1. Introduction
Shunt dysfunction may be associated with under or over drainage of shunt or shunt infections (1). The most common cause of underdrainage is the obstruction of the ventricular catheter (2). The two most common causes of peritoneal catheter obstruction are the placement of a catheter to the pre-peritoneal cavity and intraabdominal pseudocysts (3). Overdrainage of the shunt is a problem associated with the pump and may result in a subdural hematoma or fluid collection (4, 5), slit ventricle syndrome (6), or isolated fourth ventricle syndrome (7). In spite of all these complications, shunt treatment is the first choice in hydrocephalus. Pseudocyst, which was developed in our case, is a rare complication of ventriculoperitoneal shunt presenting with a mass in the abdomen, stomach ache, intestinal obstruction, and shunt function disturbances. The formations occupying a large space in the abdomen may lead to a difficult intubation in anesthesia management and cardiovascular and respiratory problems that may be life-threatening. In addition, they may lead to pathologies by exerting pressure on large vessels and adjacent organs. In association with the rapid drainage of intraabdominal fluid, it may also lead to a rapid fall in thorax pressure and with expansion to lung edema. The aspiration of fluid during drainage may result in the development of severe hypotension (8, 9).
In addition, hydrocephalus is a condition that leads to increased intracranial pressure. The method that will be used during anesthesia management should be one that will not lead to increased intracranial pressure while not leading to decreased cerebral perfusion pressure at the same time. In patients with hydrocephalus, difficulties may be experienced in aeration and during intubation due to their physical characteristics.
2. Case Presentation
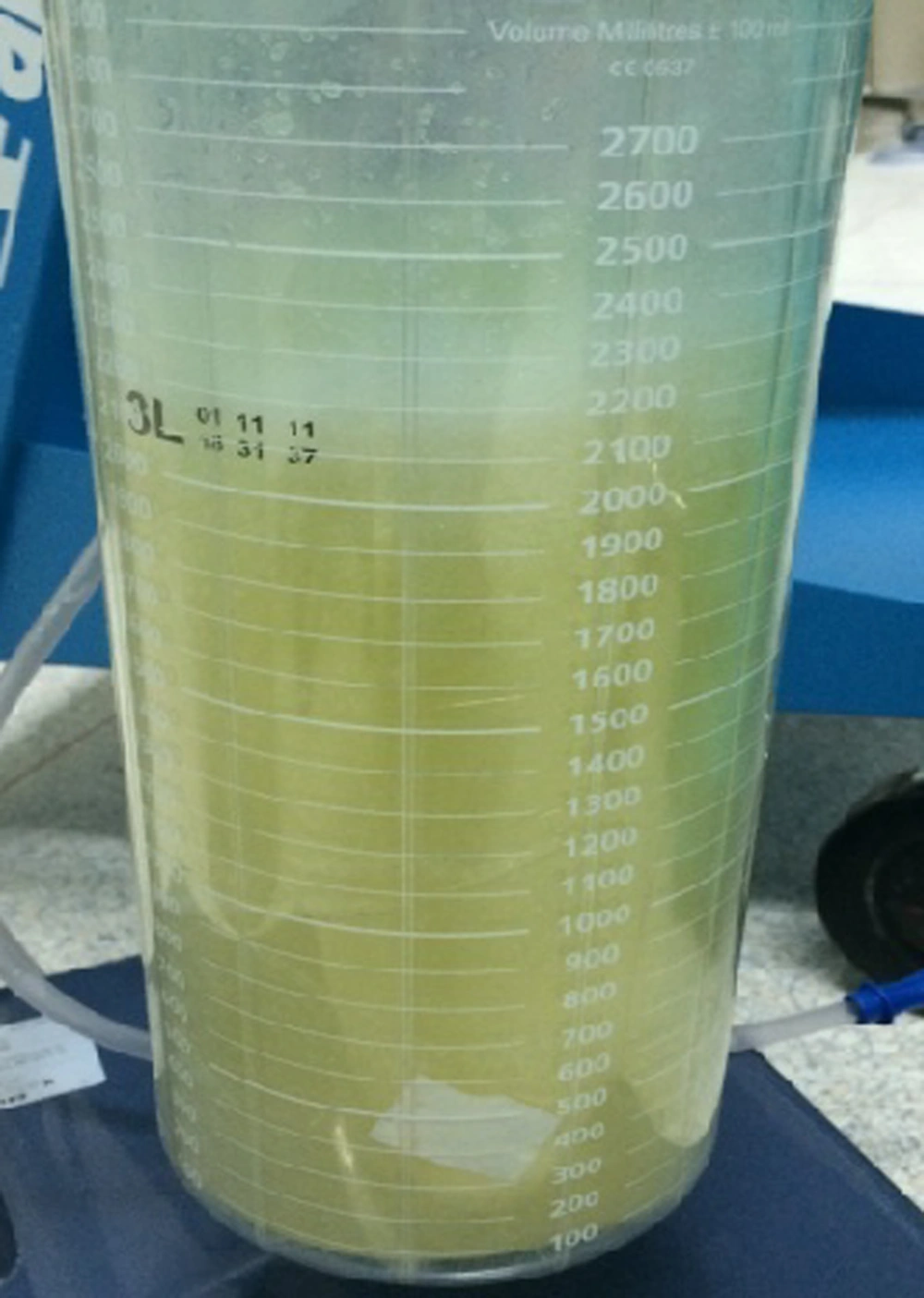
A 4-year-old girl weighing 11 kg undergoing shunt placement with the diagnosis of hydrocephalus was consulted by the pediatric surgery department due to the development of swelling in the abdomen following a shunt dysfunction. In the ultrasonographic examination, a massive free fluid was observed in the abdomen. The patient was planned for operation and monitored by electrocardiogram, pulse oximeter, capnography, and non-invasive blood pressure (NIBP). 20 G external jugular vein cannulation and 22 G peripheric vessel cannulation were carried out. Necessary preparations were made for a probable difficult intubation. After adequate preoxygenation, an induction was carried out with sevorane, 0.6 mg/kg rocuronium (MSD, Istanbul, Turkey), and fentanyl (Talinat, Turkey). The patient was intubated with a tube of the 4.5 mm inner diameter and ventilated at a low pressure in case that the massive intraabdominal fluid exerted pressure on large vessels (Figure 1). In order to prevent hypotension that may be developed during the drainage of intra-abdominal free fluid, 10 mL/kg fluid resuscitation was performed. The fluid was drained from the patient and urine output was monitored. During the operation, overall, 2500 cc fluid (Figure 2) was drained from the patient. In spite of adequate fluid resuscitation, due to a sudden fluid drainage, hypotension and bradycardia were developed. Overall, 1 mg ephedrine and 40 mcg adrenalin were administered (Figure 3). The pediatric surgeon drained intraabdominal fluid and the brain surgery corrected shunt dysfunction. The patient responded to fluid resuscitation and vasopressor treatment and after becoming stable, she was extubated without any complications with the administration of 4 mg/kg sugammadex (Bridion, Merck Sharp and Dohme, Turkey).
