1. Background
The first years of life are the most important developmental period of the child. Therefore, the child’s nutrition during this period plays a significant role in his performance in later years (1). According to World Health Organization (WHO) reports, it is recommended that all children should exclusively breastfeed for the first six months of life. Some studies in industrialized countries have shown a shorter breastfeeding period than 6 months increases the risk of common infectious diseases such as respiratory and digestive infections (2). The positive effect of breastfeeding on both the mother and the child is already proven (3). Breastfeeding is the most ideal type of nutrition during the first 6 months of life and covers all the nutritional needs of the child including vitamins and minerals (4). It is associated with a reduced rate of gastrointestinal and respiratory infections (5).
The studies performed have shown that exclusive breastfeeding has been associated with lower mortality and morbidity (6). In Iran, reports have mentioned that the prevalence of exclusive breastfeeding at six months was only 28% (7). Due to the significant positive impact breastfeeding on child growth, an immediate effort is needed to establish an effective program to promote exclusive breastfeeding (8). The duration of breastfeeding is influenced by several factors, such as: mother’s age and education, nipple problems, contraceptive method and place of residence (city or village), which can be taken into consideration (9, 10).
Different studies have shown that the most important factors associated with the reduction in exclusive breastfeeding in the first 6 months of life are socio-economic factors such as mother’s age, mother’s occupation, mother’s level of education and the child’s rank among the siblings (11). Since then, different levels of intervention have been designed to emphasize on exclusive breastfeeding both in health centers and at the community level.
2. Objectives
Since breastfeeding in different societies can be affected by various personal, social and economic factors, given the lack of a research background on this important population-based issue and the necessity of examining it in different situations, the present study was performed aimed at investigating the status of exclusive breastfeeding at the age of 6 months and its related factors in the covered population by Mashhad University of Medical Sciences (MUMS).
3. Methods
This case-control study was performed in 2017 in the covered population by Mashhad University of Medical Sciences. This article has been written with code of ethics IR.MUMS.REC.1396.361. The required data were extracted from the Sina Health Record System (SinaEHR) supervised by MUMS. The recorded information in this system includes the health records of each child. In this study, all children who did not have exclusive breastfeeding during the first 6 months of life were considered as the case group. In total, 61397 children were studied (8130 children in case group and 53266 children in control group). The control group was almost five times larger than the study group. In this study exclusive breastfeeding, based on the WHO recommendation, has been considered since the first day of birth. If the baby has only received breast milk without water or any solid food, it will be accepted as exclusive breastfeeding. The dependent variable in this study was exclusive breastfeeding in the two categories (yes/no). The probable predictive factors were mother’s age, occupation, education, residential area, type of delivery, infant’s sex, weight, height and head circumference (HC), rank of the child among siblings, the presence of hypothyroidism in the infant, diabetes, hypertension or hyperlipidemia in the mother, mental or behavioral disorders in mother, breastfeeding at night and the number of breastfeeding times during 24 hours by the mother.
Data was entered into the SPSS software, Ver 15. In order to determine the study variables were used descriptive statistics. Gayatri logistic regression was applied to specify the factors affecting in exclusive breastfeeding. Variables with a probability value less than 0.2 were included in the bivariate analysis as compared to multivariate analysis to control for possible effect. Adjusted odds ratios with 95% confidence interval were used to assess the degree of dependency and probability less than 5% to report the statistical effect on the dependent variable in multivariate analysis.
4. Results
Among the 61397 children studied at the age of 6 months, 51.2% (31437 cases) were male. 86.6% (53266 cases) had exclusive breastfeeding, whereas 13.3% did not have exclusive breastfeeding ((breast milk and synthetic milk) = 50%; synthetic milk = 46%; (breast milk and livestock milk) = 1.7%; livestock milk = 1.1% and (breast milk, synthetic milk and livestock milk) = 1.2%)). The mean weight of the infants at birth was 3.18 ± 0.51 Kg and their mean height and head circumference were 49.82 ± 2.81 cm and 34.59 ± 1.82 cm, respectively.
