1. Background
Computerized provider order entry (CPOE) systems are electronic versions that end-users can registration orders into a computer application rather than use paper records (1) also ensure standardized, legible, and complete orders (2-4). Technologically, CPOE is discussed nearly half a century (5). Until 2009, CPOE was available in less than 20% of US hospitals (6-8). In 2012, majority of hospitals use CPOE for variety tests (9). While the results of searching show that the only one public hospital in Iran uses CPOE just for prescribing (10).
One of the main aspects that can determine the success of implementation of CPOE is providers’ satisfaction. We know that providers have a crucial role in CPOE development. They could affect the success of the implementation of CPOE (11). Several studies examined the impact of CPOE implementation on providers’ performance (12-14). In 2003, almost all of the providers were dissatisfied with newly installed CPOE (15). Most studies show that providers’ resistance is a great obstacle to implement CPOE (16, 17) while other studies reported that providers have a willingness to use CPOE and believed with CPOE usability, efficiency, workflow, and patient safety (18, 19).
One of the most popular adoption models for understanding how CPOE innovation between providers is the diffusion of innovations theory and understanding how CPOE innovation accepts between providers (20-22). To increase the scientific value and generalizability this research, Rogers’ innovation diffusion theory was used to analyze the impact of factors on the nursing staff attitudes toward the acceptance or rejection of the CPOE. A CPOE technology’s relative advantage, compatibility, trialability, and observability generally lead to a faster rate of adoption, while increased complexity leads to a lower rate of adoption.
2. Objectives
The views and attitudes of nursing staff are essential on the usefulness and ease of use of a CPOE. Since nursing staff are one of the main users of CPOE, in this study, we set out to examine factors that may influence CPOE adoption among nurses in a large healthcare organization. The diffusion of innovation theory was used to understand nurses’ attitudes and thoughts about implementation and use of the CPOE system.
3. Methods
This cross-sectional study was conducted in Urmia City, North West of Iran, in 2017. Four teaching hospitals were in this region: 450-bed Emam Khomeini, 205-bed Motahari, 153-bed Seyedoshohada and 218-bed Taleghani. All nurses working in hospitals were included in data collection. The major factors influencing nursing staff’s acceptance and use of the CPOE system were examined through Rogers’ innovation diffusion theory.
3.1. Research Instrument
We used the multi-section questionnaire of Rahimi et al. that has been tested for reliability and validity in a previous study (23). The language of the questionnaire was Persian. The responses were in Likert scale format (strongly agree, agree, neutral, disagree, strongly disagree). The questionnaire was included: nursing staff' demographic information (12 questions), survey the level of computer literacy of the nursing staff (7 questions), survey the level of CPOE literacy of the nursing staff (4 questions), survey the attitude of nursing staff about the effectiveness of CPOE (21 questions (relative advantages (12 questions) and compatibility (9 questions))), survey the attitude of nursing staff of the complexity arising from the implementation of CPOE (8 questions), and survey the attitude of nursing staff regarding the technology necessary for the implementation of CPOE (8 questions). Statistical analysis was performed with SPSS Version 16.0
4. Results
4.1. Demographic Variables
Table 1 describes the research population. A total of 273 questionnaires were distributed among the nursing staff. The results showed that 177 nursing staff (64.84%) completed the questionnaire. Approximately, the number of female participants (n = 94, 53.1%) was higher than the number of male participants (n = 83, 46.9%), and most of them were young with an average age of 34.97 ± 5.85 years.
| Characteristics | No. (%) |
|---|---|
| Sex | |
| Men | 83 (46.9) |
| Women | 94 (53.1) |
| Age groups (y) | |
| 20 - 29 | 63 (35.6) |
| 30 - 39 | 54 (30.5) |
| 40 - 49 | 46 (26) |
| 50 - 59 | 14 (7.9) |
4.2. The Level of Computer Literacy
The questions and responses are listed in Table 2. Generally, the level of nursing staff’s computer literacy was high (71.32%). Respondents indicated that a large number of nursing staff download scientific contents from the internet (n = 171, use email (n = 89), also to work on the PC while at the workplace (n = 140).
