1. Background
Preterm delivery (before 37 weeks of gestation) includes 5% - 15% of childbirths worldwide (1-3). A significant percentage of infant and neonatal mortality and morbidity is related to premature babies. Problems related to prematurity consists of respiratory, nutritional, neurodevelopmental, and gastrointestinal complications involving these patients from the time of delivery and hospital admission to the post-discharge duration at home. There is a crucial need for special care of preterm infants in neonatal intensive care units (NICUs), as well as in post-discharge periods (4-6). The best outcomes of these patients are obtained by continuing the follow-up of their medical problems at special follow-up clinics. Regarding the need for following up on multiple problems of premature infants by multidisciplinary and sophisticated teams, usual health centers affiliated to the Health Ministry are not suitable for these complicated follow-ups (7). The special consideration of additive care and follow-ups for preterm neonates compared to term babies is done at high-risk neonatal follow-up clinics (HRNFCs).
The HRFNCs are multidisciplinary clinics for the detection and management of problems in different fields such as nutritional, growth/developmental, neurological, hearing, visual, and rehabilitation aspects in preterm babies from early post-discharge periods to months or years after the discharge (8, 9). On the other hand, obtaining information about long-term morbidity of high-risk neonates at follow-up clinics can be helpful for the appropriate changing of standard care of these patients to achieve a better prognosis. At HRNFCs, parental training for better care of their children can be an important factor for the decline of long-term consequences of preterm delivery (7, 10). The American Academy of Pediatrics (AAP) suggested that the discharge planning of premature babies needs to contain six essential components including the education of parents, assessments of unresolved medical problems, performance of primary care, planning for home care, mobilization and identification of support services, and surveillance and designation of follow-up clinics (11).
2. Objectives
Considering the importance of post-discharge care and follow-up of preterm babies, we planned a study to investigate long-term and post-discharge medical problems of preterm babies delivered at our maternity hospital and admitted to our NICU.
3. Methods
The present study is a prospective descriptive study focusing on preterm infants delivered from 2016 to 2017 at Mahdieh Maternity Hospital. The inclusion criteria included all premature neonates with a gestational age of less than 34 weeks and birth weight of less than 2000 g admitted to the NICU of the hospital because of prematurity and low birth weight from among those who were alive at the time of discharge to home. The exclusion criteria included dead neonates or those transferred to another hospital with no follow-up at the HRNFC. The Ethics Committee of Shahid Beheshti University of Medical Sciences approved the study and written consent was taken from the parents of patients.
Based on the policy of the care of preterm neonates in our hospital, all patients were referred to the HRNFC after discharge from the NICU to visit and follow-up their main problems. As mentioned, all preterm neonates that had at least one visit to our HRNFC were enrolled in the study. The timing of the first post-discharge visit was determined by the attending neonatologist or special nurse of the neonate. The first visit was done usually 2 - 3 days post-discharge. The frequency of outpatient visiting was weekly for all patients with a discharge weight of lower than 2,000 g, two weekly for infants weighing 2,000 - 3,000 g, and monthly for infants weighing higher than 3,000 g. Due to the lack of access to patients, in spite of suggestions to parents for the regular referral of their neonates to the HRNFC, the timing of follow-up visits was different for all infants. Regarding the importance of the growth pattern of preterm infants, we measured body weight, head circumference, and height of the neonates at all visits and the pattern of growth was assessed based on the special curve for preterm babies.
The hearing screening was done by auditory brainstem response (ABR) at centers out of the hospital, but the visual examination was done at our clinic by an expert ophthalmologist at retinopathy of prematurity (ROP). For infants with pallor detected in the physical examination, cell blood count (CBC) was checked. For neonates with hemoglobin and hematocrit levels of lower than 7 mg/dL and 21 mg/dL, respectively, despite the intake of a full dose of iron supplement, readmission in the neonatal ward was planned for packed cell transfusion.
By interviewing the mothers, the problems related to nutrition, consisting of the selection of the milk consumed, methods, frequency, and volumes of feeding, and the lactation technique, were checked and instructions were presented to the mothers, if needed. For babies with feeding intolerance, instructions were presented for changing the formula.
