1. Context
Cardiovascular disease (CVD) as the leading cause of death is significantly increased due to lifestyle changes. Aging and inadequate physical activity led to impaired fluid balance and impaired function of the cardiovascular system (1). Decreased cardiac function as a result of our sedentary lifestyle along with other risk factors such as aging, high blood pressure, and malnutrition are closely related to early-onset heart attacks (2). Etiologically, developed country reported cardiovascular diseases as the most frequent cause of death in their countries (3), and statistics attributed 30% of deaths worldwide to cardiovascular disease. The United States reported 633,842 deaths from heart disease in 2015 (4). Heart failure (HF), one of the most common cardiovascular diseases, increases with age and threatens the life of HF sufferers (5). The cost of treatment is high and burdens the patients. Hence, effective implementation of self-care programs can reduce the cost of treatment and control severe complications of the disease. However, due to the complexity of these care protocols, people with low health literacy (HL) are more susceptible to HF complications and their treatment and quality of life are adversely affected (6).
One can define the health-related quality of life (HRQol) as own perceptions of a patient and characterize it by patient assessment of the effects of a disease and its consequences on his or her life (7). Health-related quality of life is a multidimensional concept covering physical, mental, and, social health and therefore represents an individual’s overall health (8). Health-related quality of life is an imperative figure when controlling incessant, dynamic, and complex illnesses and it incorporates the patient’s encounter with the illness (7). Lower HRQoL is often experienced after heart disease (9). Also, clinicians should consider HRQoL as an essential step, when they are managing and treating patients with chronic HF (10). Patients with HF deal with more complications compared to patients of the same age without chronic illness and other conditions; thus, an assessment of HRQL in these patients is required to predict the future risk of mortality (10).
Treatment adherence is one of the necessities that HF sufferers should pay attention to. Treatment adherence is composed of adhering to medication intake, maintaining a healthy diet, and to according lifestyle changes with health guidelines. The patients who are adherent to their treatment demonstrated milder presentations of disease and had a lower rate of hospitalization (11). Whereas, non-adherence to treatment increases hospitalization by one-third and adds to the mortality rate in the HF population (12). Literature addressed that more than 50% of the HF population fails to use their medication and follow treatment regimens. This is still one of the main challenges demanding interventions to improve patients’ adherence to treatment (11).
Health literacy is a fundamental component in the development of a well-being state that humans should possess to get better well-being results (13). Health literacy for the most part incorporates the information, inspiration, and capacity of people in the utilization of well-being data to create judgments and choices in preserving an infection or moving forward to improve quality of life (14). The World Health Organization has introduced HL as one of the main factors influencing health (15). Health literacy alludes to the capacity of people in processing wellbeing information and administering the situations on create suitable well-being choices (16).
Self-efficacy is characterized by one’s belief in the own abilities to promote and maintain health. A study has shown that cardiac disease patients with higher self-efficacy had better sleep and quality of life (17). Whereas, poor self-efficacy reduced psychological well-being in the HF population and worsened their quality of life (18). Self-efficacy also mediates the implementation of self-care in patients with depression. In other words, poor self-efficacy is associated with depressive symptoms and hopelessness and can worsen the clinical condition of the HF population (19).
We observed remarkable progress in various aspects of management of patients with cardiovascular diseases such as in the prevention, diagnosis, treatment, and rehabilitation, by which mortality from these diseases has been significantly reduced. However, CVDs still play a major role in the number of deaths. Considering the noteworthy burden of heart infection, enhancing the knowledge of well-being in people can offer an unequivocal contribution to the treatment and spare assets (15). Many people with cardiovascular disease are unaware of their illness and consider its symptoms to be signs of aging. Nevertheless, these symptoms eventually affect their functioning in daily life (15). This lack of awareness can be attributed to low HL. Improving HL can be an effective strategy for promoting health status and utilizing health services. On the other hand, the availability of cost-effective educational programs to increase HL can reduce the prevalence of heart disease and minimize the economic burden to the patient and society (15). The purpose of this systematic review is to examine research literature exploring the impact of self-efficacy and HL on medication adherence and HRQoL in patients with HF.
2. Evidence Acquisition
2.1. Search Strategy and Resources
This systematic review study is based on PRISMA 2020 guidelines (20). PubMed, Scopus, and Web of Science databases were reviewed for related articles. The search was performed on July 5, ,2022 using the keywords of “self-efficacy” or “health literacy” or “health education” and “adherence to medication” or “medication adherence” or “quality of life” or “quality of health” and “heart failure” or “heart compensation”. Additional articles were also searched in the Google search engine, using the keywords “self-efficacy” or “health literacy” and “heart failure”.
2.2. Inclusion and Exclusion Criteria
Articles were approved if they met any of the specified criteria. Articles that provided evidence about the effect of HL in HF patients on their treatment adherence and their quality of life were selected. There were no restrictions on the type of study, and all interventional or observational studies were reviewed. Also, the articles examining self-efficacy and its effect on adherence to treatment and quality of life published between 1999 and 2022 were all included. We restricted the review on publication since 1999 because the concept of HL was first introduced in 1999 (21). The exclusion criteria disqualified the review of non-research articles and articles that did not assess HL and self-efficacy in people with HF.
