1. Background
Children with congenital heart diseases (CHD) in hypermetabolic state (1) need 50% more energy than healthy ones to have normal growth and development (2). Several reasons can be postulated for malnutrition in these patients, including energy intake decrement, energy requirement increment or both (2). Due to feeding difficulties, inadequate calorie intake is known to play an important role in malnutrition and growth impairment (3). The severity of malnutrition consists of a wide span of mild to failure to thrive (4). Considering weight for age Z-score, length for age Z-score, and head circumference, early and progressive growth failure in the patient with CHD have been proven in comparison to healthy cases (5, 6). Progressive growth failure is associated with poor disease control, impaired cardiac function, and increased mortality and morbidity (7-9). Complicated interactions between medical, surgical, nutritional and social factors have made the CHD a challenge for the physicians (10).
2. Objectives
This study aimed to investigate the prevalence of malnutrition and its association with other factors among the acyanotic patients with congenital heart disease undergoing palliative or corrective surgery.
3. Methods
3.1. Study Design
A retrospective study of medical records of 812 children with acyanotic congenital heart disease underwent palliative or corrective surgery was performed from March 2011 to March 2017 at Children’s Medical Center, Tehran, Iran. The inclusion criteria were defined as the acyanotic patients with congenital heart diseases diagnosed by echocardiography that underwent cardiac surgery. The exclusion criteria were defined as any complex gastrointestinal malformation in addition to the cardiac anomaly, which can affect the nutritional status, such as repaired esophageal atresia. Children with a birth weight under 1300 were excluded as well. Ethical approval for the study was obtained from the Institutional Review Board.
3.2. Data Collection
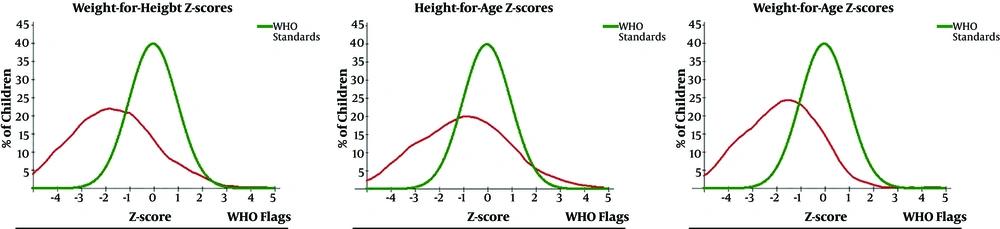
Data were collected from inpatient medical records and cardiac surgery databases. Collected data were comprised of the age at the time of the surgery, gender, weight at the time of the surgery, height at the time of the surgery, birth weight, length of ICU stay, and 1-year mortality. The WAZ, WLZ, LAZ, and BMI Z-scores were calculated according to the WHO standards. All the calculations were done using WHO Anthro (version 3.2.2, January 2011) software. Using 2016 WHO growth references, we classified the Z-scores into 4 groups, including normal (Z-scores > -1), mild (-2 to > -1), moderate (-3 to > -2), and severe (< -3). We considered LAZ determinant of chronic malnutrition, WLZ determinant of acute malnutrition and the WAZ was designated for poor nutritional state and the indicator of immediate aggravation of the health state (immediate malnutrition). The BMI Z-scores also were divided in the same way and were categorized as severely thin, moderately thin, mildly thin, and normal (11).
3.3. Statistical Analysis
The patients were divided according to gender (male and female), type of disease (cyanotic and acyanotic) and severity of malnutrition for each growth index (normal, mild, moderate, and severe). The data were analyzed with SPSS software version 22. The values were expressed with mean + SD and P value less than 0.05 was considered significant.
4. Results
4.1. Study Population
Our study was conducted by reviewing the case notes of all non-syndromic patients with acyanotic CHD who underwent either palliative or corrective surgical repair from March 2011 to March 2017. Among total amount of 812 patients, 375 (46.2%) were female and 437 (53.8%) male. The one-year mortality was 38 (4.6%) among our patients. Our patients had an average age of 23.52 months (± 29.38), the average weight at the time of the surgery was 9.086 ± 6.71 kilograms and the average height at the time of the surgery was 76.93 ± 23.37 centimeters.
4.2. Malnutrition Status in Our Study
In our study, 68.7% and 66.4% of the patients suffered from mild to severe forms of malnutrition based on WAZ and WLZ, respectively (P value < 0.0001, 0.025) (Table 1 and Figure 1) .This indicates that acyanotic patients are more prone to immediate and acute malnutrition. There was no significant difference between male and female in WAZ, WLZ, LAZ, and BMIZ (P value: 0.154, 0.265, 0.965 and 0.667, respectively). Generally, the prolonged ICU stay in acyanotic patients was proposed secondary due to the severity of malnutrition (P value = 0.001), and lower birth weight (LBW) has a significant relationship with the severity of malnutrition in infancy or childhood period (P value < 0.0001). Compared with the normal subjects, the patients with moderate and severe immediate malnutrition had longer ICU stay (P value = 0.022, 0.048, respectively). The similar changes were noted between severe chronic malnutrition and the healthy state (P value = 0.011). In all forms of malnutrition (according to WAZ, WLZ, LAZ, and BMIZ), the LBW can cause more severe malnutrition (P value <0.0001).
