GSI) was 0.84 in T1DM group (ranged 0.12-1.79), 1.20 in leukemic group (ranged 0.00-3.52) and 0.33 in control group (ranged 0.00-2.03). The GSI showed statistically significant differences between the three groups (P < 0.001). The GSI was higher in leukemic group compared to T1DM group (Mann-Whitney U test: Z = 2.692; P = 0.007) and control group (P < 0.001). In addition, mothers in control group had lower GSI compared to T1DM group (P = 0.001).
Comparison of raw scores of the groups indicated statistically significant differences in subscales of SCL-90-R (Table 2). In all subscales, the raw scores were higher in leukemic group and lower in control group. However, the raw scores of depression showed no significant difference between T1DM and leukemic groups. In addition, phobic anxiety raw scores were similar in T1DM and control groups.
In a linear stepwise regression method, the associations of GSI in the SCL-90-R with child’s disease, mother’s age, mother’s education, family outcome, employed mother, mother’s marital status, single indicated child and child’s age were investigated (Table 3). Standardized regression (β) coefficient was 0.346 for T1DM group and 1.114 for leukemia group. In addition, higher educated mothers had higher GSI (standardized β = 0.266).
Family Experience Interview Schedule (FEIS); this questionnaire was completed by mothers in T1DM and leukemia groups (Table 4). The total scores were higher in T1DM group compared to leukemia group in three domains of supervision, feeling about patient and stigma.
| Variables | T1DM | Leukemic | Control | Statistical Difference |
|---|---|---|---|---|
| Mother’s age, y b | 33.5 (24-53) | 33.5 (25-48) | 32 (26-40) | K-W: χ2= 4.131; P = 0.127 |
| University education c | 8 (26.7) | 3 (10.0) | 15 (50.0) | χ2 test: χ2 = 11.791; P = 0.003 |
| Married mothers c | 29 (96.7) | 29 (96.7) | 29 (96.7) | |
| Employed mothers c | 3 (10.0) | 12 (40.0) | χ2 test: χ2 = 18.720; P < 0.001 | |
| Higher family income c | 6 (20.0) | 6 (20.0) | 15 (50.0) | χ2 test: χ2 = 8.571; P = 0.014 |
| Number of children b | 2 (1-3) | 2 (1-6) | 1 (1-3) | K-W: χ2 = 9.656; P = 0.008 |
| Child’s age at present, y b | 7 (1-15) | 5 (1-16) | 3 (1-10) | K-W: χ2 = 18.070; P < 0.001 |
| Child’s age at diagnosis, y b | 4.5 (1-14) | 4 (1-15) | M-W: Z = 0.617; P = 0.537 | |
| Insurance coverage c | 30 (100) | 30 (100) | 30 (100) |
a Abbreviations: K-W: Kruskal- Wallis test, M-W: Mann-Whitney U test, T1DM: type 1 diabetes Mellitus, χ2: Chi square test.
b Data are presented as median (range).
c Data are presented as No. (%).
| Variables | T1DM (D) b | Leukemia (L) b | Control (C) b | Kruskal - Wallis and Mann - Whitney U Test c |
|---|---|---|---|---|
| Somatization | 1.05 (0.10-2.20) | 1.29 (0.00-4.00) | 0.25 (0.00-1.83) | L > I > C |
| Obsessive compulsive | 1.05 (0.10-2.20) | 1.45 (0-4.00) | 0.60 (0-2.20) | L > I > C |
| Interpersonal sensitivity | 0.83 (0.11-1.89) | 1.17 (0-3.67) | 0.33 (0-2.67) | L > I > C |
| Depression | 1.38 (0.38-3.08) | 1.88 (0-3.85) | 0.65 (0-2.31) | L > (I = C) |
| Anxiety | 0.55 (0-1.60) | 1.10 (0-3.60) | 0.10 (0-1.80) | L > I > C |
| Hostility | 0.58 (0-2.17) | 1.17 (0-3.33) | 0.33 (0-1.50) | L > I > C |
| Phobic anxiety | 0.14 (0-0.86) | 0.43 (0-3.71) | 0.14 (0-1.00) | (L = I) > C |
| Paranoid ideation | 1.25 (0-2.33) | 1.17 (0-3.50) | 0.75 (0-2.00) | L > I > C |
| Psychoticism | 0.50 (0-1.20) | 1.10 (0-2.50) | 0.20 (0-2.20) | L > I > C |
| Additional items | 0.57 (0-1.86) | 1.29 (0-3.14) | 0.21 (0-2.57) | L > I > C |
a Abbreviation: T1DM: type 1 diabetes Mellitus.
