1. Background
Acute lymphoblastic leukemia (ALL) is the most common cancer diagnosed in children, and B-cell is the most common type of ALL (1). ALL has approximately an overall survival of 80% with certain subsets experiencing greater than 98% cure rate (1).
Currently, 80% - 85% of children with ALL can be cured through the application of reliable prognostic factors permitting the employment of risk-oriented treatment protocols (2).
The most important determinant of prognosis in ALL is treatment, and ALL is a fatal disease without the effective treatment. Until the mid-1960, no effective treatment was known for this disease, and the five-year survival was less than 10% (3).
Over the years, different protocols are employed to treat patients with ALL in different countries.
There is a remarkable improvement in the outcome of the childhood ALL as a result of serial clinical trials conducted by pediatric oncology cooperative groups. These groups studied the disease biology and followed risk directed combination therapy with better supportive care (4).
In Mofid Children’s Hospital located in Tehran, Iran, newly diagnosed cases of ALL are randomly treated with two protocols, COG (5) and modified BFM 2000 protocols called Mofid Children’s Hospital protocol (MCHP) (Table 1).
| Standard Risk, Pre/Early Pre B-Cell ALL | High Risk, Pre/Early Pre B-Cell ALL | |
|---|---|---|
| Induction | Prednisolon: 30 mg/m2, po, 28 d; VCR:1.5 mg/m2, iv, on days 1, 7, 14, 28; L.Aspar: 6000 U/m2, im, on days 2, 5, 8, 12, 15, 19; ADR:25 mg/m2, iv, 3 doses (end of induction); IT: MTX + cytozar, weekly for 4 wk | Prednisolon: 30 mg/m2, po, 28 d; VCR:1.5 mg/m2, iv, on days 1, 7, 14, 28; CPM: 600 mg/m2, iv, on the 1st wk; L.Aspar: 6000 U/m2 im, on days 2, 5, 8, 12, 15, 19; ADR: 25 mg/m2, iv, 3 doses (end of induction); IT: MTX + cytozar, weekly for 4 wk |
| Post-induction | Cytozar: 120 mg/m2, iv, days 1 - 7; L.Aspar: 6000 U/m2, im, 7 doses, every other day; VP16: 100 mg/m2, iv, on days 1 and 7 | Cytozar: 120 mg/m2, iv, days 1 - 7; L.Aspar: 6000 U/m2,im, 7 doses every other day; VP16: 100 mg/m2, iv, on days 1 and 7 |
| Consolidation; 1 mo | L.Aspar: 1000 U/m2, im, 16 doses,every other day; VCR: 1.5 mg/m2, iv, after 3 doses of L.Aspar; MTX: 2 g/m2, iv, 1 dose; Dexamethason: 6 mg/m2, po, for 1 mo; Danamycin: 25 mg/m2, iv, weekly for 4 wk | L.Aspar: 1000 U/m2, im, 16 doses, every other day; VCR: 1.5 mg/m2, iv, after 3 doses of L.Aspar; CPM: 600 mg/m2, iv, after 3 doses of L.Aspar; VP16: 100 mg/m2, iv, every 2 weeks, totally 8 doses; MTX: 2 g/m2, iv, 1 dose; Dexamethason: 6 mg/m2, po, 1 mo; Danamycin: 25 mg/m2, iv, weekly for 4 wk |
| Maintenance; 3 y | 6MP: 50 mg/m2, po, daily + MTX: 20 mg/m2, po, weekly for 3 y; VCR: 1.5 mg/m2, iv, + Prednisolon: 30 mg/m2, po, for 5 d: every 21 d for 2 y; IT: monthly in first year and every 2 mo in second y | 6MP: 50 mg/m2, po, daily + MTX: 20 mg/m2, po, weekly: for 3 y; VCR: 1.5 mg/m2, iv, +CPM: 600 mg/m2, iv, + Prednisolon: 30 mg/m2, po, for 5 d: every 21 days for 2 y; IT: monthly in 1st year and every 2 mo in second y |
Mofid Children’s Hospital Protocol; A Modified BFM Protocol
2. Objectives
The current study mainly aimed at evaluating and comparing the efficacy, and determining the complications of these two protocols to treat childhood ALL.
3. Methods
The current study was performed on ALL patients with type B leukemia treated at Mofid Children’s Hospital from March 2006 to March 2012.
Patients above 12 months newly diagnosed with ALL were reviewed. For these patients, all available medical records, notes, and laboratory data were reported. The total duration of observation was extended to a minimum of five years after starting the treatment.