| Normal (≥ -1) | Mild (-2 to > -1) | Moderate (-3 to > -2) | Severe (< -3) | |
|---|---|---|---|---|
| WAZ | 249 (31.3) | 194 (24.4) | 163 (20.5) | 189 (23.8) |
| LAZ | 261 (51.4) | 88 (17.3) | 68 (13.4) | 91 (17.9) |
| WLZ | 146 (33.6) | 88 (20.2) | 93 (21.4) | 108 (24.8) |
| BMI-Z | 177 (34.8) | 102 (20.1) | 102 (20.1) | 127 (25) |
The Severity of the Malnutrition Among the Childrena
5. Discussion
Irrespective of the type of cardiac defect and presentment of cyanosis, malnutrition is common among these patients (7). The prevalence of growth impairments is 64% in children with cardiac defects in developed countries (12); however, it is more prevalent and more severe in developing countries with a rate of 90%. In addition, the malnutrition is a usual phenomenon even in healthy children (8, 13, 14). In our study, 68.7% had immediate, 66.4% had acute, and 48.6% had mild to severe forms of chronic malnutrition. Delayed corrective surgeries in developing countries increase the likelihood of malnutrition (15). The prevalence of moderate to severe forms congenital heart defects is considered to be about 6 in 1000 live births (16, 17) and the incidence of moderate to severe forms of malnutrition in patients with congenital cardiac defects is 15%, more occurred in the presence of pulmonary hypertension (18), which the majority of them have low caloric intake and only a few have sufficient nutritional support (18). Several studies demonstrated that the total energy expenditure of the patients with non-corrected CHD is increased (19-21). Trabulsi et al. found that the growth failure in infants with CHD is probably due to insufficient energy intake, but did not to increase energy expenditure (22). Immediate malnutrition even occurs during hospitalizing of the infants with CHD. Clinical status or medically necessary tests and procedures can cause feeding disturbances (23, 24), and gastrointestinal issues (25, 26), and finally, cause inadequate energy intake. As a matter of fact, inadequate caloric intake has been reported in the perioperative period (27). Our study also confirmed that immediate and acute forms were significantly more frequent; in other words, acyanotic patients are more susceptible to these types of malnutrition. This finding highlighted the importance of nutritional support even during the hospitalization and perioperative period.
Infants with ventricular septal defects (VSD) and AVSD accompanied by large left to right shunts (19-21) have higher total energy expenditure compared with healthy infants. According to Salzer et al. study, infants with left to right shunts gain less weight and seem more underweight than infants with cyanotic cardiac defects (9). Previous studies have found that acyanotic defects impact weight gain velocity much more than height changes (28, 29). Wasting or acute malnutrition, ascribed to acute events such as infection, is seen frequently in acyanotic lesions (30). Furthermore, the severity of the growth failure is related to the degree of the hemodynamic impairment (2, 31, 32). The high prevalence of the growth failure in acyanotic patients can be secondary to the delayed surgery due to the nature of the acyanotic disease. Since our center is considered a referral tertiary center, complicated cases are referred for the total correction even after the pulmonary hypertension is established; therefore, it can be deduced that most of our patients suffered from large right to left shunts and it is congruent with the findings of the previous studies.
Birth weight under 2.5 Kg, the presence of the symptomatic heart failure, surgery after the age of 6 months, and low caloric intake are considered risk factors for the malnutrition (33). Our findings have shown that the lower birth weight is associated with all types of growth impairment, with all range of the severity. Previous studies stated that younger age at the time of surgery has a positive effect on nutritional recovery (33-35). Delayed corrective surgery is considered to be a risk factor for growth failure and malnutrition (10), but according to a study by Vaidyanathan et al., malnutrition existed in 27% of the patients even after the early surgery. They also stated that significant improvement in nutritional status on short term follow-up is achieved by the corrective surgery; furthermore, children under five years old are more sensitive to the impact of malnutrition (36, 37). In our study, the age range was 0.03 - 176 months, mostly (89.3%) under five years old, which is a vulnerable group. The surgery is usually postponed because of the overwhelming load of the patients related to the equipment; this is the probable reason for the mean age of 23.52 ± 29.38.
All types of malnutrition, especially severe forms increase the mortality risk (7). Recurrent hospitalization, poor surgical outcomes, and persistent somatic growth failure are other complications of malnutrition in patients with CHD (38, 39). On the other hand, prolonged and recurrent hospitalization worsens the nutritional status (40). Previous studies have found that growth failure in early childhood is related to delayed mental development, poor school performance, and reduced intellectual abilities (8). Based on our findings, generally, severe malnutrition causes prolonged ICU stay following the surgery, and by detail, moderate and severe immediate and severe chronic malnutrition lead to a more protracted ICU stay.
According to a study done by Okoromah et al., the presence of the heart failure, type of cardiac defect, duration of the symptoms, age of under 5 years, and poor dietary fat intake are the possible predictors of malnutrition (30). In our study, the high prevalence of the malnutrition and related complications during and after surgical repair showed the importance of nutritional support and interventions in patients with CHD.