The vaccination and repeated screening for hypothyroidism were checked based on the protocols of the Health Ministry. Other possible problems of infants such as surgical problems, infantile colic, allergic symptoms, and gastroesophageal reflux were evaluated and managed. For all infants with spasticity detected by the physician or physiotherapist, rehabilitation and physiotherapy were done at special clinics of our hospital. Ultrasound of the brain, pelvis, and kidneys was done for all patients in the radiologic ward of the hospital, except for infants with a prolonged hospital stay or a previous normal finding of recent sonography. Developmental assessment by a special scoring system was not done at our HRFNC and for suspected cases with gross developmental delay, referral to a pediatric neurologist was done. Demographic data and anthropometric indices of the patients and all information about the mentioned issues were recorded, as well.
The collected data were analyzed by SPSS version 23 software. For the analysis of quantitative variables, we used the mean and standard deviation and for qualitative variables and multivariate analysis, a regression test was used. P < 0.05 was considered significant.
4. Results
Based on the demographic data collected from 140 neonates, 72 (51.4%) neonates were male and 68 (48.6%) were female. The mean gestational age of the neonates was 30 weeks with a standard deviation of 2.36. The lowest gestational age was 24 weeks. Table 1 shows the number of patients at different gestational ages. The mean birth weight of the neonates was 1,366.99 g with a standard deviation of 37.37. The lowest weight was 630 g and the highest weight was 1,990 g. Table 1 shows the number of patients in different birth weight groups. The average length of stay of the patients in the NICU was 34.6 (5 - 140) days. The mean interval between the discharge and the referral time to the clinic was 6.16 days with a range of 1 to 45 days. The frequency of visits at the clinic is shown in Table 1. The number of visits to the HRNFC at post-neonatal ages (after one month of life) is shown in Table 1. As can be seen, the number of visits to the HRNFC decreased with the increase in the age of patients and just 33 (23.5%) patients referred to the clinic at the ages of three and six months.
| Variables | Values |
|---|---|
| Gestational age, weeks of gestation | |
| < 28 | 35 (25) |
| 28 - 32 | 81 (57.9) |
| > 32 | 24 (17.1) |
| Birth weight, g | |
| < 1000 | 23 (16.4) |
| 1000 - 1500 | 61 (43.6) |
| 1500 - 2000 | 56 (40) |
| Number of visits to HRNFC | |
| One time, the lowest | 14 (10) |
| 18 times, the highest | 2 (1.4) |
| ≥ 8 times | 35 (25) |
| Number of visits to HRNFC at post-neonatal ages, mo | |
| 3 | 60 (42.8) |
| 6 | 55 (39.2) |
| 12 | 14 (10) |
| Nutrition | |
| Exclusive breast milk | 24 (17.1) |
| Formula and breast milk | 75 (53.6) |
| Exclusive formula | 41 (29.3) |
aValues are expressed as No. (%).
The nutrition selection of the patients is shown in Table 1. Unfortunately, the number of exclusively breastfed infants was lower than the number of infants fed with formula. Among formula-fed infants, 97 (69.3%) cases were fed with preterm formula in the first few weeks after discharge and 5 (6.3%) cases were fed with Post-Discharge Formula (PDF). In the absence of the PDF availability, after gaining the bodyweight of 3 - 3.5 kg, the regular formula for term babies was recommended.
The results of the one-year follow-up of infants indicated that the rate of readmission was 26.4% (n = 37). Infantile colic, gastroesophageal reflux, and respiratory allergy were reported in 35 (25%), 31 (22.1%), and 5 (3.6%) cases, respectively, and 9 (6.4%) cases needed surgical intervention for inguinal hernia. Prolonged Jaundice requiring readmission for phototherapy was detected in 10 (1.7%) infants and cholestasis was observed in one case.
All newborns received the full vaccination as per the standard protocols and had a screening for hypothyroidism by filter papers at the age of 3 - 5, 14, 42, and 70 days of life, based on the protocols of screening by the Health Ministry. In 4 (2.9%) patients, hypothyroidism was detected and levothyroxine was administered for treatment.
Brain sonography was done in all 140 (100%) eligible neonates before and after discharge and 122 (86.3%) neonates had normal findings. Hydrocephaly and periventricular leukomalacia (PVL) were diagnosed in 11 (7.9%) and 4 (2.9%) neonates.
Echocardiography as a modality for the assessment of cardiac disorders was done in neonates with abnormal findings in the physical examination favoring cardiac dysfunction or in patients with previous abnormal echocardiography. In our patients, 3 (2.1%) neonates had Patent Ductus Arteriosus (PDA) with no patients needing surgical closure of PDA. In 5 (3.6%) neonates, other cardiac anomalies were recorded such as ASD and tetralogy of Fallot.
