1. Introduction
Chronic abdominal pain is a common problem in children and adolescents. Although many causes are listed for it, nutcracker syndrome is not considered in this list. Nutcracker phenomenon (NCP) is a rare vascular variation which is caused by contraction of the left renal vein, usually between the superior mesenteric artery (SMA) and the aorta. The nutcracker syndrome (NCS) results in some symptoms that range from mild proteinuria or asymptomatic microscopic hematuria to severe symptoms duo to pelvic congestion (1) or nephrotic range proteinuria (2). Most patients become symptomatic in the second and third decades of their lives (3).
Here is the report on a case of an eight-year-old girl who presented chronic abdominal pain and microscopic hematuria and was diagnosed with NCS.
2. Case Presentation
An eight-year-old girl was referred to pediatric nephrology clinic of Mofid Pediatric hospital, Tehran, Iran, by gastroenterologist due to microscopic hematuria. She had been evaluated by gastroenterologist for chronic abdominal pain with one year duration. She had a previous history of urinary tract infection. The patient did not have the history of gross hematuria, renal stone, genitourinary tract trauma, chronic diseases and drug consumption in her medical history, but she had dysuria occasionally. Her father had a history of microscopic hematuria without known renal problems.
On physical examination, her weight was on the third percentile and her height was on the 25th percentile; others factors were unremarkable.
According to the laboratory urinalysis, gravity was 1015, pH 6.0, blood (++ +), leukocyte esterase (-), protein (+) and urine microscopy showed many red blood cells (RBCs) and 1 - 2 white blood cells (WBCs). Her urine culture was negative. Stool exam and antiendomysial antibodies were normal. Complete blood count (CBC), serum biochemistry, urine solute including calcium, oxalate and uric acid were in the normal range. Antinuclear antibody, C3, C4 and CH50 were also normal.
Abdominal ultrasound (US) showed fullness of the left pyelocalyceal system with anteroposterior diameter of 9 mm. Cystography and diethylenetriaminepentaacetic acid (DTPA) renal scan were normal.
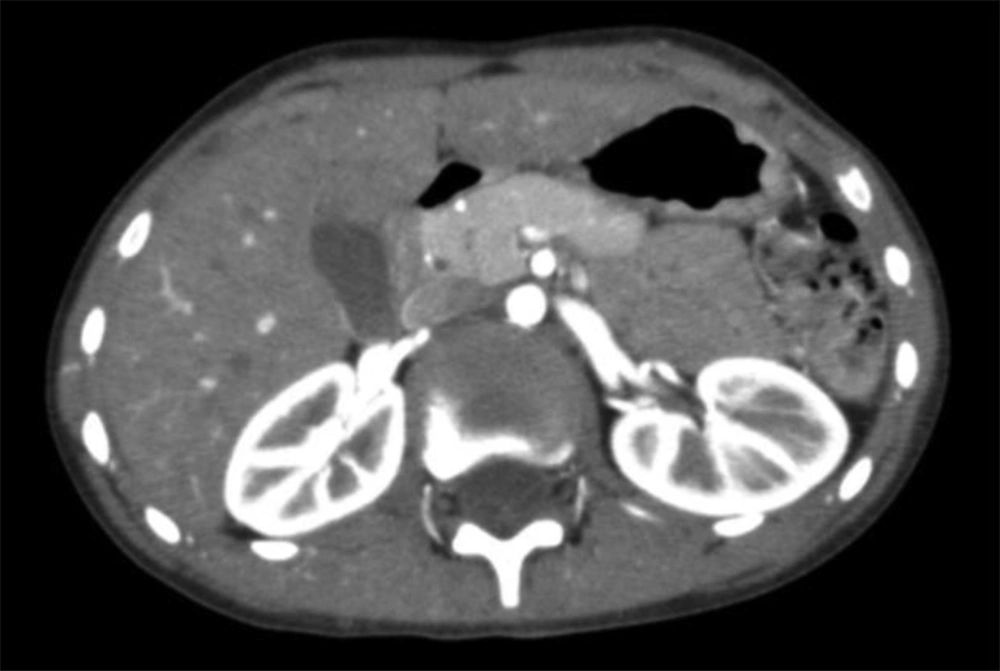
Computed tomography angiography (CTA) was performed to elucidate the other causes. There was abrupt diameter change in the left renal vein passing superior mesenteric artery and aorta (7 mm to less than 1 mm) suggestive for anterior nutcracker syndrome.
Whereas there were no severe symptoms such as relentless pain, gross hematuria or decreased renal function conservation treatment such as painkillers and weight gain were recommended.
3. Discussion
The left renal vein (LRV) entrapment between the SMA and aorta was first described by El Sadr and Mina in 1950 (4). de Schepper (5) referred to the disorder as nutcracker syndrome in 1972.
