1. Introduction
Tachycardia-induced cardiomyopathy (TIC), tachycardiomyopathy, is a type of dilated cardiomyopathy (DCM) caused by various atrial or ventricular arrhythmias. This cardiomyopathy improves partially or totally by rhythm and heart rate control; therefore, its early diagnosis is vital. The time of DCM following arrhythmia treatment varies based on the patient’s age. Improvement occurs in infants within few weeks, while it takes two/three years in older children. In fact, the longer duration of tachycardia, the longer duration of remodeling (1).
Atrial arrhythmias such as atrial flutter, atrial fibrillation, ectopic atrial tachycardia (EAT), intraatrial reentrant tachycardia, permanent junctional reciprocating tachycardia (PJRT) and arrhythmias with reentrant mechanisms such as atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT) are reported so far (2, 3). Also, ventricular arrhythmias such as persistent ventricular tachycardia or premature ventricular contraction are reported (4). The most frequent cause of TIC in children is orthodromic tachycardia, but atrial fibrillation or flutter and persistent ventricular tachycardia are more prevalent in the adults and the elderly. Clinical presentation in older children is left ventricular dysfunction, exercise intolerance, chest pain, syncope, perspiration, respiratory distress and recurrent palpitation (5). This condition should be considered while making the diagnosis, particularly when the patient presents with the first episode of congestive heart failure and echocardiography is suggestive of DCM.
In long QT syndrome (LQTS), clinical features include syncope and sudden death. This syndrome is due to dysfunction in Na and K channels in the myocardial cell wall. Three common types include LQTS1, LTQS2 and LTQS3 that develop due to mutation in KCNQ1, KCH2 and SCN5A, respectively. This syndrome also has an acquired type that develops following the use of certain drugs.
Authors herewith report a case of TIC with LQTS. Coincidence of LQTS and EAT is important since it can result in sudden death. However, the current case always had recurrent intermittent tachyarrhythmia but did not have syncope or LQTS symptoms.
2. Case Presentation
The patient was a conscious 12-year-old boy with obesity (height = 153 cm, weight = 63 kg, BMI = 26.9) who presented palpitation since the previous day. In physical examination, symmetric but weak pulses were felt in the extremities. The patient had pallor, tachycardia and tachypnea, with a blood pressure of 80/50 mmHg. A 2/6 holosystolic murmur was discovered in the cardiac apex with clear gallop rhythm. Lung sounds were normal and liver and spleen were within normal size ranges.
His parents admitted that he had several episodes of palpitation in the past three years and had received oral beta-blocker with no significant effect. The patient also complained of early exhaustion, exercise intolerance and sweating. In the chest X-ray, cardiomegaly and increase of parenchymal vessels was observed.
Electrocardiogram revealed regular tachycardia of 170 - 180 bpm with narrow QRS complexes and 1:1 atrioventricular relationship. The early diagnosis was supraventricular tachycardia and he was admitted in the cardiac care unit for further evaluation, monitoring and treatment.
Due to the absence of abnormal T wave in the electrocardiogram and normal serum levels of CK-MB and troponin, myocarditis was ruled out. Negative blood culture and normal serologic evaluations also ruled out infectious and inflammatory etiologies.