All preterm neonates admitted to the NICU were examined by ophthalmologists for retinopathy of prematurity (ROP) at the age of 4 weeks and repeated ophthalmologic examination was planned based on the maturity of retinal vascularity and suggestion of our ophthalmologist. After discharge from the hospital, all preterm infants had repeated exam for the diagnosis of ROP. Vascularization of the retina in 47 (33.6%) infants were completely normal while the others had some degrees of the immaturity of retinal vascularity which needed repeated examination and 10 (17.1%) infants had severe abnormality needing treatments such as intra-retinal injection of Avastin or laser therapy for prevention of blindness.
Based on the policy of our ward, all the neonates admitted to the neonatal ward and NICU should have hearing screening by otoacoustic emission (OAE), but because of the inaccessibility of ABR, as the main tool for the assessment of hearing loss in preterm infants, the hearing assessment was planned after discharge from the hospital. Unfortunately, just 42 (30%) patients underwent this accurate evaluation, showing 39 (92.8%) normal findings and 3 (7.1%) abnormal hearing findings.
For the screening of hip dislocation, 85 (60.8%) neonates underwent a hip ultrasound at the ages of 4 - 6 weeks of life or later. Of them, 74 (87%) cases had normal hip and 11 (12.9%) cases had abnormal alpha (lower than 60 degrees) and beta angles related to type 1A hip dislocation. In the follow-up of patients with probable hip dislocation, after a suggestion to parents for appropriate positioning of their neonates’ hips, repeated hip sonography showed that all patients had normal hips.
Based on the reported discharge sheets of patients, 64 (45.7%) neonates underwent pre-discharge hemoglobin evaluation and 37 (26.4%) cases had mild anemia (hemoglobin < 10 mg/dL) without the need for packed cell transfusion (before discharge) but after discharge, despite nutritional supplementation with iron, 66 (47.1%) neonates had still anemia, 28 (20%) of whom had severe anemia (hemoglobin < 7 mg/dL) in need of readmission for packed cell transfusion.
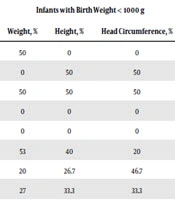
All growth indices of the patients (birth weight, head circumference, and height) at birth are listed in Table 2. Based on the birth weight of our patients, infantile growth indices in the first, third, and sixth months of life are presented in Table 3.
| Percentile, % | Weight Number, % | Height Number, % | Head Circumference Number, % |
|---|---|---|---|
| 3 | 21 (15) | 30 (21.6) | 16 (11.55) |
| 10 | 43 (30.7) | 34 (24) | 42 (30.2) |
| 50 | 59 (42.1) | 50 (36) | 52 (37.4) |
| 90 | 16 (11.4) | 21(15) | 26 (18.7) |
| 97 | 1 (0.7) | 3 (2.2) | 2 (1.4) |
aValues are expressed as No. (%).
| Percentile, % | Infants with Birth Weight < 1000 g | Infants with Birth Weight 1000 - 1500 g | Infants with Birth Weight 1500 - 2000 g | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Weight, % | Height, % | Head Circumference, % | Weight, % | Height, % | Head Circumference, % | Weight, % | Height, % | Head Circumference, % | |
| First Month of Life | |||||||||
| 3 | 50 | 0 | 0 | 68.4 | 36.8 | 21.1 | 32.4 | 14.7 | 5.9 |
| 10 | 0 | 50 | 50 | 15.8 | 42.2 | 52.6 | 38.2 | 29.4 | 41.2 |
| 50 | 50 | 50 | 50 | 15.8 | 21 | 15.8 | 36.5 | 53.3 | 44.1 |
| 90 | 0 | 0 | 0 | 0 | 0 | 0 | 2.9 | 17.6 | 5.9 |
| 97 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2.9 | 2.9 |
| 3rd Month of Life | |||||||||
| 3 | 53 | 40 | 20 | 13.6 | 13.6 | 4.8 | 4.3 | 4.3 | 0 |
| 10 | 20 | 26.7 | 46.7 | 18.2 | 13.6 | 38.1 | 8.7 | 4.3 | 30.4 |
| 50 | 27 | 33.3 | 33.3 | 54.5 | 54.5 | 42.9 | 56.2 | 60.9 | 39.1 |
| 90 | 0 | 0 | 0 | 13.6 | 18.2 | 14.3 | 17.4 | 21.7 | 26.1 |
| 97 | 0 | 0 | 0 | 0 | 0 | 0 | 4.3 | 8.7 | 4.3 |
| 6th Month of Life | |||||||||
| 3 | 33.3 | 33.3 | 46.7 | 11.1 | 11.1 | 5.6 | 4.5 | 0 | 4.5 |
| 10 | 26.7 | 6.7 | 20 | 22.2 | 11.1 | 38.9 | 22.7 | 4.5 | 4.5 |
| 50 | 20 | 46.7 | 33.3 | 50 | 55.6 | 38.9 | 22.7 | 45.5 | 63.6 |
| 90 | 20 | 13.3 | 0 | 11.1 | 16.7 | 11.1 | 36.4 | 27.3 | 9.1 |
| 97 | 0 | 0 | 0 | 5.6 | 5.6 | 5.6 | 13.6 | 22.7 | 18.2 |
5. Discussion
