1. Background
Medical malpractice is a serious problem in the healthcare system and a threat to the safety of patients, and it may occur in any stage of the care process (1). Assuring the safety of patients is the first crucial step in the improvement of the quality of care and reducing medical errors (2). The problems arisen from the lack of patient safety mostly are systematic and less involve individual errors.
Although eliminating clinical errors is not entirely achievable, avoiding it is a key component of health care quality. Moreover, patients’ safety plans are aimed to just minimize failures and reduce the harm to the patients (3, 4).
Likewise, the rate of adverse events is high among hospitalized children. Studies conducted on NICU and PICU patients reveal high rates of harm, with 74 and 203 adverse events(AEs )per 100 patients in the NICU and PICU, respectively (5). A Canadian study of adverse events in children identified a 9.2% rate of iatrogenic complications in 3,700 children, 45% of which could be preventable (6). The rates of adverse events are still lower than in adults, but we cannot exclude the possibility of postoperative life-threatening events in pediatric surgery (7). Performing risk management plans by the national center of patient’s safety indicated that the number of medical events decreased from 3,643 in 2008 to 2,412 in 2009 (8).
Determining the risks of the procedure and potential reasons for errors is the first step to achieving a safe system in healthcare. It is effective to do a systematic assessment of the healthcare sector and implement various risk preventive measures to apply risk management for preventing these events (9). Failure Mode and Effect Analysis (FMEA) is one of the valid programs for risk management and error prevention. It was introduced by the U.S. Department of Veterans Affairs, National Center for Patient Safety (10). Healthcare Failure Mode and Effect Analysis (HFMEA) was specially designed for health care organizations to prevent failure modes (11).
In other words, HFMEA is an improvement strategy to identify and prevent the medical failures before they occur, and is widely used in the health care system (12).
The pediatric surgery ward is among the riskiest wards of a hospital recognized based on organizational, academic, environmental, and technological needs. The pediatric wards require the double care for patients, not only because of meaningful differences in anatomy, treatment response, the possibility of diagnostic procedures than in internal medicine but also because of the limited communication with patients that are often unable to voice their complaints or precisely describe and locate the symptoms (6, 13). The medical error occurs in more than one-half of children admitted for general pediatric surgery, leading to several unfavorable outcomes (14). Therefore, applying systematic and comprehensive methods in different surgical wards would result in remarkable outcomes. However, risk prevention strategies are not even fully implemented in developed countries (15).
2. Objectives
The present study aimed to examine the risk assessment of processes in the Pediatric Surgery Department of Ghaem Hospital in Mashhad using the Healthcare Failure Mode and Effect Analysis (HFMEA) in 2013 - 2014.
3. Methods
3.1. Research Design and Setting
A mixed-method study (qualitative action research and quantitative descriptive cross-sectional study) was conducted with five processes selected in the Pediatric Surgery of Qaem Hospital in Mashhad from December 2017 to June 2018. Qeam Hospital is one of the biggest centers in Iran, with 815 active beds, 18 departments, seven emergency departments, and various clinical and para-clinical services. In addition, this hospital is a medical education and research center where medical students are trained for specialty and subspecialty degrees.
3.2. Data Collection
Data were collected through focus groups, interviews, observations, and brainstorming. The team members controlled the validity of the study at the end of each phase. The five steps of HFMEA were used in the study (10); however, some modifications were made in practice.
3.2.1. First Step: Definition of HFMEA
Seven members in the pediatric surgery team were asked to select five procedures out of 25 procedures listed in the department based on patient dissatisfaction and the probability of harms caused by the shortcomings of the procedure, and then to list them in order of priority from 1 to 5. Then, the data from the voting were organized according to the Borda number (16), and the five high-priority processes were selected for risk management.
3.2.2. Second Step: Establishment of the Team
In this process, the HFMEA team included seven members: one person in charge of risk management (team leader), one health care manager (consultant), one supervisor, one professor in the field of pediatric surgery, two nurses, one physician, one laboratory expert, and one health information expert
3.2.3. Third Step: Illustration of the Process
At this stage, the process and its sub-processes were designed, modified and approved in focus group discussion, and was drawn on a flow diagram using VISIO software.
3.2.4. Fourth Step: Hazard Analysis
The hazard analysis was conducted in four phases.
First phase: Determining the potential failure mode: At this stage, the failure modes of sub-processes of the selected ward were identified by the triangular method (17) and classified according to nursing errors in the clinical management model (NECM) (18).
