1. Introduction
Liver abscess is an important cause of hospital admissions in tertiary care centers in India, but it is only seldom that we encounter them as a consequence of infection acquired during hospital stay. We reported a case of liver abscess developed during hospital stay while the child was on hemodialysis as a consequence of nosocomial bacteremia. This article highlights the importance of high index of suspicion, strict vigilance and infection control policies to prevent such nosocomial infections.
2. Case Presentation
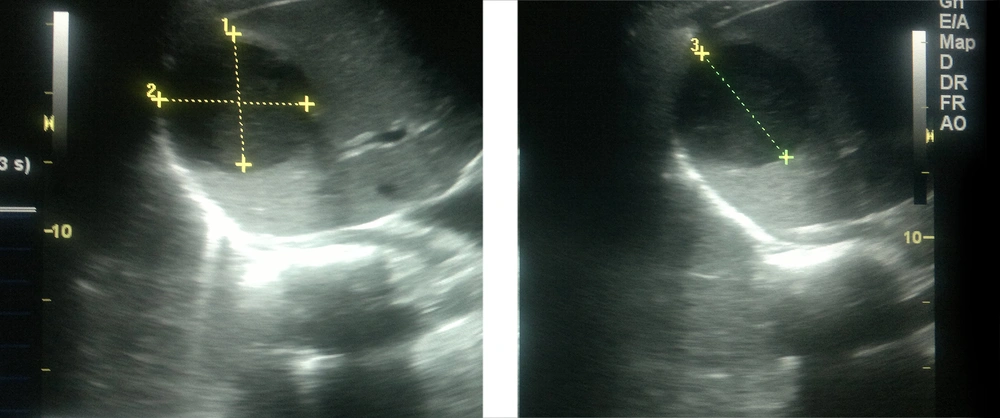
A 6-year-old boy presented with high grade fever for 12 days before being referred our hospital, vomiting (2 - 3/day) and abdominal pain (periumbilical area, dull aching) since two days ago. Treatment from a local practitioner (undocumented) had not brought any relief. There were no past complaints. On physical examination, weight was 22 kg (between 50th to 75th percentile for age), height was 112 cm (on 25th percentile for age), he was febrile (temperature of 101°F (38.3°C)); pulse rate was 100/minute, BP of 90/60 mmHg and respiratory rate of 26/minutes. There was generalized abdominal tenderness without guarding or rigidity, liver was not palpable, spleen was palpable 2 cm below the costal margin. Respiratory, cardiovascular and neurological system examinations had normal findings. Investigations on admission showed Hb 10 g/dL (hemoglobin), TLC-12000/cumm (total leucocyte count), DLC-N88L12 (differential leucocyte count), Blood urea 70 mg/dL, S. creatinine 0.77 mg/dL and normal levels of serum electrolytes. The patient received intravenous antibiotics and other supportive care. However, his sensorium worsened on the next day and was kept under close monitoring in intensive care area. He further developed multiorgan dysfunction syndrome (MODS). Repeat investigations showed polymorph nuclear leukocytosis with deranged coagulation profile, renal parameters and liver function tests (Hb-9 g/dL, TLC-17,000/cumm, DLC-P80L20, platelet-4 lakh/mm3, prothrombin time (PT) Test > 1 minute, activated partial thromboplastin time (APTT) > 1 minute, blood urea-110 mg/dL, S.creatinine-4 mg/dL, total bilirubin-5.3 mg/dL, direct bilirubin-3.1 mg/dL, SGOT-3255IU/L (serum glutamic oxaloacetic transaminase), SGPT-2539IU/L (serum glutamic-pyruvic transaminase), S. albumin-2.74 g/dL). Widal, peripheral smear for malarial parasite and rapid malarial antigen had negative results. Blood culture was negative. Chest X-ray had normal findings. Ultrasound abdomen showed mild ascites, normal liver size and echotexture. Cerebrospinal fluid analysis was also normal. Patient was managed as a case of sepsis with multiorgan dysfunction syndrome with encephalopathy most likely due to uremia. Antibiotics were upgraded to meropenem. He was given ventilatory support due to low score 6 on Glasgow Coma scale and blood products (fresh frozen plasma and packed red cells) for gastrointestinal bleeding. Stress induced hyperglycemia was managed with insulin. On day two of hospitalization, due to acute kidney injury, he underwent peritoneal dialysis and was given 110 cycles. His awareness improved and became afebrile by day five; however, he continued to have deranged renal parameters; therefore he was given five cycles of hemodialysis. Renal parameters improved gradually, but he had high grade fever on day 17, while on hemodialysis. Thorough examination and detailed investigation work up could not localize the cause of fever. An abdominal sonography (done again this time) detected an abscess in the right lobe of the liver measuring 40 cc as shown in Figure 1. Meropenem was continued and vancomycin was added, doses of which were modified according to the glomerular filtration rate (estimated glomerular filtration rate was 15 mL/minutes/l.73 m2 according to the Schwartz equation). He showed good symptomatic improvement obviating any need for aspiration. The liver abscess regressed completely and he was discharged on oral antibiotics to complete a six-week course and was symptom free on follow-up.