Despite increasing the survival of premature neonates over the past few decades, the complications of prematurity still account for the main problems of the health system (12). Long-term morbidity of preterm infants requires multidisciplinary follow-ups for the prevention of delayed complications of prematurity or following the present involvements of them for better outcomes of these high-risk infants (8, 9). The establishment of special multidisciplinary clinics for preterm babies needs a team consisting of neonatologists, ophthalmologists, pediatric neurologists, physical therapists, audiologists, and nutritionists for following the main problems of them in each area for the prevention or treatment of long-term morbidities (7, 13, 14).
The purpose of this study was to evaluate the post-discharge follow-up of preterm babies admitted to our NICU. A total of 140 premature infants were followed up for two years after discharge. According to the findings of this study, 25% of the newborns had more than eight visits, which shows desirable conditions. Unfortunately, 10% had just one visit to our clinic, which can be an alarm for the healthcare system to assess the causes of parents’ reluctance to bring their babies to clinics with the probability of missing their problems. Regarding the absence of a regionalization system for care at Iranian maternity hospitals, the place of residence of some patients in our NICU was far from our hospital and regular outpatient visiting of infants was not possible for parents.
The longest time interval of follow-up was 36 months observed just in one case. As mentioned in Table 1, 60 (42.8%) patients had visited at their three months of life, 55 (39.2%) at six months of life, and 14 (10%) at one-year-old; therefore, it seems that the number of visits to our clinic decreased with increasing the age of patients. It is possible that due to the reduction of their specific problems over time, the continuing of their outpatient care was done at other general centers near to their residence locations.
Based on the growth indices at birth in our population, the most values of birth weight, height, and head circumference were at the 50th percentile of growth charts; that is, 42.1% of neonate birth weights, 36% of neonate heights, and 37.4% of neonate head circumferences were at the 50th percentile of growth charts. This issue indicates that due to good prenatal care of mothers, the number of premature infants appropriate for gestational age (AGA) was higher than growth retardation. In a study in Taiwan that was done in 2007 - 2011, Tsai et al. reported that AGA preterm infant delivery at birth was more than SGA (65 % vs. 33.2%) (15).
Although the number of our neonates with AGA at birth was remarkable, the rate of growth impairments was significant after discharge from the hospital, particularly in extremely low birth weight infants (ELBW) with birth weight of less than 1000 g (n = 23 infants) so that at the age of one month, 50% of the infants were at the 50th percentile of weight while at the age of three months, 53% of the infants’ weight and 40% of the infants’ height were at the third percentile. Thus, this result indicates some degrees of growth impairment in these high-risk patients at a few months post-discharge. The justifying reasons for this issue can be the nutritional-related problems of these patients, such as the selection of milk, lack of proper lactation technique, use of unfortified breast milk, feeding with regular formula instead of a specific post-discharge formula for preterm infants, and gastrointestinal problems. However, at the age of six months, the number of patients at the third weight percentile decreased and 20% of the patients were at the 90th percentile of weight.
Based on our results, a better condition was observed in neonates with a birth weight of 1,000 to 1,500 g. Moreover, 54.5% by the age of three months and 50% at the age of six months were at the 50th weight percentile of the growth curve. In infants with a birth weight of more than 1,500 g, the rate of increasing birth weight was more appropriate than in the neonates with lower-birth weight. Thus, ELBW infants needed more attention to the nutritional state. Our results are consistent with the results of a study by Modi et al. that showed weight, height, and head circumferences of newborns at 12 months of age increased compared to their birth time, but they had lower mean scores than term neonates (16).