Second phase: Determining the hazard score: The hazard score was obtained based on the hazard scoring matrix (multiplying severity by the possibility of the failure occurrence), and it was recorded in the HFMEA form. The severity was rated by the professional comments of team members, and the probability was rated by the staff dealing with that process. Finally, the collective viewpoints were entered in the ultimate report as mean scores. The failures were classified into four interventional levels, including emergency, urgency, programming, and monitoring based on the hazard score in the hazard score matrix (19) (Table 1).
| Intervention Level | Severity and Probability | Catastrophic (4) | Major (3) | Moderate (2) | Minor (1) |
|---|---|---|---|---|---|
| Critical = level 1 | Frequent (4) | 16 | 12 | 8 | 4 |
| urgent = level 2 | Occasional (3) | 12 | 9 | 6 | 3 |
| Programming = level 3 | Uncommon (3) | 8 | 6 | 4 | 2 |
| Monitoring = level 4 | rare (1) | 4 | 3 | 2 | 1 |
Third phase: Plotting the decision making tree: We decided on how to proceed or stop each of the failure modes (hazard score ≥ 8) based on the three items of weakness point, existing control, and detestability.
Fourth phase: Factors affecting failure modes in the decision tree: The factors affecting failure modes in the decision tree were identified based on the cause-effect analysis. Furthermore, the root causes of failure modes were classified with the hazard score ≥ 4 in brainstorm meetings with some of the team members.
3.2.5. Fifth Step: Measured Actions and Outcomes
The actions and outcomes were measured in two phases. The strategies suggested for each factor affecting the failure mode were presented, and an action plan was designed with the theory of inventive problem-solving to improve each failure mode. Finally, its application was decided on based on organizational sources.
4. Results
By implementing the voting method, five out of 25 processes in pediatric surgery were selected, as follows: Admission and profile making, nursing care, the patient’s first visit, the consulting or visit from other services and the process of performing, and sending and pursuing the test results.
Generally, for 5 selected processes per25 listed steps, 48 sub-processes and 218 failure modes were recognized. The number of identified failure modes and the number of intervention levels for selected processes are demonstrated in Table 2.
| Process/Activity | Frequency of Sub-Processes | Frequency of Error Modes | Max Hazard Score | Min Hazard Score | Frequency of Hazard Scoring | |||
|---|---|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 4 | |||||
| Admission and profile making in the sector | ||||||||
| Issuing the inpatient recommendation letter in the clinic | 2 | 8 | 4 | 1 | 0 | 0 | 4 | 3 |
| The patient’s referral for possessing a bed | 2 | 7 | 9 | 2 | 0 | 1 | 5 | 2 |
| Central admission and primary profile preparation | 5 | 19 | 8 | 1 | 0 | 0 | 11 | 8 |
| Making the patient's profile and guiding to the bed | 4 | 11 | 6 | 2 | 0 | 0 | 5 | 6 |
| Primary visit/checkup of the patient | ||||||||
| Making patient’s profile in the ward/sector | 1 | 4 | 4 | 2 | 0 | 0 | 3 | 1 |
| Collecting the biography/history of the patient in the intern and medical checkup examinations by the resident | 5 | 18 | 6 | 2 | 0 | 0 | 12 | 6 |
| Performing the necessary tests and graphs | 1 | 4 | 9 | 3 | 0 | 1 | 2 | 1 |
| Checking and following the physician’s orders | 3 | 17 | 9 | 2 | 0 | 0 | 7 | 10 |
| Consulting or visiting other services | ||||||||
| Issuing of the consulting request by the physician and checking the request | 3 | 11 | 6 | 2 | 0 | 0 | 5 | 6 |
| Sending the consultation request letter | 1 | 3 | 4 | 4 | 0 | 0 | 2 | 1 |
| The presence of the consulting physician in the ward and performing the examinations | 2 | 10 | 4 | 2 | 0 | 1 | 4 | 5 |
| New issuing of the order by the physician and implementing it | 4 | 11 | 4 | 3 | 0 | 0 | 5 | 6 |
| Conducting, laboratory management and following up the test results | ||||||||
| Physician order for laboratory and checking the order (the stage before analysis) | 2 | 8 | 9 | 2 | 0 | 1 | 6 | 2 |
| Registering the test request in the computer and test directory (the stage before analysis) | 3 | 11 | 6 | 1 | 0 | 0 | 6 | 4 |
| Collecting the sample and sending it to the laboratory (the stage before analysis) | 5 | 16 | 6 | 2 | 0 | 0 | 11 | 5 |
| Controlling the sample and doing the lab tests on the sample (analysis stage) | 4 | 16 | 6 | 2 | 0 | 0 | 16 | 0 |
| Issuing the test result (the stage after analysis) | 1 | 3 | 9 | 6 | 0 | 2 | 1 | 0 |
| Using the test results in the related ward (the stage after analysis) | 2 | 6 | 6 | 2 | 0 | 0 | 3 | 3 |
| Care and nursing of the patient | ||||||||