The mean age of mothers in our study was 29.18 ± 6.13 and over two-thirds of the mothers (81.2%) were between 18 and 35 years old. Most cases (98.7%) were healthy mothers without; diabetes, hypertension, mental and behavioral disorders, hyperlipidemia and obesity, 92.5% were housewives and 38.9% had an under-diploma degree. Among the studied cases 75.6% lived in the cities and 24.4% in the rural areas.
Of the 61397 studied cases, exclusive breastfeeding had stopped in 1779 infants from birth to 6 m of age; 1087 cases due to inadequacy of breast milk, 22 cases due to the mother’s illness, 108 cases due to the infant’s illness and 364 cases due to the mother’s reluctance. Among the 5802 infants who had consumed synthetic milk, 3667 infants (63%) had done so due to the physician’s prescription, 113 infants (1.9%) because of the acquaintance recommendation, 1583 infants (27.3%) arbitrarily and in 439 infants (7.8%) due to other reasons.
The first model of multivariate logistic regression analyses was done by inserting variables such as residential area, rank of the child among siblings, weight, height and head circumference at birth and type of delivery. By considering the fit to test model, a lower chance of non-exclusive breastfeeding was achieved in the rural areas compared to the cities. Moreover, cesarean section (CS) increased the chance of non-exclusive breastfeeding by 2.01 times. The birth weight, height and HC also increased the rate of non-exclusive breast feeding a bit less than the average (Table 1).
| Variable | Univariate Model | Multivariate Model | ||
|---|---|---|---|---|
| Crude Odd Ratio (CI = 95%) | P Value | Adjusted Odd Ratio (CI = 95%) | P Value | |
| Sex | ||||
| Female | 0.97 (0.93 - 1.02) | 0.327 | ||
| Male | - | - | ||
| Location | ||||
| Rural | 0.55 (0.52 - 0.59) | 0.0001 | 0.44 (0.30 - 0.64) | 0.0001 |
| Urban | - | - | ||
| Birth rank | ||||
| First | 1.28 (1.11 - 1.48) | 0.001 | 1.17 (0.80 - 1.73) | 0.403 |
| Second | 0.97 (0.83 - 1.12) | 0.68 | 0.72 (0.48 - 1.1) | 0.131 |
| ≥ third | - | - | ||
| Birth weight, Kg | ||||
| < 2.5 | 5.64 (5.19 - 6.14) | 0.0001 | 2.37 (1.45 - 3.86) | 0.001 |
| 2.5 - 4.5 | - | - | ||
| > 4.5 | 1.06 (0.62 - 1.79) | 0.83 | 1.55 (0.28 - 8.47) | 0.609 |
| Birth HC, cm | ||||
| < 32.5 | 3.37 (3.05 - 3.72) | 0.0001 | 1.84 (1.11 - 3.06) | 0.018 |
| 32.5 - 37 | - | - | ||
| > 37 | 0.89 (0.69 - 1.16) | 0.42 | 0.76 (0.30 - 1.92) | 0.572 |
| Birth height, cm | ||||
| < 45 | 4.88 (4.44 - 5.37) | 0.0001 | 1.91 (-0.93 - 3.92) | 0.075 |
| 45 - 55 | - | - | ||
| > 55 | 0.56 (0.42 - 0.75) | 0.0001 | 0.92 (0.18 - 4.52) | 0.921 |
| Delivery site | ||||
| Home or others | 0.86 (0.6 - 1.22) | 0.40 | ||
| Hospital | - | - | ||
| Type of delivery | ||||
| CS | 2.01 (1.91 - 2.11) | 0.0001 | 2.00 (1.45 - 2.75) | 0.0001 |
| NVD | - | - | ||
| Hypothyroidism | ||||
| No | - | - | ||
| Yes | 0.87 (0.37 - 2.04) | 0.756 | ||
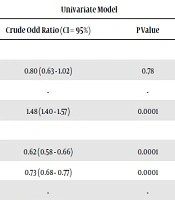
In the second model, multivariate logistic regression analyses for variables related to the mother, who was significantly associated with the breastfeeding status, were entered into the model. With increasing maternal age, the chance of non-exclusive breastfeeding increased. The same result was obtained for the mother’s level of education, in which this chance was 58% less in working mothers. In mothers who did not breastfeed their children at night, exclusive breastfeeding rate increased 2.48 times. Also, by reducing the number of breastfeeding times during 24 hours the possibility of non-specific breastfeeding increased (Table 2).