3. Discussion
Liver abscesses constitute more than 79 per 100000 pediatric admissions (< 12 years age) in tertiary care centers in India (1). Important predisposing factors are parasitic infections, malnutrition, skin infections, abdominal infections, trauma and genetic disorders causing immune deficiencies (1). Patients with renal disease on chronic hemodialysis are prone to infectious diseases and among them liver abscesses (2). Impaired immunity in these patients renders them susceptible to infectious processes and dialysis itself also impairs immunity (3).
Chuang et al. found that chronic hemodialysis patients who developed extra-renal abscesses were more frequently associated with lower serum albumin level and lower normalized protein catabolism rate compared to other hemodialysis patients and diabetes mellitus and poor nutrition status were important predisposing factors for the development of extra-renal abscesses in these patients, the most common site being the liver (2). Huang et al. found a high incidence of liver abscess among ESRD (End-Stage Renal Disease) dialysis patients, especially patients ≥ 65 years, with peritoneal dialysis and polycystic kidney disease as important risk factors in addition to the known risk factors (4). The reports of extra renal abscesses developing in patients on hemodialysis are all among adults (2-5). The only pediatric case of liver abscess developing in a patient on hemodialysis (chronic) was reported by Spencker et al. in a 14-year-old girl on hemodialysis for four years (6).
Among the pathogens involved in pyogenic liver abscesses in children, Staphylococcus aureus is the leading cause apart from anaerobes and Gram-negative rods (1). The causative organisms in most reports of abscesses developing during hemodialysis therapy have been Gram-negative bacilli (2, 3). Methicillin resistant Staphylococcus aureus has also been reported in a man who had 13 years history of frequent hospital visits for hemodialysis treatment (7). In Spencker’s case, Aeromonas hydrophila was isolated from the environment of the hemodialysis room (6).
Pyogenic abscesses can be single or multiple. The right hepatic lobe, as in this case, is more commonly involved than the left one (1, 7). Biliary system infection is generally associated with multiple lesions, whereas abscesses arising via the portal vein are usually solitary (1, 7).
Patients with ESRD who develop pyogenic liver abscess carry a poor prognosis and if left untreated is uniformly fatal (5). Small abscesses, which are diagnosed early may respond to antibiotic therapy alone as not requiring any drainage or aspiration procedures in our case. Drainage procedures when required are associated with complications like peritonitis (5), which may be difficult to manage in already immunocompromised patients.
In our case, liver abscess developed during the course of hospital stay while the patient was already receiving broad spectrum antibiotics. The patient deteriorated and developed fever while on hemodialysis, after initial improvement. Dialysis therapy for renal disease and hyperglycemia may have predisposed our patient to bacterial infections leading to liver abscess, but our patient was not on chronic hemodialysis therapy as seen in other case reports. Our patient may have acquired nosocomial bacteremia, the most likely route of infection being bloodstream infection acquired during hemodialysis with subsequent hepatic seeding. The limiting factor seems to be non-isolation of any pathogen. Quick response to vancomycin and also the small size of the abscess, obviated any need for direct aspiration. Blood culture was sterile probably due to ongoing antibiotic therapy. Staphylococcus is known to be an important cause of liver abscesses in children arising via the hematogenous route and good response to vancomycin suggested the same. This case report is unique as there is no similar report of a child developing nosocomial liver abscess after short-term dialysis therapy. Pyogenic liver abscess should be suspected in any patient on dialysis who develops fever.