| Issuing the order by the physician | 2 | 9 | 9 | 2 | 0 | 2 | 4 | 3 |
| Checking and entering the physicians’ orders in the patient’s kardex by the nurse | 2 | 6 | 6 | 3 | 0 | 0 | 4 | 2 |
| Performing the physician’s orders and registering the nursing report | 2 | 16 | 6 | 2 | 0 | 0 | 7 | 9 |
| Collecting and delivery of the patient’s profile to the secretary of the ward | 1 | 4 | 4 | 3 | 0 | 0 | 0 | 4 |
| Total | 48 | 218 | 9 | 1 | 0 | 8 | 123 | 87 |
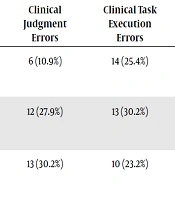
Table 3 shows the classification of the error modes for the selected processes based on nursing errors in the clinical management model (NECM). In general, eight error modes were considered as high risk and unacceptable failures (risk score ≥ 8) and transferred to the decision tree. The factors influencing error modes with high risks and action recommendation strategies are shown in Table 4. Finally, the improvement strategies were suggested using the TRIZ method for the selected processes in the pediatric surgery ward.
| Process Steps | Care Process Errors | Communication Errors | Administrative Processes Errors | Knowledge and Skill Errors | Total | ||
|---|---|---|---|---|---|---|---|
| Clinical Judgment Errors | Clinical Task Execution Errors | Continuity of Care Errors | |||||
| Admission and profile making in the ward | 6 (10.9%) | 14 (25.4%) | 7 (12.7%) | 21 (38.1%) | 5 (9.1%) | 2 (3.6%) | 55 |
| Primary visit/checkup of the patient | 12 (27.9%) | 13 (30.2%) | 3 (6.9%) | 8 (18.6%) | 4 (9.3%) | 3 (6.9%) | 43 |
| Consulting or visiting other services | 13 (30.2%) | 10 (23.2%) | 6 (13.9%) | 5 (11.6%) | 2 (4.6%) | 7 (16.2%) | 43 |
| Conducting, laboratory management and following up the test results | 7 (10.6%) | 23 (50%) | 4 (6.06%) | 11 (16.6%) | 5 (7.5%) | 6 (9.09%) | 66 |
| Care and nursing of the patient | 6 (14.2%) | 13 (30.9%) | 3 (7.1%) | 8 (19.1%) | 8 (16.6%) | 4 (11.9%) | 42 |
| Total | 44 (17.6%) | 83 (33.3%) | 23 (9.2%) | 53 (21.2) | 24 (8.9%) | 22 (8.8%) | 249 |
| Hazard Analysis | Action and Outcome Measures | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Failure mode | Potential causes | Scoring | Decision Tree Analysis | Proceed | Action Type | Actions or Rationale for Stopping | ||||
| Severity | Occurrence | Hazard Score | Weakness Point | Existing Control measures | Delectability | |||||
| The request for an unnecessary test by the physician | A: Lack of attention to the patient’s clinical symptoms, B: Lack of expertise in newly registered physicians | 3 | 3 | 9 | → | No | No | Yes | Control | Defining physician’s performance assessment criteria, based on the observed malfunctions and periodical assessment of the physicians and providing feedback to them; proper communication with the patient; Encouraging physicians to ask in the case of obscurity; periodical training of newly registered physicians; considering the Advisory comments of other clinical experts by the service provider if necessary |
| Error in entering the test results | A: Heavy workload and the staff fatigue, B: Lack of sufficient knowledge, C: Lack of sufficient experience | 3 | 3 | 9 | → | No | No | Yes | Control | Planning and management of performance during the work shifts; responsibility sharing; preparing tables for work shifts and avoiding long shifts; Investigating and monitoring the performance and checking the final test results by the technical expert; providing a smart data system that possesses alarms in the case of out of range tests results; periodical training of staff; defining the guidelines for introducing the newly registered physicians with the existing criteria in the wards |
| Delay in registering the test results | A: Lack of attention and ignorance, B: Lack of knowledge of the consequences, C: Heavy workload, D: Lack of analysis on the sample due to the problem in the sample | 3 | 3 | 9 | → | No | No | Yes | Control | Defining staff performance assessment criteria based on the observed malfunctions; Training of providers regarding the culture of safety and taking responsibility for the safety of patients; holding reminder courses for the personnel; Adjusting the workload with the human resources; Improving the personnel’s awareness regarding the proper methods of collecting samples; communication of information between the technical expert and the ward. |
| The patient’s delay in entering the ward for making the organizations | A: lack of information transfer, B: improper designing of the ward and lack of sufficient signs | 3 | 3 | 9 | → | No | No | Yes | Control | Improving the patient’s awareness using effective communication and offering brochures to the patients and attracting their contribution; registering the names and reminder calls to the patient one day before the in-patient date; Installing the ward’s frame in a proper and eye-catching point; revising the hospital policies; 5S (methodology) in the ward. |
