1. Background
Viral infections are one of the most important causes of fever in children (1). Many children experience convulsion several times in their life due to various types of infections, especially viral infections. Febrile seizure is one of the most prevalent reasons for pediatric clinics referrals. The prevalence rate of febrile seizure has been 3% to 8% (2). The general population’s concept of this incident is that fever can cause convulsion in children. However, the convulsion happens right before the fever onset in one-third of febrile seizure cases. The risk of recurrence in children with a history of one attack is 20% to 30% (2). Some factors increase the risk of febrile seizure recurrence in children, including first convulsion occurring in very young ages, family history of febrile seizure, and the convulsion occurring with a relatively low body temperature.
prescribing anti-pyretic medications, which may prevent convulsion or recurrence during the febrile stage, is recommended although it has not been proven yet (3). Fever in children has always been a stressing agent for parents, which causes an even higher level of anxiety among parents whose children have a history of febrile seizure. Fever control in such children has two general targets: A) confrontation with parents’ stress and fear toward seizure recurrence; and B) decreasing the risk and trauma following prolonged seizures, even if negligible.
2. Objectives
This study was performed to compare the effects of acetaminophen and ibuprofen on controlling fever and preventing seizures in children with febrile seizure.
3. Patients and Methods
In this cross-sectional study, 72 children, aged 6 months to 4.5 years who were hospitalized in the Pediatric Ward of Shohada-e-Tajrish Hospital, were primarily included. The febrile seizure diagnosis was based on elimination of other convulsion factors in patients. Before discharging the patients, the parents were educated about the methods of fever control and applicable medications as well as their dosage and they were provided with an informational pamphlet, a practical schedule, and a data-recording sheet. Common adverse effects of acetaminophen and ibuprofen were described for the parents and they were asked to refer their children to the physician and stop using the drug if they observed any of the conditions.
In occurrence of fever (axillary temperature > 37.8℃), 36 children received acetaminophen (15 mg/kg) in the form of drop, syrup, or suppository; the other 36 children received ibuprofen syrup (10 mg/kg) every 6 hours. The patients were under control and monitor for six months.
After the drug prescription, the parents were asked to measure and record the children’s body temperatures at 0, 2, 4, 6, 12, and 24 hours after administration of the first dose. The parents were regularly contacted, at least once a month, to ask about any incidence of fever, its intensity, drug dosage, any seizure indication, and drugs adverse effects.
Inclusion criteria were as follows: children aged 6 months to 4.5 years old, being diagnosed with febrile seizure, and being hospitalized in the Pediatric Ward of Shohada-e-Tajrish Hospital.
Exclusion criteria were as follows: 1) unwillingness to participate in the study; 2) inability of parents in correctly measuring the body temperature; 3) being < 6 or > 60 months old; 4) history of allergy to the study drugs; 5) history of epileptics; 6) proved brain anomaly; 7) history of brain surgery; 8) history of recent head trauma; 9) anti-seizure drug use prior to the study; 10) detection of any other cause for seizure during hospitalization; 11) using two antipyretic drugs during the febrile disease; and 12) Developing drug adverse effects.
4. Results
A total of 72 patients were assessed in two categories of acetaminophen and ibuprofen. Of the 72 patients, 42 were female (58.3%) and 30 were male (41.7%), with 21 females and 15 males in each group. In total, 40 patients (55.6%) were younger than two years old and 32 (44.4%) were between two and 4.5 years old. patients in each age group were equally divided into two groups of acetaminophen and ibuprofen.
The mean of fever episodes of all the patients during the study period was 1.58 ± 0.5; 1.56 ± 0.4 for the acetaminophen and 1.6 ± 0.5 for the ibuprofen groups.
In the acetaminophen category, there was only one fever episode in 20 patients during the six-month control period; two in 12, and three in four patients. In the ibuprofen category, 18 patients experienced one fever episode during the six-month period; 15 had two and three had three episodes. In total, the 72 patients experienced 114 fever episodes during the six-month study period; some information related to these episodes were recorded and investigated.