| Questions | Strongly Disagree | Disagree | No Comment | Agree | Strongly Agree |
|---|---|---|---|---|---|
| Office skills | 5.6 | 9.7 | 60.7 | 20.2 | 3.7 |
| Work on the PC at workplace | 8.6 | 13.9 | 31.5 | 37.5 | 8.6 |
| Ability to install the software | 8.6 | 18 | 46.8 | 21.7 | 4.9 |
| Use Email | 38.6 | 38 | 0 | 102 | 24 |
| Download book and scientific contents from the internet | 4.1 | 0.4 | 47.9 | 34.8 | 12.7 |
| Advantages of using computers in the healthcare | 4.1 | 18 | 55.8 | 18 | 4.1 |
| Computer ability to facilitate daily tasks | 3.7 | 17.2 | 39 | 27 | 13.1 |
4.3. Nursing Staff Satisfaction
The collected data showed that just 26% of the nursing staff was aware of the CPOE system. Also we found that the compatibility, relative advantages, and complexity of the CPOE were 71.94%, 66.29% and 40.36%.
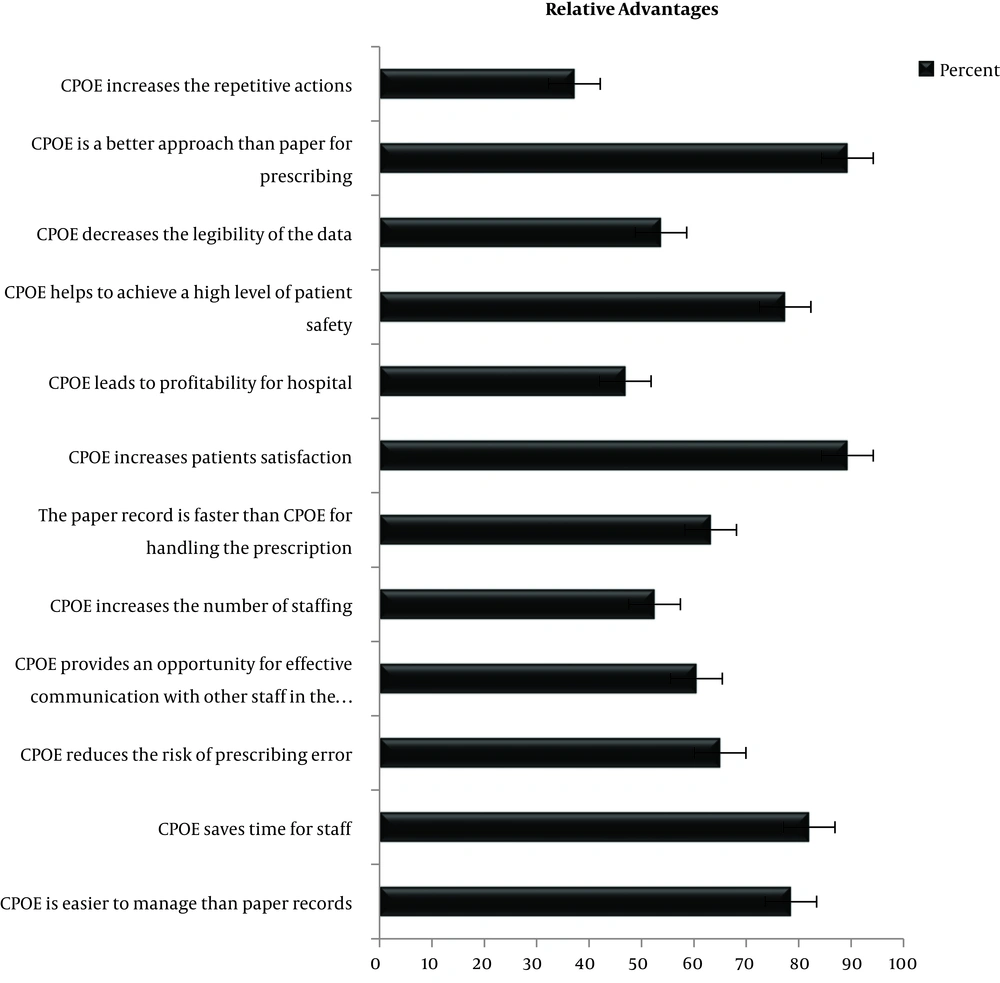
4.3.1. Level of the View of Nursing Staff About the Relative Advantages of CPOE
In the present study, the received relative advantages of the CPOE was high (66.29%). In advantages section from Figure 1, it can be seen that a lower percentage of the nursing staff agreed that the CPOE is faster to handle than the paper-based system (36.8%) whereas the vast majority respondents (78.5%) agreed that system is easier to manage than paper records and an up percentage of the nursing staff (82%) agreed that the system will save time for staff.