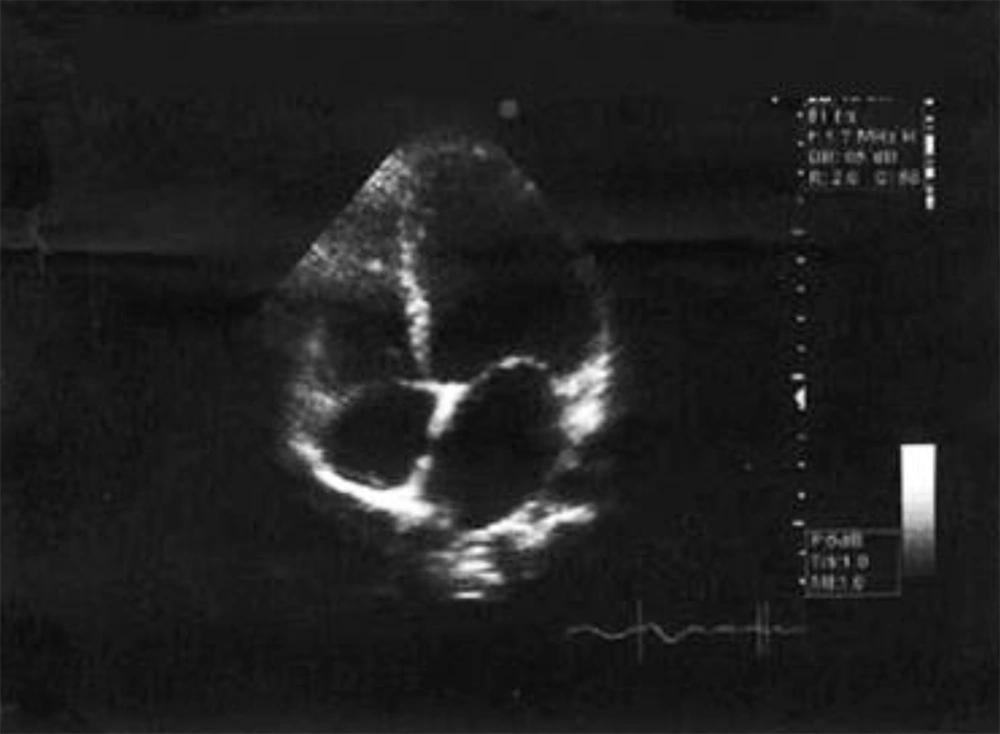
In echocardiography, ejection fraction was 30% with M-mode and 25% with the Simpson method. Other findings included left ventricular end-diastolic diameter = 58 (zv ≥ 3) and left ventricular end-systolic volume = 48 mm (zv ≥ 3), as well as the presence of mitral regurgitation. DCM was suggested as the probable diagnosis (Figure 1).
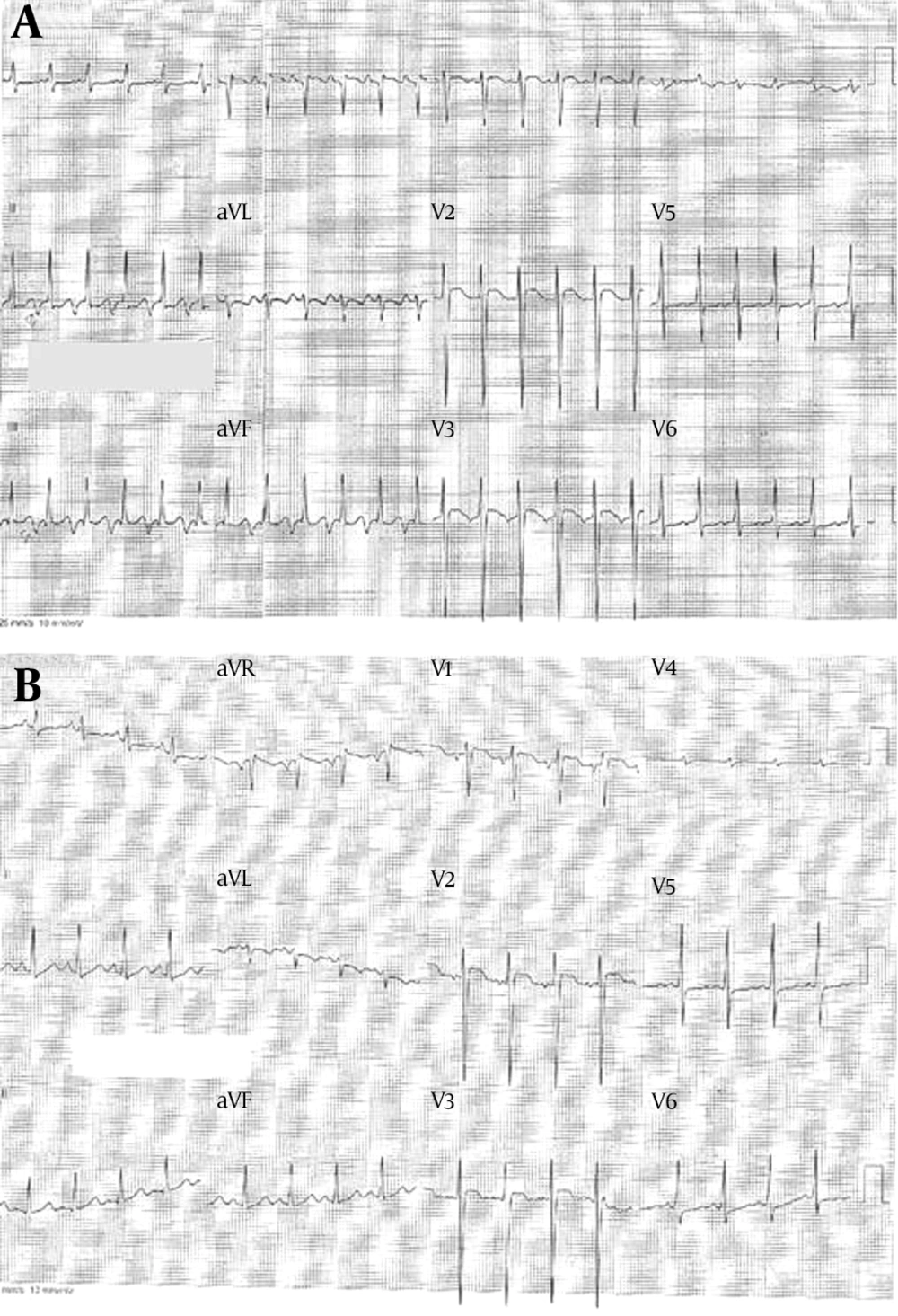
Based on the electrocardiogram, since the P wave was negative in the leads II, III and AVF, and long PR interval was present, PJRT was considered as the next diagnosis (Figure 2A).
To treat arrhythmia, adenosine was administered in three doses, which was not successful. Therefore, amiodarone was initiated that showed no therapeutic effect after 12 hours. Due to unresponsiveness to adenosine and amiodarone, the diagnosis of EAT from the perspective adjacent to coronary sinus or posteroinferior region of the right atrium was made.
The patient underwent electrophysiological study and ectopic foci were recognized near coronary sinus in the posterior wall of the right atrium (Tables 1 and 2).
| Results | |
|---|---|
| Induced-Arrhythmia | |
| Arrhythmia CL | 388 |