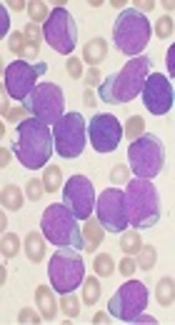
Diagnosis of ALL was established by bone marrow aspiration, and type of ALL was determined by flow cytometry. Only patients with B-cell and early pre B-cell were included in the current study. Based on prognostic factors in childhood ALL (5), patients were divided into two groups: high- and standard-risk. Patients were considered as standard risk (SR) ALL if they were 12 - 119 months old with a presenting leukocyte count of less than 50 × 109/L; otherwise, the patients were classified as high risk (HR).
Patients with CNS involvement were excluded from the current study. Patients in both groups were observed and evaluated for complications and accurately recorded.
Lack of bone marrow remission on day 28 was considered as induction failure (6).
Isolated bone marrow relapse was defined as more than 25% blasts (M3 marrow) at any point after achieving remission in a single bone marrow aspirate or biopsy, without involvement of the CNS and/or testicles. Isolated CNS relapse was defined as positive cytomorphology and WBC 5/μL, and/or clinical signs of CNS leukemia such as facial nerve palsy, brain/eye involvement, or hypothalamic syndrome. Isolated testicular relapse was defined as leukemic infiltration of testicles confirmed by testicular biopsy. Finally, combined relapse was defined as M2 (5% - 25% blasts in the bone marrow) or M3 bone marrow at any point after achieving remission with concomitant CNS and/or testicular relapse (4, 5). Patients were followed up for to five years after starting treatment to determine the five-year overall survival.
Patient data were tabulated and processed with SPSS version 18.0. Chi-square test was employed to identify the associations between the event free survival and the studied independent variables. The Kaplan-Meier method was used to show the survival curves; P values ≤ 0.05 were considered significant (7).
4. Results
4.1. Patient Characteristics
A total of 108 patients were enrolled into the current study; 56 (51.9%) patients were male and 52 (48.1%) female; 57 (52.8%) and 51(47.2%) patients were treated with MCHP and COG protocols, respectively; 39 (36.1%) patients were categorized as HR and the rest of them, 69 (63.9%) patients, as SR.
In MCHP and COG protocols 66 (61.1%) and 35 (61.4%) patients, respectively, had pre B-cell ALL.
Patient characteristics are summarized in Table 2.
| Total | MCHP Group | COG Group | |
|---|---|---|---|
| Patients | 108 | 57 (52.8) | 51 (47.2) |
| 12 - 119 mo | 94 (87) | 52 (91.2) | 42 (82.4) |
| ≥ 120 mo | 14 (13) | 5 (8.8) | 9 (17.6) |
| Male | 56 (51.9) | 30 (52.6) | 26 (51) |
| Female | 52 (48.1) | 27 (47.4) | 25 (49) |
| Pre B-cell ALL | 66 (61.1) | 35 (61.4) | 31 (60.8) |
| Early pre B-cell ALL | 42 (38.9) | 22 (38.6) | 20 (39.2) |
| High-risk | 39 (36.1) | 18 (31.6) | 21 (41.2) |
| Standard-risk | 69 (63.9) | 39 (68.4) | 30 (58.8) |
Demographic and Clinical Data of the Studied Patientsa
In MCHP and COG protocols 45 (78.9%) and 43 (84.3%) patients, respectively, had WBC < 50000. HGB < 7 g/dL was observed in 17 (29.8%) and 20 (39.2%) patients treated with MCHP and COG protocols, respectively.
Platelet count ≥ 50000/mm3 in 37 (64.9%) and blasts in peripheral blood smear in 31 (54.4%) patients with MCHP were observed; 88 (81.5%) of all patients, 48 (84.2%) patients in MCHP protocols and 40 (78.4%) in COG protocol, had normal cytogenetic study (Table 3).