3. Discussion
Hydrocephalus is a clinical picture that develops in association with the circulation of cerebrospinal fluid (CSF) or the impairment of the balance between production and absorption of CSF and courses with the expansion of ventricles and increases in intracranial pressure. In patients with increased intracranial pressure (ICP), anesthesia induction and endotracheal intubation are critical. In the induction, a suitable anesthetic that will decrease ICP along with hyperventilation should be chosen. A muscle relaxant is administered in order to facilitate ventilation and prevent contraction and cough, which will increase ICP because arterial hypertension during induction increases brain blood volume and brain edema. Prolonged hypertension may give rise to marked ICP increase, decrease in cranial perfusion pressure (CPP) and risk of herniation. However, an excessive drop in arterial blood pressure may cause a decrease in CPP. The faulty position of lying, respiratory irregularities, fever, hypertension, and metabolic imbalances that may lead to increased intracranial pressure should be eliminated and the goal should be to keep the pressure under 20 mm Hg with hyperventilation, hyperosmolar fluid administration, and drainage of CSF. Another point is that care should be taken to keep CPP at an adequate level.
As in our case, space -occupying lesions in the abdomen may lead to problems in respiration and circulation during anesthesia management. It poses risks of difficult intubation, aspiration due to pressure, and massive bleeding. After the drainage of cysts, due to re-expansion of the lung, pulmonary edema may develop (10, 11). Masses occupying a large space in the abdomen may lead diaphragm to rise and respiratory functions to be impaired by rendering rib cage narrower. During the administration of muscular relaxants, the compliance between lung and diaphragm is impaired and respiratory management becomes even more difficult. The high airway pressure is also likely to lead to lung injury (12). The drainage of large cysts may cause bleeding, hypotension, and electrolyte disturbance along with morbidity and other serious problems.
Due to these risks, preoperative preparation is necessary to prevent adverse effects both intracranially and in respiratory and circulatory systems. In order to control hemodynamic alterations that may develop during operation and to prevent a secondary damage caused by ICP, brain oxygenation should be followed (jugular bulb oximeter brain tissue PaO2 oximeter) and fever, pulse oximeter, blood pressure, blood sugar and electrocardiogram monitoring should be carried out. In addition, pulse oximeter, fluid balance (monitoring of fluid input and output, central venous pressure, and urine density), blood-electrolyte, and intracranial pressure monitoring are also necessary. In the postop period, both hemogram and electrolyte monitoring are recommended.
3.1. Conclusions
Space-occupying lesions after ventriculoperitoneal shunt dysfunction performed for hydrocephalus may lead to life-threatening problems due to intracranial, respiratory, cardiovascular, and circulatory impairment. Due to the probability of the development of these conditions, each case should be evaluated meticulously in the preoperative period by anesthetists and the anesthesia method that will be used should be determined. Proper hemodynamic monitoring, management of fluid balance, and ventilator monitorization are important.