Nutcracker phenomenon (NCP) is not a hereditary phenomenon. NCP or renal vein entrapment is characterized by disrupted outflow from the LRV into the inferior vena cava (IVC) due to outside LRV compression. The nutcracker phenomenon is not always associated with clinical symptoms. The term nutcracker syndrome refers to patients with characteristic clinical symptoms such as hematuria, proteinuria, flank pain, abdominal pain and varicocele associated with demonstrable nutcracker morphologic features. LRV entrapment is divided into anterior and posterior types.
Anterior NCS is created by the entrapment of LRV between the abdominal aorta and the superior
mesenteric artery. Posterior NCS is the compression of LRV by abdominal aorta and vertebral column. Some acquired causes may play a role on the etiology of posterior NCS such as LRV duplication, paraaortic lymphadenopathy, retroperitoneal mass, aneurysm of abdominal aortic, overarching testicular artery and ventral replacement of right renal artery (6, 7). However, all of the anatomic mechanisms lead to renal vein contraction resulting in outflow blockage with a measurable renocaval pressure gradient. LRV hypertension leads to forming of varices and collaterals in the nearby renal calyces. Hematuria and proteinuria are the consequences of these venous sinuses.
The current study patient had significant microscopic hematuria. Hematuria, which is the most common presentation of this syndrome differs from microscopic to gross, depends on the severity of the LRV hypertension. It is primarily due to high LRV pressure end to the rupture of the thin-walled septum between the small veins and the collecting system in the renal fornix (8). An incidence rate about 33% among children with microscopic hematuria was reported in literature for nutcracker syndrome (9). The study patient was thin and her abdominal pain was exaggerated by physical activities. Regarding anatomy, when the body is upstanding, visceral proptosis diminishes the angle between the SMA and aorta, heightens the hemodynamic response especially if there is decreased retroperitoneal and mesenteric fat tissue (10).
Proteinuria with various degrees is another common symptom of NCS. NCS is established as an etiology of nephrotic syndrome or orthostatic proteinuria (2, 11, 12). Although the exact mechanism of orthostatic proteinuria is not defined, it could be due to the increased liberation of angiotensin II and norepinephrine induced by changes in renal hemodynamic upon standing and increased LRV pressure and mild subclinical immune damage (13).
Pelvic congestion resulting in abdominal pain, flank pain, back pain and varicocele is observed in patients with NCS (1, 14, 15). Collaterals formation could become a cause of pelvic congestion (3, 16). Pain is a consequence of flaring of the inflammatory cascade induced by venous hypertension (7). The current study patient had chronic abdominal pain for one year.
Tachycardia, hypotension and syncope are the symptoms of autonomic dysfunction presentation of NCS, but they are rare (17).
Doppler ultrasonography, CTA, magnetic resonance angiography (MRA) and retrograde venography could be applied for diagnosis. CTA is non-invasive and has an excellent diagnostic value, although has the detriment of radiation exposure. The normal LRV diameter is 4 - 5 mm (18).
In CTA, the left renal vein often shows a disparity in caliber between the part distal to the aorta and the part precisely in front of the aorta. Buschi et al. evaluated CT scan, ultrasonographic and pathologic data in a series of 72 patients, showing that the ratio of LRV diameters of the distended to the narrowed portions may reach 4:1 (19). This ratio in the current case was approximately 7:1 significantly more than upper normal limit (4:1).
The treatment decision ranges from surveillance to nephrectomy (13, 20). Mild symptoms can be followed conservatively. However surgical treatment is suggested for recurrent gross hematuria accompanied by anemia, relentless flank or abdominal pain, renal insufficiency and inefficacy or aggravation of symptoms despite a quiet treatment such as persistent orthostatic proteinuria after 24 months follow-up (21, 22). Transposition of the LRV or SMA, nephropexy, intravascular and extravascular stent implantation, gonadocaval bypass, renal autotransplantation and nephrectomy are surgical procedures (4, 20, 22).
The best option for patients younger than 18 is a conservative approach with at least 24 months follow-up without medications. Kurklinsky et al. showed that 75% of patients with hematuria completely treated during this period (23). Another suggested conservative therapy is weight gain. Alaygut et al. followed clinical course of 23 patients with NCS. They showed that at the end of an average of 16 - 22 months follow-up, body mass index (BMI) markedly increased (BMI at diagnosis 16.9 ± 4.0 kg/m2; at the end of the follow-up period 18.6 ± 4.6 kg/m2; P= 0.028) in patients with regressed hematuria and proteinuria (24). Angiotensin inhibitors also could be useful in patients with severe orthostatic proteinuria (7).
NCS is a rare entity with various symptoms such as hematuria, proteinuria, flank pain, abdominal pain, varicocele, fatigue and orthostatic intolerance. Insufficient knowledge of its clinical manifestations results in late diagnosis and attempting invasive procedure such as renal biopsy. Doppler sonography and CTA are the optimum choices of imaging modalities to diagnose NCS. In asymptomatic patients, especially those who are less than 18 years old, expectant treatment is the best option. Those with serious and persistent symptoms may benefit from a surgical or intravascular intervention.