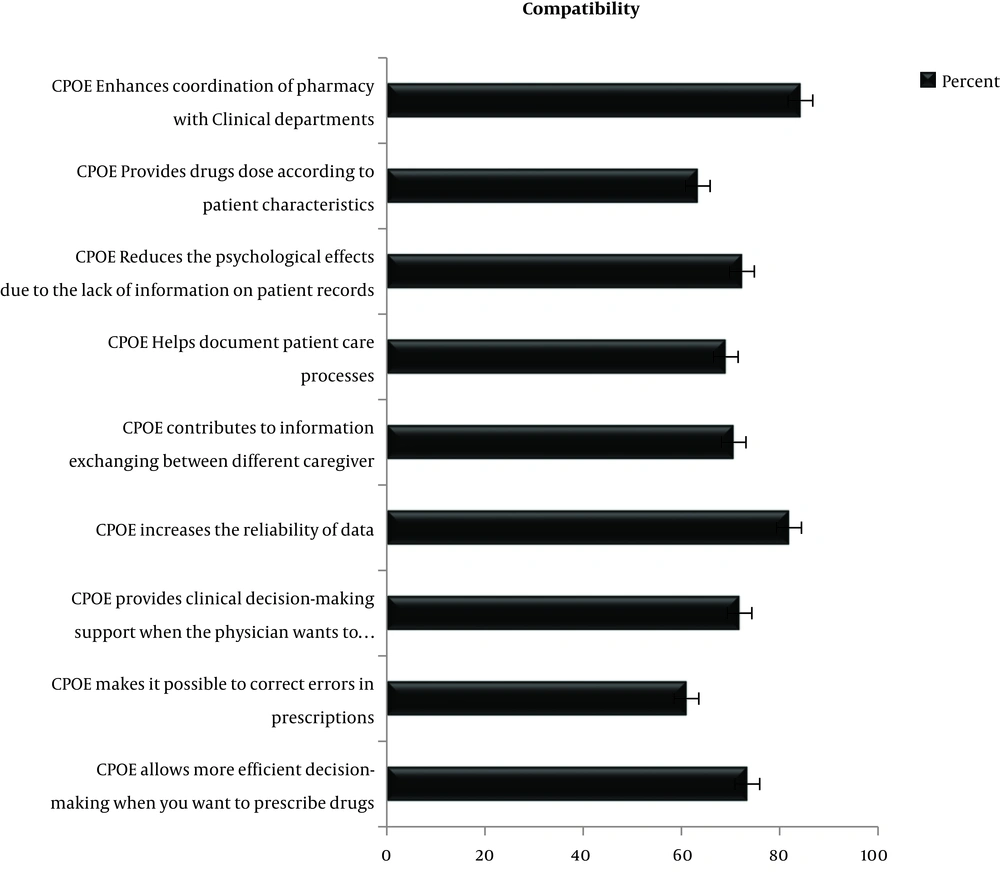
4.3.2. Level of the View of the Nursing Staff About the Compatibility of CPOE
In this study, we found that the compatibility of the CPOE was 71.94%. In the compatibility section from Figure 2, it can be seen that the CPOE will be more effective than the paper-based system. For example, when physicians prescribe drugs, the system can be more effective (73.4%). Findings show that 72.3% of the nursing staff agreed that the CPOE Reduces the missing of information on patient records.