The findings of our study indicated that 17.1% of the infants at the time of discharge were exclusively breastfeeding; 53.6% were fed with breast milk and formula simultaneously and 29.3% were fed exclusively by the formula. Despite the emphasis on the exclusive breastfeeding for all infants, especially preterm babies, nearly 83% of our infants did not feed exclusively by their breasts of mothers. Similar to our result, in a study by Rodrigues et al., 91% of newborns were non-exclusively breastfed (17). In a study by Lee and Jang (18) in 2016, exclusive breastfeeding in premature newborns from the first week to 12th week of life and breastfeeding concurrent with formula increased from 5.7% to 19.8% and from 27.3% to 67.9%, respectively. Breastfeeding with formula at the same time decreased from 67% to 12.3%. However, the increase in nutrition with formula was much higher than the increase in breastfeeding (18).
Given that 11 (7.9%) hydrocephalus, 4 (2.9%) PVL, and 3 (2.1%) GMH patients were reported in our study, it seems that the investigation of neurological and developmental prematurity-induced complications is highly important and has a significant role in the healing of these patients. In Tsai et al. study in Taiwan, the rate of PVL was 0.33% at GA 30 - 32 weeks, 1.19 % at GA 27 - 29 weeks, and 0.77 at GA 24 - 26 weeks (15).
One of the most important problems of prematurity is anemia. Prolonged hospitalization, lots of blood sampling, and the low levels of erythropoietin and iron storage of preterm infants are the leading causes of this problem before and after discharge from the hospital. The lack of attention to anemia can adversely affect the weight gain of infants or their neurological developments (19). In the present study, 47.1% of the neonates had post-discharge anemia and 20% of them required blood transfusions. Based on these results, it seems that the prevalence of post-discharge anemia is significantly high in premature infants. Therefore, paying more attention to the proper nutrition of premature infants and the use of food supplements, such as appropriate doses of iron drops, may prevent severe anemia and its consequences. These results are in line with the results of Domellof and Sjostrom’s study in 2015, in which 40% of preterm infants needed oral iron supplements after discharge from the hospital (20).
In the present study, 37 (26.4%) infants had a history of re-admission to the hospital because of intensified jaundice (requiring phototherapy), respiratory distress, and the need for hernia repair surgery. Considering that all neonates in this study were premature with low birth weight, it seems that this number is acceptable.
According to Underwood et al. (21) study, approximately 15% of premature infants needed at least one hospitalization during their first year of life, with the highest prevalence being in neonates with the gestational age of fewer than 25 weeks. The most common cause of re-admission was acute respiratory diseases (21).
One of the complications of prematurity is delayed hypothyroidism that can be detected in repeated screening tests. In the present study, delayed hypothyroidism requiring treatment with levothyroxine was detected in 2.9% of the neonates. In the study by Armanian et al., transient hypothyroidism was the most common endocrine problem in neonates with a prevalence of 33.33% (22).
One of the common problems of premature infants after discharge from the hospital is developmental delay and motor skill problems. In this study, 16.4% of newborns needed treatment with physical therapy. However, we did not use a standard assessment tool for the developmental evaluation of our patients, but based on routine physical examinations of the patients at the HRNFC or the reports of their parents, referring to a pediatric neurologist was suggested in cases with diagnosed or suspected developmental delay. Glass et al. (6) in 2015 reported high rates of neurodevelopmental abnormalities in preterm infants despite significant changes in the care of them. They also mentioned no improvement in the neurodevelopmental outcomes of preterm infants even though the incidence of some neurosensory impairments had been decreased (6).
A limitation of our study was the discordance of the time of visits of patients to the HRNFC. This irregularity in the interval of visiting our patients made the statistical analysis difficult and probably has caused inaccurate results of growth chart indices. Another limitation was the lack of planned neurodevelopmental assessments in our patients.
5.1. Conclusions
According to the results of this study, the follow-up of premature infants after discharge from the hospital is necessary by an expert multidisciplinary team. Growth and developmental problems, especially in neonates with birth weights of less than 1000 g, seem to be more important than in those with higher birth weights and as a result, more nutritional care is needed in this specific birth weight group. Considering the low percentage of exclusive breastfeeding in premature infants, comprehensive planning to increase the rate of breastfeeding by mothers of preterm neonates is very crucial. Due to the high prevalence of anemia and the need for blood transfusion after discharge from the hospital, proper nutrition with milk and dietary supplements is necessary to prevent anemia and blood transfusion. Developmental assessment of discharged premature infants should be taken into account in the outpatient care program after discharge from the hospital.