| Total | MCHP Group | COG Group | |
|---|---|---|---|
| WBC < 50000/mm3 | 88 (81.5) | 45 (78.9) | 43 (84.3) |
| WBC ≥ 50000/mm3 | 20 (18.5) | 12 (21.1) | 8 (15.7) |
| HGB < 7 mg/dL | 37 (34.3) | 17 (29.8) | 20 (39.2) |
| HGB ≥ 7 mg/dL | 71 (65.7) | 40 (70.2) | 31 (60.8) |
| PLT < 50000 /mm3 | 39 (36.1) | 20 (35.1) | 19 (37.3) |
| PLT ≥ 50000 /mm3 | 69 (63.9) | 37 (64.9) | 32 (62.7) |
| Blast in PB | 59 (54.6) | 31 (54.4) | 28 (54.9) |
| Normal cytogenetic | 88 (81.5) | 48 (84.2) | 40 (78.4) |
Laboratory Results at Baselinea
4.2. Treatment Results
4.2.1. Induction Failure
Induction failure in all patients was 8.3% (n = 9). Induction failure was more in MCHP protocol than COG protocol (n = 6; 10.5% vs. n = 3; 5.9%); although the difference was not significant (P = 0.390). No other factors except WBC ≥ 50000 (P = 0.049) had a significant effect on induction failure.
4.2.2. Relapse
Relapse rate was 9.3% in all patients. Seven patients in MCHP (12.3%), 3 (40%) in BM, and 4 (60%) in CNS were relapsed. Relapse in the COG group was 5.9% (n = 3), one in BM, one in CNS, and one in BM + testis. There was no testicular relapse in the MCHP group. Mean relapse time in the MCHP group was 9.18 months and in the COG 22.67 months (P = 0.012).
Relapse in the MCHP group was not significantly different from that of the COG group (P = 0262).
In both groups, relapse was higher in high risk patients (P = 0.009) and also in patients with WBC ≥ 50000 (P = 0.013).
4.2.3. Complication
Patients were monitored for two complications: bleeding and infection; totally, 56.6% (n = 61) of all patients, 64.9% (n = 37) in the MCHP, and 47.1% (n = 24) in the COG groups had no complications.
Bleeding was observed in 10.5% (n = 6) of patients in the MCHP and 5.9% (n = 3) of the ones in the COG groups (P = 0.934). But, infection was lower in patients with MCHP (22.8%; n = 13) than the ones with COG (41.2%; n = 21) (P = 0.016).
4.2.4. Overall Survival
After five years of observation, overall percentage of survival was 93% in the MCHP group and 96.1% in the COG group (P = 0.489).
In the MCHP group, the death reason in two patients (50%) was infection, in one patient (25%) relapse, and in one patient (25%) other causes.
In the COG group, only two patients died, one of them from infection and the other one from relapse. In summary, the most common cause of death was infection.
5. Discussion
Induction failure in the MCHP group was 10.5% and in the COG 5.9% (P = 0.390). Hyperleukocytosis (WBC count ≥ 50000/L) (P = 0.049) was an important factor in induction failure.
In the MCHP, WBC ≥ 50000 was observed in 12 (21.1%) patients, while WBC ≥ 50000 was less in the COG group (n = 8; 15.7%). This result was comparable with other studies such as the ones by Schrappe et al. (19.7% to 22.3%) (8), Karimi (20%) (9), and Gaynon et al. (21% to 22.8%) (10). But this result was less than that of the study by Hussein et al. from Egypt (39.6%), which included an older age group (0 - 18 years) (11).
Failure of induction therapy is an uncommon event occurring in fewer than 5% of children with ALL treated with the current regimens (12). But in the MCHP group, this failure was 10.5%.
Relapse was more common in the MCHP group (12.3%); moreover, in this group, CNS relapse was more common than BM. This result was less than those of Ghali with modified UKALL protocol (19.6%) in Baghdad (13) and Kaiserova et al., with BFM 95 protocol (20.5%) in Slovakia (14). Moghrabi et al. reported 16% relapse on protocol 95 - 01 for 491 children with ALL (15).
In another study by Hunger on children with ALL, two chemotherapy regimens of BFM and COG were compared. Toxicity and infections were higher in the BFM group (16). However, in the current study, there was no significant difference between the two groups. But, the rate of complications in the COG group was 53.9%, which was higher than that of the BFM group (35.1%) in the current study. In the current study, infection (31.5%) and then bleeding (8.3%) were the most common complications. In the current study, five-year overall survival in the MCHP group was 93% and in the COG group 96.1%; five-year overall survival was reported 80.3% by Friedmann (16).
Ghali reported that event-free survival was 54% for 559 children (within the age range of 1 to 15 years) treated at CWTH from 2000 to 2009 (13). Survival probability was 71.7% in 171 patients treated according to ALL BFM 95 protocol in Slovakia (14). All of these results were less than those of the current study. Five-year overall survival of 54% was higher than those of the results of most of the well-known cancer centers. The most common causes of death were relapse and infection.