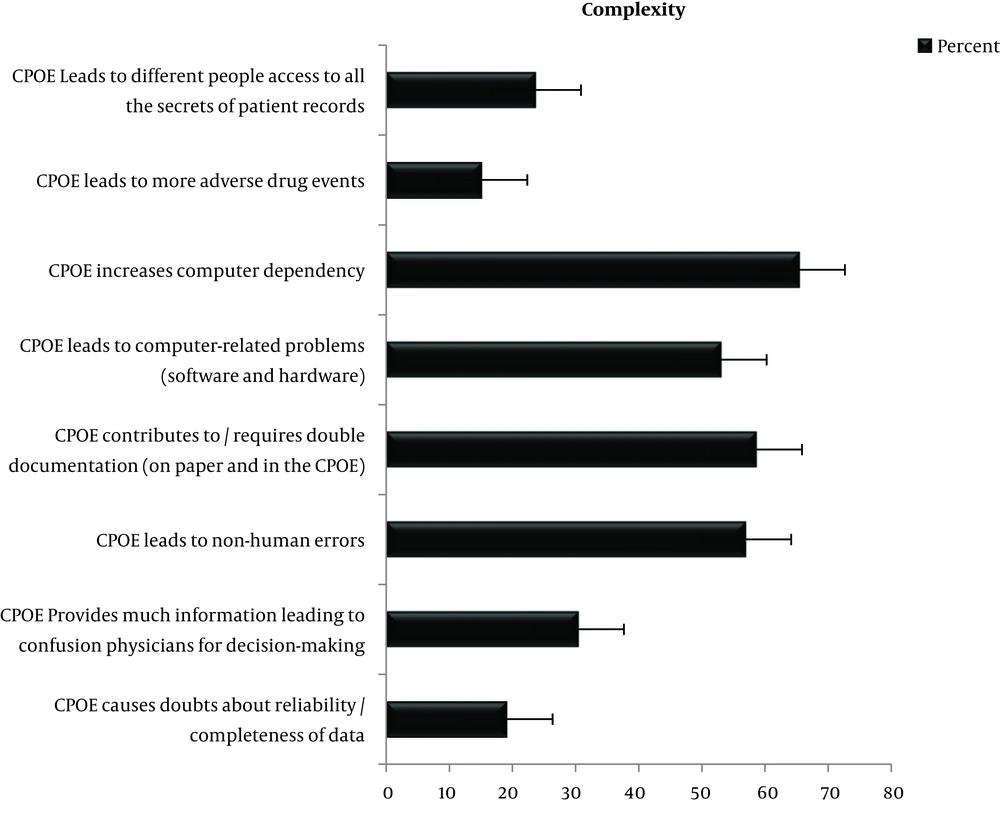
4.3.3. The Level of the View of the Nursing Staff About the Complexity of CPOE
In this study, we found that the complexity of the CPOE was 40.36%. In complexity section from Figure 3, it can be seen that a minority of the nursing staff (19.2%) stated that the CPOE system will increase doubts about completeness and reliability of data. In addition, 53.1% of the nursing staff stated that the CPOE system can lead to computer problems (software and hardware).
4.4. Comparison of the View of the Nursing Staff About the Innovation of CPOE with Gender, Age, Educational Level, Experience of Using the HIS System and Computer Literacy
CPOE implementation in male nursing staff was acceptable. The findings showed that the relative advantages, compatibility and complexity among male and females nursing staff were almost equal (gender section from Table 3). Their viewpoint about the relative advantages, compatibility was high and complexity was low (P > 0.05).