| Variable | Univariate Model | Multivariate Model | ||
|---|---|---|---|---|
| Crude Odd Ratio (CI = 95%) | P Value | Adjusted Odd Ratio (CI = 95%) | P Value | |
| Age, y | ||||
| < 18 | 0.80 (0.63 - 1.02) | 0.78 | 1.13 (0.79 - 1.63) | 0.489 |
| 18 - 35 | - | - | ||
| > 35 | 1.48 (1.40 - 1.57) | 0.0001 | 1.59 (1.44 - 1.75) | 0.0001 |
| Education | ||||
| Under diploma | 0.62 (0.58 - 0.66) | 0.0001 | 0.63 (0.57 - 0.69) | 0.0001 |
| Diploma | 0.73 (0.68 - 0.77) | 0.0001 | 0.72 (0.65 - 0.81) | 0.0001 |
| University degree | - | - | ||
| Occupation | ||||
| Housewife | - | - | ||
| Employed | 1.58 (1.42 - 1.75) | 0.0001 | 1.31 (1.12 - 1.46) | 0.0001 |
| Diabetes | ||||
| No | - | - | ||
| Yes | 1.14 (0.39 - 3.29) | 0.810 | ||
| HTN | ||||
| No | - | - | ||
| Yes | 1.11 (0.67 - 1.83) | 0.675 | ||
| HLP | ||||
| No | - | - | ||
| Yes | 1.38 (0.79 - 2.41) | 0.252 | ||
| Obesity | ||||
| No | - | - | ||
| Yes | 1.12 (0.71 - 1.77) | 0.606 | ||
| Mental and behavioral disorder | ||||
| No | - | - | ||
| Yes | 1.50 (1.19 - 1.90) | 0.001 | 1.46 (0.96 - 2.21) | 0.72 |
| Lactation at night | ||||
| No | 2.48 (2.00 - 3.09) | 0.0001 | 1.99 (1.48 - 2.69) | 0.0001 |
| Yes | - | - | ||
| Lactation in 24 hrs | ||||
| < 10 | 36.75 (19.01 - 72.05) | 0.0001 | 47.31 (19.57 - 114.35) | 0.0001 |
| 10 - 20 | 4.39 (2.27 - 8.49) | 0.0001 | 6.02 (2.49 - 14.55) | 0.0001 |
| > 20 | - | - | ||
5. Discussion
In the present study, the prevalence of exclusive breastfeeding and its predictive factors in children with an age of 6 months who were referred to the health centers affiliated to MUMS during one year was studied. The results showed that 86.8% of 6-month-old children were exclusively breastfed. Jones et al. (12) did a study called “Factors Associated with Exclusive Breastfeeding in the United States”. In this study, 25197 children were studied. The results of their study showed that 16.8% of infants were breastfed. Setegn et al. (13) conducted a study to identify factors predicting exclusive breastfeeding among mothers in the Bale Goba district, south east Ethiopia. In this study a total of 608 mothers were selected randomly. The results showed that 71.3% of infants were breastfed. Also, Tan (14) in a study showed that only 54.2% of children studied were breastfed. In Iranian cities, exclusive breastfeeding has a rate of 72.4% in Mashhad (15), 69% in Zahedan (16) and 66.4% in rural areas of Northern Iran (17).