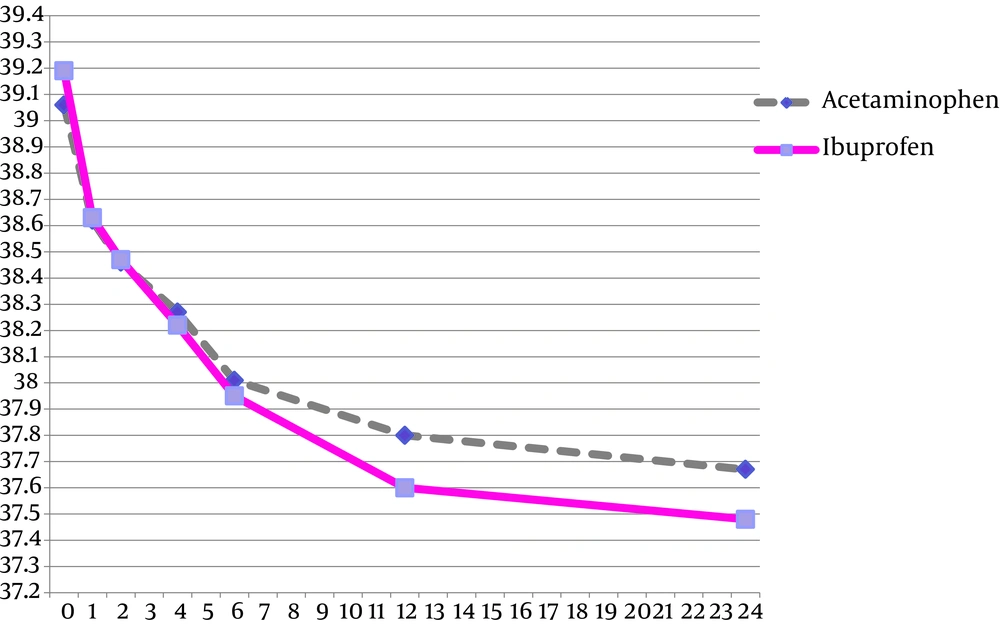
There was no significant difference in the mean of fever episodes between the acetaminophen and ibuprofen groups (P = 0.20). The means of body temperature at the beginning of antipyretic drugs administration were 39.06℃ ± 0.56℃ in the acetaminophen and 39.19℃ ± 0.61℃ in the ibuprofen groups (Figure 1). There was no statistically significant difference between the acetaminophen and ibuprofen groups in the patients’ mean body temperature (P = 0.335).
Table 1 shows the mean body temperatures in the patients at the beginning of antipyretic drug administration as well as at 1, 2, 4, 6, 12, and 24 hours of first dose administration.
Table 2 shows the mean of body temperature decrease in different time intervals after acetaminophen and ibuprofen consumption in two different age groups of < 2 and 2-4.5 years old.
There was no difference in body temperature decrease following administration of acetaminophen and ibuprofen at one, two, and four hours after the consumption (P = 0.055, P = 0.181, and P = 0.0167, respectively).
However, there was a significant difference in body temperature decrease in children of the two groups at 6, 12, and 24 hours of the drug consumption (P = 0.006, P = 0.005, and P = 0.0044, respectively).
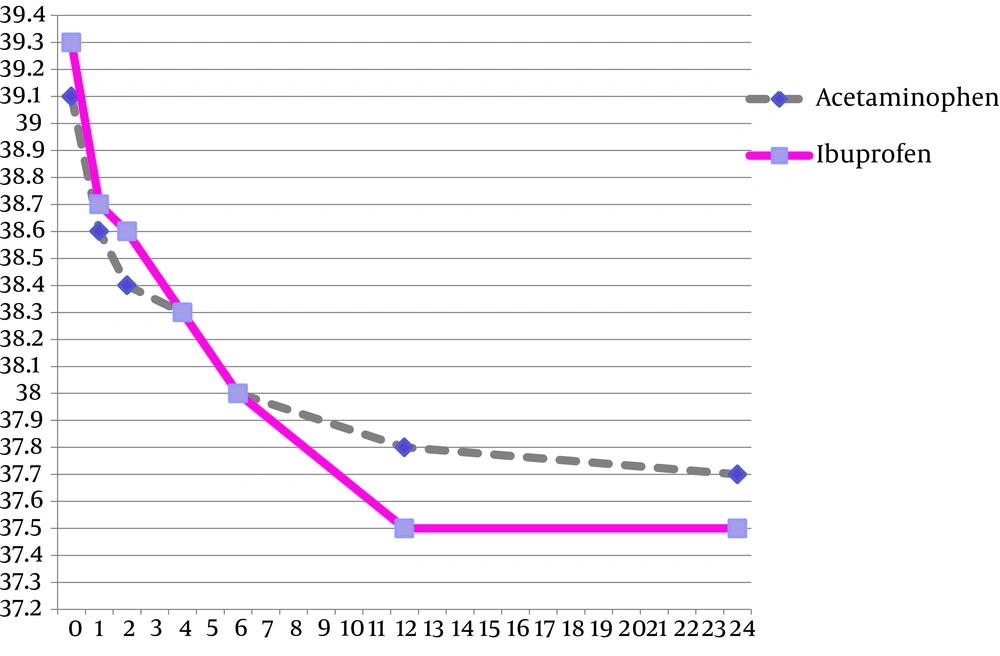
Regarding the children in the < 2-year-old group (Figure 2), there was no significant difference in the body temperature decrease following acetaminophen and ibuprofen consumption at one, two, four, and six hours of drug administration (P = 0.199, P = 0.108, P = 0.748, and P = 0.411, respectively). However, there was a significant difference in body temperature decrease between two groups at 12 and 24 hours of drug administration (P = 0.02 and P = 0.003, respectively).