| The delay in the consulting physician at the patient’s sight | A: Lack of information transfer, B: Lack of proper teamwork, C: Lack of recognition of the right patient and providing consultation for another patient | 3 | 3 | 9 | → | No | No | Yes | Defining the patient’s consulting guidelines and acquiring assurance regarding the properness of the executive method; conducting the necessary follow-ups by the head nurse; adjusting the workload with the number of HR; organizing the medical team; Improving the teamwork via holding teamwork training courses; responsibility and responsiveness of individuals by defining a clear and written job description; Following the guidelines and performance methods for recognizing the right patient; effective communication with the patients | |
| Missing some of the necessary graphs or tests | A: Lack of teamwork, B: Lack of attention and preciseness in registering the commands, C: Missing the request letter for graphs or tests | 3 | 3 | 9 | → | No | No | Yes | control | Monitoring the processes; harmonized performance of the medical team; responsibility and responsiveness of the individual offering services via clear written job description; Ordering a special file for each patient in the nursing station and placing the patients request sheets in each of them separately; rapid registration of the diagnostic and para-clinical acts by the nurse or secretary of the ward; informing the physician regarding the completion of the necessary orders requested by him |
| Shortcoming in punctual diagnosis by the resident | A: lack of expertise, B: lack of proper communication with the patient | 3 | 3 | 9 | → | No | No | Yes | control | Considering the consulting viewpoints of other clinical experts; offering services, if necessary; holding re-training courses in the definite intervals for the clinical staff; Assessing the patient’s capability for building an effective communication |
| Incomplete registration of data in the physician’s order sheet | A: lack of knowledge regarding the significance of the issue, B: lack of sufficient supervision | 3 | 3 | 9 | → | No | No | Yes | control | Defining the guidelines and methods of performance clearly and periodical revising of them; continuous and periodical training for the individual offering the services; installing the electronic prescription system; continuos supervision on performance; providing feedback to the personnel regarding malfunctions. |
Among the improvement strategies for the admission and profile making were the re-engineering of the admission process, continuous supervision on the trend of admission and in-patient care, preparing and organizing the executive guidelines, defining the written responsibilities for the admission unit and announcing them, preparing the performance assessment criteria and conducting periodical assessment and offering feedback to the personnel, continuing education and proper training content based on the needs of the personnel, reducing the workload and correcting the lack of workforces, maintaining effective relations with the patient and companions and teaching all rules of the ward in welcome notes during admission, and presenting sufficient information and training patients via brochures before entering the ward.
The improvement strategies for the process of the patient’s first visit included preparing new forms with special parts for ensuring the complete registration of data, physicians’ training on how to write the prescription, improving the process of patient identification and revising guidelines for correct identification of patients, holding teamwork training courses, attracting patient’s contribution by making effective relationships with them, setting standards for assessing performance, presenting feedback to the staff, inter-ward communications, and enhancing the ward control ability of the person in charge of the shift work.
5. Discussion
In this study, using a prospective method, we employed the healthcare failure mode and effect analysis to identify the probable errors of selected processes in the pediatric surgery and the effective causes of errors and define the improvement strategies. Some differences were found in the suggested models, as follows: (1) high-risk processes selected through the voting method; (2) failure classification within the nursing failure management model framework; (3) development of more comprehensive and convincing methods for scoring the failure level; and (4) failure classification through medical failure preventive strategies.