| Attributions of the Diffusion of Innovation Theory | Relative Advantages | Compatibility | Complexity |
|---|---|---|---|
| Gender | |||
| Men | 60.84 ± 6.96 | 61.06 ± 7.01 | 36.01 ± 4.88 |
| Women | 59.96 ± 5.94 | 67.29 ± 5.88 | 34.57 ± 4.77 |
| Age groups (y) | |||
| 22 - 32 | 40.18 ± 6.28 | 40.3 ± 6.3 | 21.84 ± 4.89 |
| 33 - 42 | 34.1 ± 6.53 | 30.42 ± 6.7 | 25.83 ± 4.72 |
| > 43 | 35.72 ± 6.77 | 26.53 ± 6.46 | 20.55 ± 4.85 |
| Degree of education | |||
| Associate’s degree | 30.5 ± 5.52 | 20.42 ± 5.41 | 26.5 ± 3.6 |
| Bachelor’s degree | 30.08 ± 6.37 | 20.57 ± 6.32 | 25.27 ± 5.04 |
| Master’s degree | 31.1 ± 7.06 | 20.75 ± 7.32 | 26.32 ± 4.75 |
| Phd’s degree | 31.86 ± 9.46 | 23.14 ± 9.79 | 28.71 ± 5.09 |
| Experience with the HIS system (mo) | |||
| NO | 30.06 ± 5.93 | 20.39 ± 5.69 | 25.48 ± 4.83 |
| < 1 | 28.78 ± 3.96 | 19.13 ± 2.48 | 25 ± 3.42 |
| 2 - 6 | 31.92 ± 8.35 | 21.77 ± 8.95 | 28.03 ± 4.66 |
| 6 - 12 | 31.95 ± 8.63 | 22.45 ± 9.3 | 25.23 ± 6.32 |
| > 12 | 30.31 ± 5.74 | 20.58 ± 5.67 | 25.77 ± 4.64 |
aValues are expressed as mean ± SD.
Older nursing staff also accepted CPOE implementation hardly (age section from Table 3). Since young nursing staff use technology more often, then they also welcome CPOE. However, older nurses were also more likely to agree that relative advantages of CPOE are high (P > 0.05).
The findings showed that the degree of education has the same effect on the recognition of Relative advantages, Compatibility and Complexity of the CPOE system (degree of education section from Table 3). Although nurses with a baccalaureate degree and more had better computer literacy, the educational level did not affect CPOE acceptance (P > 0.05).
5. Discussion
All of the organizations and individuals are interested to change (24). The present study has demonstrated that understanding the nursing staff’s computer literacy and their attitude and satisfaction can be effective in accepting and the implementation of a CPOE system. Although prescribing is done by the physicians, our study examines nursing staff satisfaction with CPOE. The results of this study show that to how extent nursing staff agree with the use of computers in the workplace and the implementation of CPOE.
Generally, the level of nursing staff’s computer literacy was high. Approximately, half of the nursing staff reported that they use computers in the workplace. Our results demonstrate the associations between nursing staff’s view computers with age, educational level, and experience with the HIS system. Our study found that age was small in the nursing staff’s computer literacy. Similarly, as with other studies reported this to be very small or nonexistent (25, 26).
Since the level of nursing staff’s computer literacy was high, it is expected that they would easily accept CPOE. The findings indicated that the educational level did not affect CPOE acceptance. Likewise, Khajouei’s study revealed that there was no significant relationship between nurses’ satisfaction and educational level (27). However, evidence shows that gradual acquisition of the skills through training could effectively increase users’ satisfaction (28). Young nursing staff accepted CPOE implementation more easily.
Often, studies have shown that CPOE provision of just-in-time feedback to physicians when they want to prescribe drugs (29-31). In our study, most of the nursing staff believe that CPOE makes it possible to correct errors at the moment of prescription. Correct errors at the moment of prescription increase patient satisfaction that one finding in our study demonstrated that approximately all nursing staff thought CPOE increases patient satisfaction.
Another important finding of this study was that approximately half of the nursing staff agreed about increasing prescription legibility. Also study Foster and Antonelli on CPOE showed the same opinion (32). They believe that the advantages of CPOE include order legibility, improved response time, reduction in adverse drug reactions, and improved patient outcomes.
This study has several limitations. First, this study was limited to the perception of innovation attributes such as relative advantage, compatibility and complexity and other studies could be carried out to include other factors such as trialability and observability. Second, the number of the participating nursing staff was also low.
Despite these limitations, this study has identified a factor that could have an impact on the users’ high satisfaction. Results of this study emphasize the importance of training programs that aim at improving computer literacy among nursing staff and ultimately would increase their levels of satisfaction with the system and increase productivity with ease.