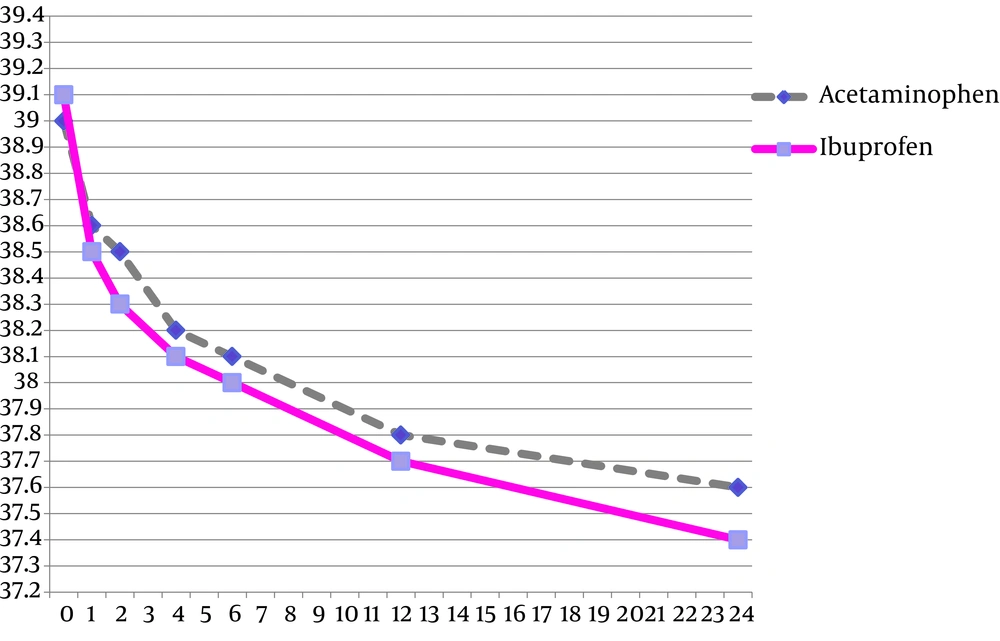
Regarding the children in the age group of 2-4.5 years (Figure 3), there was no significant difference in body temperature decrease after administration of acetaminophen and ibuprofen at one, two, four, six, 12, and 24 hours of drug consumption (P = 0.140, P = 0.330, P = 0.102, P = 0.307, P = 0.119, and P = 0.263, respectively).
In total, febrile seizure recurrence happened in seven patients (9.7%); five in the acetaminophen and two in the ibuprofen groups. There was no significant difference in seizure recurrence between the two groups of acetaminophen and ibuprofen (P = 0.233). From these seven patients, four were in the age group of < 2 years and three in the age group of 2-4.5 years.
There was no significant difference between the two age groups of < 2 and 2-4.5 years old regarding seizure recurrence (P = 0.929). in addition, there was no significant difference between the two groups of acetaminophen and ibuprofen in children < 2 and 2-4.5 years old regarding seizure recurrence (P = 0.605 and 1.000, respectively).
There was a significant difference in the mean of primary body temperature between the patients with and without seizure recurrence (P = 0.007); This difference between these two groups was significant up to 12 hours of the antipyretic drug administration, but there was no significant difference between the two groups 24 hours after the drug administration. No serious adverse effect was reported in any of the patients.