| AH interval | 124 |
| HV | 44 |
| LVA (HIS) | 224 |
| VA (HRA) | 32 |
| Ectopic Atrial Tachycardia | |
| Initiation mode 1 | A pace |
| Initiation mode 2 | |
| Initiation mode 3 | |
| Termination mode 1 | V pace |
| Termination mode 2 | |
aA Successful ablation of the AT origin was done in Cs ostium.
Abbreviations: CL, cycle length; LVA, left ventricular analysis; VA, ventricular activity.
| Results | |
|---|---|
| Cycle Length | 464 |
| PR Interval | 118 |
| QRS Duration | 90 |
| QT interval | 325 |
| AH interval | 78 |
| HV interval | 48 |
| Ventricular Stimulation | |
| VA WP | Diss |
| RERP of AV node | Diss |
| VA jump | |
| Ventricular ERP | 220 |
| Ventricular DCL | 450 |
| Atrial Stimulation | |
| AV WP | 260 |
| AERP of AV node | 240 |
| AERP of AV node | 220 |
| Atrial ERP | < 200 |
| Atrial DCL | 450 |
After radiofrequency catheter ablation (RFCA), heart rate decreased to 80 - 85 bpm (Figure 2B). Three days later, the patient was discharged in a good condition with a blood pressure of 110/75 mm Hg. In the echocardiographic evaluation at the time of discharge, his ejection fraction was 40%, and anti-congestion drugs were prescribed.