b Data are presented as median (range).
c P < 0.05 was considered as statistically different range in parenthesis.
| Variables | β Coefficient b | Standardized β Coefficient | T | P Value |
|---|---|---|---|---|
| Leukemia as Child’s Disease | ||||
| Leukemia = 1; others = 0 | 1.114 ± 0.159 | 0.776 | 7.202 | < 0.0001 |
| T1DM as Child’s Disease | ||||
| T1DM = 1; others = 0 | 0.518 ± 0.146 | 0.364 | 3.537 | 0.001 |
| Mother’s Education | ||||
| Higher educated = 1; others = 0 | 0.399 ± 0.144 | 0.266 | 2.775 | 0.007 |
a Abbreviation: T1DM: type 1 diabetes Mellitus.
b Data are presented as mean ± SD.
| Variables | T1DM | Leukemia | Mann - Whitney U Test |
|---|---|---|---|
| Benefits and gratification | 4 (4 - 9) | 4 (4 - 16) | P = 0.113 |
| Financial expenditure | 4 (2 - 7) | 5 (2 - 10) | P = 0.311 |
| Assistance in daily living | 17.5 (10 - 28) | 20.5 (8 - 28) | P = 0.303 |
| Supervision | 11 (9 - 12) | 9 (3 - 12) | P = 0.001 |
| Impact on daily routines | 10 (5 - 16) | 10.5 (4 - 16) | P = 0.789 |
| Affective response | 15 (7 - 30) | 12.5 (7 - 28) | P = 0.317 |
| Feeling about patient | 32 (21 - 40) | 26.5 (8 - 38) | P = 0.013 |
| Stigma | 26.5 (18 - 28) | 21.5 (14 - 28) | P < 0.001 |
a Abbreviation: T1DM: type 1 diabetes Mellitus.
5. Discussion
Our aim was to compare psychological health among T1DM children’s mothers, Leukemic children’s mothers and control group. The GSI score in Leukemic children’s mothers was higher than the two other groups. In comparison between the T1DM and control groups, T1DM group had higher score in all medical characteristics except phobic anxiety. Multivariate analysis of covariance indicated significantly more posttraumatic stress symptoms in mothers and fathers of childhood Leukemia survivors, but there was no difference between survivors and peers. There were no significant group differences for family functioning or social support, although they were associated with anxiety and posttraumatic stress outcomes. Current child age, age at diagnosis and months off treatment were not significantly correlated with the outcomes.
These findings indicate the long-term impact of childhood cancer treatment on parents. Lack of significant differences for survivors argues for further attention to the relevance of posttraumatic stress disorder for childhood cancer survivors. The clinical implications indicate that psychological interventions are needed during and after cancer treatment for parents (12).
We found no sufficient study on disease comparison; just in one study, there was a comparison between mothers with a child diagnosed with cancer and mothers of T1DM and epileptic children, in which quality of life of parents with a child with cancer was lower compared to other groups. This study reported that parental functioning and wellbeing are important aspects of a family adaptation to chronic pediatric conditions. The study investigated the effects of diagnosis (cancer, diabetes, epilepsy) and time since diagnosis on parental quality of life (PQL). Parents of a child with cancer consistently reported lower PQL compared with parents of a child with diabetes and epilepsy. A diagnosis of cancer, especially in young children has a strong negative effect on PQL (13). The aforementioned result was similar to our study.
We use group therapy as a preventing tool in working with families and to reduce the stress(14). In a study performed on Japanese mothers with T1DM children, mothers had shock, increased stress levels, depression, and exhaustion. In our study, mothers of T1DM children had depression and anxiety as well as the Japanese mothers showed coping with diagnosis after the first year (15).
In another study performed on mothers of children with leukemia, posttraumatic symptoms were reported. Age of child and the time passed from the diagnosis had no significant association with mother’s symptoms, and these results are introduced as a sequel of long-term treatment in Leukemic children (12). In the above study, we found that a Leukemic child’s mother had depression and anxiety, which would not change by passing time after disease diagnosis.
Most mothers with a child diagnosed with a chronic disease such as T1DM and Leukemia have symptoms such as anxiety and depression, which mostly begin after child’s chronic disease. All these mothers need psychological intervention to improve their lives and their children nursing quality, but children themselves are not affected as much as their parents.