1. Introduction
There are many causes of neck masses in children of which congenital anomalies are the most popular ones. These abnormalities include cervical bronchogenic cyst, remnants of the bronchial cleft or lymphatic malformation, thyroglossal duct, cystic teratoma, parathyroid and thyroid cysts and thymic anomalies. Due to its rarity, cervical thymic cyst is seldom included in the differential diagnosis of a neck mass, and it is rarely a symptomatic cervical thymus cyst (1). Thymus gland is mainly originated from the third and fourth pharyngeal pouches in association with the inferior parathyroid glands. Right and left portions of the thymic primordium descend down the neck during the sixth to eighth weeks of gestational life and fuse to form the gland (2). Finally, thymus gland reaches its destination in anterior mediastinum behind the sternum. Thymic gland anomalies in the neck are the consequences of an arrest in the descent of the gland, sequestration of the thymic tissue or failure of involution (3). In other words, these thymic cysts are more often found in mediastinal part but since thymus normal descent pathway is from the angle of the mandible to the superior mediastinum, these anomalies can be found at any level. Thymic cysts are infrequent causes of neck masses in children, which are not usually considered in the differential diagnosis. Physical examination and preoperative imaging correctly diagnoses thymic remnants in 15% patients (4). Although rare, malignant thymomas also may develop from an ectopic thymus, situated in the thyroid gland or in the neck (5). Sometimes ectopic thymic cyst is associated with parathyroid element in the neck mass (6). Because of many side effects like immunodeficiency after total thymectomy, it is important to be careful enough to avoid unnecessary thymectomy in infants and children, so preoperative diagnosis of the lesion with confirmation of normal mediastinal thymus is essential (7). Except visible mass in the neck, most of the patients are asymptomatic (8). The purpose of this study is to present the experience, as well as to review current data on the embryology, clinical presentation, diagnosis and management of thymic cysts in childhood. Moreover the most cases have been described as asymptomatic and of little clinical consequence. The following case presenting with respiratory signs, made it worthy for reporting.
2. Case Presentation
A 5-year-old boy was referred to our clinic for evaluation of a left sided cervical mass. The mass had initially appeared about 4 months ago and its growth was accelerated in the last month without inflammation. Two weeks ago, the patient had been admitted in local hospital due to respiratory distress following a common cold. He was referred to our clinic because of incomplete recovery after intravenous antibiotic therapy. There was no history of change in voice or difficulty in swallowing, pain, dyspnea, cough or fever. His past medical history, drug history and family history were unremarkable.
On physical examination, he was conscious and cooperative with mild tachypnea. His weight and height were in normal range. The auxiliary temperature was 37.2 ºC, blood pressure and pulse rate were within normal range. Ophthalmologic and also ear, nose and throat examinations were normal but an ill defined mass was visible in the left side of the neck. It was soft, nontender, noncompressible, but moved with deglutition and was 5 ×5.5 cm in size on palpation. The swelling was located in medial to anterior border of sternocleidomastoid muscle extending from below of the mandible to the clavicle on the left side of the neck. It was cystic in consistency with no signs of inflammation. The trachea was deviated to the right side and an inspiratory stridor could be heard on auscultation. Auscultation of the heart had normal s1 and s2 with no murmur. There was no lymphadenopathy. The Chest and abdomen were normal on examination. Physical examination of other systems had no abnormal findings.
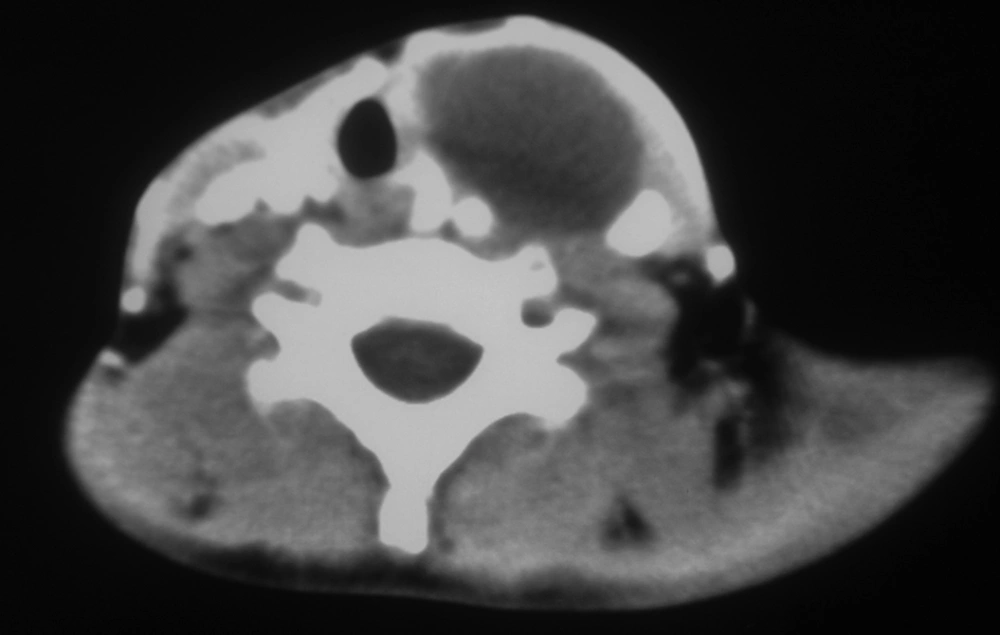
Patient's laboratory tests showed normal hemoglobin, white blood cells count and differentiation, erythrocyte sedimentation rate, C-reactive protein, prothrombine time (PT) and partial thromboplastin time (PTT). Also chest X-ray was almost normal. Ultrasound revealed a 6×6 cm cystic mass in the left side of the neck, beneath the sternocleidomastoid (SCM) muscle and anterior to the carotid artery. The mass was extended to the mediastinum and was compressing the trachea. CT scan with intravenous contrast showed a 6×5.5 cm cystic mass in the left neck (Figure 1) which was extended to the anterior mediastinum, suggesting cystic hygroma.