| Passed Time From Drug Administration, h | 0 | 1 | 2 | 4 | 6 | 12 | 24 |
|---|---|---|---|---|---|---|---|
| Acetaminophen | 39.06 ± 0.56 | 38.62 ± 0.45 | 38.46 ± 0.34 | 38.27 ± 0.36 | 38.01 ± 0.40 | 37.80 ± 0.29 | 37.67 ± 0.23 |
| Ibuprofen | 39.19 ± 0.61 | 38.63 ± 0.50 | 38.47 ± 0.43 | 38.22 ± 0.42 | 37.95 ± 0.41 | 37.60 ± 0.36 | 37.48 ± 0.30 |
Mean of Body Temperature in Participants a
| Elapsed Time From Drug Administration, h | 1 | 2 | 4 | 6 | 12 | 24 |
|---|---|---|---|---|---|---|
| Acetaminophen | ||||||
| < 2 y | 0.47 ± 0.33 | 0.66 ± 0.37 | 0.76 ± 0.36 | 1.11 ± 0.36 | 1.29 ± 0.40 | 1.39 ± 0.38 |
| 2-4.5 y | 0.56 ± 0.39 | 0.70 ± 0.41 | 0.98 ± 0.47 | 1.30 ± 0.52 | 1.74 ± 0.50 | 1.76 ± 0.55 |
| Ibuprofen | ||||||
| < 2 y | 0.41 ± 0.38 | 0.53 ± 0.42 | 0.83 ± 0.42 | 0.96 ± 0.38 | 1.23 ± 0.52 | 1.39 ± 0.51 |
| 2-4.5 y | 0.56 ± 0.33 | 0.76 ± 0.42 | 0.98 ± 0.36 | 1.18 ± 0.35 | 1.41 ± 0.51 | 1.66 ± 0.49 |
Mean of Fever Decrease Since Drug Administration a
| Age Group | Occurrence of Seizure at the Time of Study | Total | |
|---|---|---|---|
| Negative | Positive | ||
| < 2, y | |||
| Acetaminophen | 17 | 3 | 20 |
| Ibuprofen | 19 | 1 | 20 |
| 2 - 4.5, y | |||
| Acetaminophen | 14 | 2 | 16 |
| Ibuprofen | 15 | 1 | 16 |
| Total | 65 | 7 | 72 |
Seizure Recurrence in Patients According to Age and Treatment Groups
5. Discussion
In total, 72 patients were evaluated; 36 were in the ibuprofen and 36 in the acetaminophen groups. The mean of body temperature at the beginning of antipyretic drug administration was 39.60℃ ± 0.56℃ in the acetaminophen and 39.19℃ ± 0.61℃ in the ibuprofen groups. These amounts did not have any statistically significant differences between the two categories of acetaminophen and ibuprofen (P = 0.325).
In this study, the prevalence of seizure recurrence was approximately 10%. In reference books, this prevalence among children with febrile seizure has been reported to be 20% to 30% (2).
Seemingly, the most important reason for lower recurrence prevalence in our study was the short study period. Most probably, by following up the patients to the age of five, the prevalence of seizure recurrence would be higher. In our study, there was no difference in seizure recurrence between the two groups of acetaminophen and ibuprofen consumption. Similar results have been observed in other studies. In a study by Uhari et al. 180 patients were assessed after the first experience of febrile seizure in three groups:
A) Patients who received acetaminophen and placebo,
B) Patients who received diazepam and placebo,
C) Patients who received acetaminophen and diazepam.
They revealed that none of the mentioned treatments were effective on decreasing the probability of seizure recurrence (4).
Offringa et al. performed a meta-analysis on results of 26 clinical trials, including 2740 individuals, regarding the role of prophylactic treatments for febrile seizure, and revealed no significant difference between ibuprofen and acetaminophen (5).
In our study, the consumption of ibuprofen for controlling fever was more effective than was acetaminophen during the six to 24 hours of the administration of the first dose. Many other studies have come up with similar conclusions. In a meta-analysis (Medline, 1966 to November 2003; and Embase, 1988 to November 2003), ibuprofen was more effective than acetaminophen after six hours. In another meta-analysis in Medline/PubMed until 2009 and in Embase until 2008 on 85 studies regarding comparison of acetaminophen with ibuprofen usages, it has been revealed that ibuprofen was effective for pain and fever relief in both children and adults and the usage of both drugs was safe. It was also demonstrated that four hours after drug administration, the antipyretic effect of ibuprofen was stronger than that of acetaminophen (6). There was no significant difference between the adverse effects of acetaminophen and ibuprofen in the two studied groups (6). In other evaluations, the abovementioned results were confirmed (7, 8).
According to the mentioned results, the following concepts can be conceived:
First, antipyretic drugs administration does not have a very important role in preventing seizure occurrence in children. Second, most probably, ibuprofen is more effective than acetaminophen for fever control in patients, especially in younger children. Third, there was no significant adverse effect, both generally and regarding prevalence, in any of the antipyretic drugs (acetaminophen and ibuprofen) in different dosages. Nevertheless, more certainty could be achieved through performing studies with larger sample sizes.