In this research among all the studied variables, factors such as the residential area, rank of the child among siblings, weight, height and HC at birth, type of delivery, maternal age, mother’s educational status, mother’s occupation, presence of a mental or behavioral disorder, breastfeeding at night and the number of breastfeeding in 24 hrs were significantly associated with non-exclusive breastfeeding.
However, eventually and based on the logistic regression analyses, the following variables were associated with non-exclusive breastfeeding in the studied cases: rural versus urban residential area, cesarean section versus normal vaginal delivery (NVD), HC less than average versus an average HC, birth height less than average versus average height and birth weight less than average versus average weight, age over 35 years versus 18 - 35 years, under diploma and diploma degree versus university education, housewife versus employee, no breastfeeding at night and less than 20 times breastfeeding in 24 hrs versus over 20 times breastfeeding. In the present study, the relationship between the residential area and exclusive breastfeeding was significant; this result is consistent with a study performed in the northwest of Ethiopia (18).
When comparing cesarean section to NVD, the rate of non-exclusive breastfeeding increased significantly, this is consistent with the results of similar studies in Iran (19, 20).
As the results of this study show, the mother’s age at breastfeeding is one of the factors that are inversely related to exclusive breastfeeding. During the last 10 years, this pattern (increased maternal age and decreased breastfeeding) has been repeated in the reports from Iran and other countries, becoming stronger by the passage of time (21, 22).
As the results of this study clarify, the mother’s age at breastfeeding is one of the factors that is inversely related to exclusive breastfeeding. The possibility of exclusive nutrition with breastfeeding to mothers of 30 years and lower is more than others. Sanjari et al. conducted a study entitled “The Relationship Between Demographic Factors, Healthy Family and Social Health with Exclusive Breastfeeding in Women Referred to Kashan Hospital of Jaroff in 2014”. In this study, 375 women referred to the hospital were evaluated. The results of their study also showed that the possibility of exclusive nutrition with breastfeeding to mothers of 30 years and lower is more than others (23, 24).
Furthermore, a significant association was found between breastfeeding failure and the mother’s occupation. The main cause for failure and formula initiation was the mother’s return to work. The results of the study by Jalahi et al. (25) on 462 mothers also showed that a working mother was one of the causes of using artificial milk in children under 6 months. In addition, the results of the study by Merten et al. (26) and Li et al. (27) on 3032 and 212 mothers respectively, showed a significant relationship between mother employment and non-exclusive breastfeeding.
The other important finding was the significant association between the mother’s educational level and breastfeeding failure. Accordingly, the failure of nutrition with breast milk in mothers with a higher educational level was significantly more than others. The results of the study by Mosenzadeh et al. were matched with our study (20).
In the present study, a meaningful relationship was found between the presence of mental and behavioral disorders in the mothers of 6-month-old infants and non-exclusive breastfeeding; Sanjari et al. conducted a study to investigate the relationship between demographic factors, healthy family and social health with exclusive breastfeeding. In this study, 375 mothers were studied. The results of this study also showed that mental health in mother had a significant relationship with exclusive breastfeeding (24).
5.1. Conclusions
Taken together, it can be concluded that the rate of exclusive breastfeeding in the population covered by MUMS is similar to the recommended rate by the WHO (90%). Global nutritional policies are always looking for solutions to increase the amount of breastfeeding and its continuity. The findings of this study can be quite beneficial in diagnosing the mothers at risk of early discontinuation of breastfeeding. Regarding the modifiability of factors affecting breastfeeding such as care and monitoring of breastfeeding in the mother and encouraging them to breastfeed throughout the night, it can help maintain exclusive breastfeeding and its continuity.
One of the strong aspects of this study was the application of records of over 61000 infants which can be a true representative of exclusive breastfeeding in the population covered by MUMS. Given the study limitations, the errors made in filling the forms in the system can be mentioned. Supervising the correct registration of data in the electronic file and settings of the electronic form in such a way to avoid possible errors made by users in the recording of information is highly recommended for future research.