A decision was made to remove the mass surgically. The operation was performed with patient in supine position and his neck rotated to the right. The neck and chest were prepared and draped. Neck was explored; the incision was made along the anterior border of the sternocleidomastoid because of possible necessity to sternotomy in continuation of surgery. The cyst was located beneath the sternocleidomastoid and antro-medial to the carotid sheet with adherence to vascular structure. For protection of vessels, sharp technique was used to dissect the mass from carotid artery and internal jugular vein. Then the most cephalic portion of mass was dissected. As the mass was elongated toward the anterior mediastinum, partial sternotomy was made to fallow its extension (Figure 2). Evaluation showed that the mass was originated from the left lobe of the thymus. After complete dissection from brachiocephalic vessel, the cyst and its extension were completely removed. Mediastinum was drained with hemovac drain. The patient was transferred to intensive care unit with no complication or neurological injuries for 2 days and afterwards, was transferred to the surgery ward. The patient’s post-operative course was uneventful, his symptoms and signs disappeared and he was discharged on 4 th postoperative day. Histopathological examination of mass showed a cyst wall lined by flat to cuboidal lining. The wall was composed of fat and fibro-collagenous tissue, showing focal aggregation of lymphoid cells with Hassall’s corpuscles inside. Based on these classical findings, the diagnosis of ectopic thymic cyst of the cervical region was given. The patient was followed up for 12 months without any evidence of recurrence.
3. Discussion
Presence of solid thymic rests in the neck is not rare according to autopsies, but silent nature of such remnants conceals them throughout the life (9). Thymic cyst prevalence is less than 1% of all cervical masses, and they are usually noted in childhood (10). Most patients with thymic cysts complain of a slowly enlarging, asymptomatic cervical mass. Symptomatic cases of cervical thymic cysts are so rare that this diagnosis is not common preoperatively. Only 6-10% suffer from dysphagia, dyspnea, stridor, hoarseness, cervical pain or vocal paralysis caused by compression of the recurrent laryngeal nerve, trachea or esophagus by the mass (9-11). There are reports of various pathologies that indicate the defective pathways of embryologic descent of thymic primordial, the leading cause of a clinical spectrum of anomalies of the thymus (12). There are three mechanisms for pathogenesis of ectopic thymus in the neck: aberrant descent, sequestration of thymic tissue and failure of involution (3). The development of thymic cyst is caused by persistence of thymopharyngeal duct or degeneration of Hassall’s corpuscles within the thymic remnant (13). As thymus is larger before puberty, about two thirds of these lesions occur during the first decade of life (1). They can be seen at any level of normal thymic descent from the mandible to the mediastinum. Fifty percent of these cystic masses are continuous with mediastinal thymus (14). Thymic cysts are more frequent in males, usually asymptomatic and located left sided, deep or anterior to the sternocleidomastoid muscle (15). They can enlarge during an upper respiratory tract infection, as in our case (9, 14, 16). Differential diagnosis of a cervical mass in a child includes congenital cysts such as bronchiogenic or thyroglossal duct, cystic hygroma, lymphadenopathy, lymphangioma, hemangioma, lymphoma, soft tissue sarcoma and thyroid or parathyroid lesions (17, 18). But thymic cysts should always be included in the differential diagnosis of lateral cervical masses, especially in children (11, 19).
CT scan can help to differentiate thymic cysts from other differential diagnoses and MRI can help to detect the connection of the abnormal mass to the thymus (2). Surgery is the treatment of choice and helps to establish the definitive diagnosis (10). Presence of normal thymus gland in the mediastinum must be confirmed before surgery to avoid postoperative immune dysfunction (1). For the definite diagnosis of a thymic cyst, the histopathologic examination is necessary in which Hassall’s corpuscles and/or cholesterol granulomas are revealed. The cyst wall lining may be spindle, cuboidal, columnar, stratified, pseudostratified, ciliated or non-ciliated. Malignant degeneration has not been reported in children. Very rarely, cyst may adhere to surrounding structures, like internal jugular vein, internal carotid artery, vagus, phrenic, hypoglossal or recurrent laryngeal nerves, microscopically (13). examinations usually demonstrate a cyst with epithelial lining, lymphoid foci, granulomas and cholesterol or keratin crystals (20). The prognosis is excellent since no case of recurrence has been reported (3). Although thymic cysts situated in the neck are uncommon they should be included in the differential diagnosis of cervical masses preoperatively, especially in the young children to prevent unwished events.