The voting method was used to rank and select the high-risk processes, which is in line with the study by Molavi Taleghani et al. (2). However, Anderson et al. used a risk assessment matrix and mean error scores for choosing and ranking high-risk processes in the surgical ward (20). In the present study, team members with different disciplines identified and evaluated the risks related to the pediatric surgery ward. Dominici indicates that it is essential to have team members with different disciplines for evaluating the effect of HFMEA on the quality of patient care and realizing and categorizing probable risks (21).
There are various methods for classifying errors. In all previous studies, medical errors were classified retrospectively (22, 23). In the current study, the classification of error modes was based on nursing error management in the clinical management model. They included 60.13% caring errors, 21.1% communication errors, 8.9% executive process errors, and 8.8% errors related to knowledge and skill. In the study performed by NECM, the most frequent errors included caring errors (66%), communication errors (22%), executive process errors (6%), and errors related to knowledge and skill (5%), which are in agreement with the results of the current study (18).
In this study, the interventional levels, including programming, monitoring, emergency, and urgency, were predicted for each error mode concerning the hazard score. This method is suggested because corrective actions and decreases in error risks are based on the interventional levels (16). In Bonefant et al. (24) study, of 93 errors in the dialysis ward, 0% were in the emergency intervention area, 9.6% in the urgency area, 38.7% in the programming area, and 51.6% in the monitoring area, which is in line with the present study. In the present study, the frequency percentage of error modes were in the interventional areas of programming, monitoring, urgency, and emergency.
In the HFMEA study, according to the process under investigation, defining the score of the undesirable risk is done differently. In this study, undesirable risks had scores ≥8, and their causes need to be found. Besides, the scores of unacceptable risks were in line with most studies performed with the HFMEA technique (11).
The crucial points to the safety of patients include assuring the capability of the staff, re-engineering organizations, and parallel consideration of obvious and clandestine causes to discover and correct the errors in time. Concerning insufficient resources in each health care system, the most economical strategies and methods should be chosen to remove the causes of failures (25). In this study, among the offered strategies according to the TRIZ were the improvement of patient recognition, creating and revising the guidelines and clear performance methods, the contribution of patients to the treatment procedure, re-engineering and monitoring the work procedures, holding workshops and teaching recommendations and regulations, and improving the relations among the sectors; they were executive strategies in the pediatric surgery ward in Ghaem Hospital included in the performance agenda.
The improvement strategies for care and patient nursing included revising the guidelines for checking the physician’s orders and patient’s recognition, obeying the oral orders only in urgent cases, proper supervision on the correct re-check techniques, supporting the staff to ask their questions in the case of ambiguity, settling the lack of human resource, improvement strategies in performance processes, sending and following the test results in the form of root analysis of events and reporting the critical results, continuous supervision and controlling the performance procedures, improving the team relations, checklists for maintenance of the tools and facility management, adjusting the workload with the staff, facilitating the processes and removing the unnecessary steps, enhancing software for including the physician’s orders for tests and presenting a reference laboratory and conducting some of the important tests randomly in various periods as binary tests by the hospital laboratory and the reference lab.
Finally, it is worth mentioning that performing the strategies and recommended acts is strongly correlated with the contributions of the team and financial support from the leaders of the organizations. In the Latino perspective, even if the prospective risk assessment is annually performed for high-risk processes, but the management of the organization does not consider this action as a long term strategy for the improvement of safety, the results of the prospective risk assessment would be of short-term nature (26). Furthermore, Duwe et al. study indicated that the success of the prospective risk assessment plans is connected to effective, committed, and permanent leadership (27).
One of the research constraints was that high-risk errors in every institute depend on the climate of the organization and it is not possible to compare the results with other institutions. The frequency and intensity of errors are not even the same in various units of different hospitals, and a change in people can change the results to a high degree (28).
5.1. Conclusions
It is very effective to use HFMEA for realizing possible failures in treatment procedures, the reasons for each failure mode, and the development of improvement strategies. Therefore, HFMEA can be used as a risk assessment model in healthcare systems. Besides, HFMEA can reduce failures and their consequences, and it can be used in quality improvement and risk reduction. Risk management techniques, combined with the commitment of managers and the renewal of organizational policies, can ensure the effectiveness of these activities.