Within the follow-up period, it was noticed that QT interval in leads II and AVF was about 450-460 milliseconds. Therefore, genetic tests for LQTS were requested and the results revealed that the patient had LQTS gene type I.
Until the last follow-up visit that was 8 months after the initial presentation, the patient was under treatment with sotalol and had no arrhythmia. The latest ejection fraction was 62% and in Holter monitoring, in assessing cardiac arrhythmias, the mean heart rate was 97 bpm and reached 70 bpm while sleeping.
3. Discussion
To manage the children who complain of palpitation, the initial step following history taking and physical examination is electrocardiography. If the rhythm and heart rate are normal in the electrocardiogram, it is advised to request Holter monitoring for 24 - 48 hours in order to evaluate palpitation and tachycardia attacks. Performing an echocardiography, particularly in the presence of auscultation findings is necessary. The development time of the left ventricular dysfunction depends on the type and duration of tachycardia as well as the presence of any structural heart diseases (6).
Initial evaluation of the electrocardiogram in the current study patient showed negative P wave in leads II, III and AVF suggesting public health response team (PHRT) as the mechanism of tachycardia. In this rare tachycardia, persistence and continuation of tachycardia results in cardiomyopathy in the affected children (7). It has an orthodromic mechanism in which conduction occurs via the accessory pathway and an antegrade connection occurs via the AV node. Accessory pathway is mostly at the anterior orifice of the coronary sinus. In this tachycardia, heart rate is about 300 bpm in neonates and 150 bpm in asymptomatic children. P wave is closed to its next QRS complex and in fact the RP interval is long in one cycle; therefore, it is a tachycardia with prolonged RP interval. This finding was also present in the electrocardiogram of the current study patient, but it did not stop or decrease following three times of adenosine administration.
One of the tachycardias with normal and regular QRS complexes and 1:1 AV relationship is EAT. Development and continuation of this arrhythmia does not depend on AV node; therefore, it does not stop spontaneously or following adenosine administration. This arrhythmia manifests as TIC in children. Finding the medical history is usually a non-specific compliant such as malaise, lethargy, vomiting, and exercise intolerance (8). Due to insidious nature of the condition and small changes in the heart rate, sometimes the patient may not feel the palpitation. Therefore, high clinical suspicion and evaluation of several electrocardiograms are crucial for the diagnosis. In this tachycardia, heart rate is usually above normal limits, even during resting time. Moreover, drastic changes in the heart rate occur during exercise. Changes of heart rate are small and monotonous heart rate is seen in long term recordings. Although EAT is persistent, it sometimes resolves during sleep and sinus rhythm appears.
The goal of treatment in TIC is to relieve the arrhythmia. Antiarrhythmic drugs class IA, IC and III as well as beta blockers are used to treat EAT. In unresponsive cases to medical treatment, electrophysiological study and radiofrequency catheter ablation are recommended (1). Following the treatment of arrhythmia, improvement of DCM occurs which its duration differs based on age (1). In the current case, the patient did not respond to medical treatment but successfully responded to electrophysiological study and catheter ablation.
Mutation of KCNQ1 gene was the major finding in the current study patient as he did not have any clinical or pharmacological predisposing factor for acquired long QT syndrome.
3.1. Conclusions
Overall, careful management of children with recurrent tachycardia is highly recommended. It is necessary to have the standard tables and percentile graphs of heart rate and blood pressure for children in every emergency department, hospital ward and office to better interpret the clinical evaluations in children. Findings of electrocardiogram in the first visit can help to establish the diagnosis, especially in the presence of changes in P wave, RP interval, delta wave and signs of ectopic atrial tachycardia. TIC has a good prognosis and cardiac function returns to normal level with proper treatment in case of early diagnosis. Therefore, this condition should be considered in the differential diagnoses of idiopathic DCM.