2.3. Study Selection
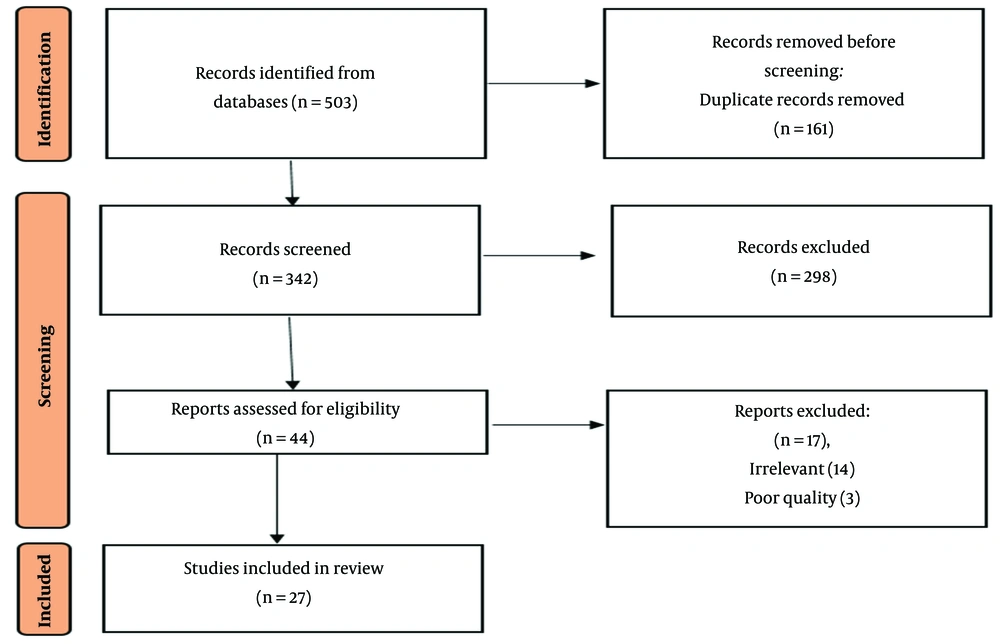
After collecting the articles, an author primarily reviewed the titles and excluded any articles that did not meet the inclusion requirements. The two authors then independently reviewed the abstract of the remaining studies. At this stage, only eligible articles approved by both authors were included. Afterwards, the two authors thoroughly reviewed the remaining articles. In case of disagreement between the two authors, the article was reviewed by the third author and then selection occurred by the majority of votes. Figure 1 describes the selection process for each study at each stage.
2.4. Quality Assessment
The quality of the articles was evaluated using guidelines of the Agency for Healthcare Research and Quality (AHRQ) (22). Two authors were asked to evaluate each study in terms of method and measurement, study design, use of appropriate statistical methods and consideration of confounding factors. In case of disagreement between the two authors, the opinion of the third author was inquired to assure the quality.
Following the search process, 503 possibly related articles were identified and their bibliographic information was transferred to Endnote reference management software. Of these, 161 were duplicates and were therefore eliminated. In the screening phase, out of the remaining 342 studies, 298 articles were deleted after applying the inclusion and exclusion criteria in articles’ title and their abstracts. In the eligibility stage and quality assessment, 24 unrelated articles out of the remaining 44 studies were removed after reading their full text based on inclusion and exclusion criteria. Finally, 27 articles were systematically reviewed.
2.5. Data Extraction
The data were extracted using standardized forms. This information included the first author, year of study, place of study, type of study, demographic characteristics, aim the of study, utilized tools and results of studies.
3. Results
Appendix 1 in the Supplementary File provides general information of the studies reviewed. The study populations were patients with HF and these studies were conducted between 2005 and 2020. From a total of 27 approved studies, 1 was conducted in Brazil (5), 1 in Serbia (23), 1 in Korea (24), 1 in the Netherlands (25), 1 in Italy (26), 1 in Iran (27), 1 in Singapore (17), and 1 in Taiwan (28). Other studies (19, 29-46) were conducted in the United States. The smallest number of participants in this review belongs to the study of Murray et al. and Barnason et al. with 44 patients (31, 45), while the largest number of participants belongs to the study of McNaughton et al. with 705 patients (34). A gender distribution with a minimum number of male participants (20.5%) was observed in the study of Murray et al. (31), whereas the maximum number of male participants (75.5%) was observed in the study of Tung et al. (28). Except for 2 studies in Asia (24, 28) in which all participants were of Asian descent, other studies indicated that the majority of participants were African American (30, 31, 36, 37, 39). Other studies reported the ethnicity of the participants separately, and most of the participants were white (5, 29, 32-35, 39-42).
Among the studies, five were cohorts (29, 31, 33, 34, 44). One of these studies (31) investigated the factors associated with exacerbation of clinical symptoms and reduced quality of life in patients with HF. Two studies (29, 34) examined the relationship between HL and mortality and the factors influencing hospitalization. In another study, the effect of self-efficacy on medication adherence and patients’ quality of life was measured (44). The latest study (33) also examined the effect of HL on adherence to medication and treatment. Thirteen studies (5, 17, 19, 23-25, 28, 32, 35, 36, 40, 41) were cross-sectional. In some studies, only the effect of HL on various factors influencing the quality of life was investigated (23, 28, 32, 35, 36). In addition to this, some other studies assessed the effect of HL on adherence to treatment (5, 24, 36, 40, 41). Another descriptive comparative study examined the effect of HL on quality of life, self-care and hospital stay (39). Three other studies (38, 42, 43) that were randomized clinical trials examined the effect of self-care education in HF patients on their treatment adherence and their quality of life. In 7 studies, the effect of self-efficacy on quality of life and adherent medication was investigated (17, 19, 25-27, 45, 46). Lastly, 1 post hoc analysis study (30) was performed on a randomized controlled clinical trial and ascertained the effect of pharmacological education by a pharmacologist on adherence to treatment, HL, and the quality of life of people with HF (Appendix 1 in the Supplementary File).
The prevalence of inadequate and marginal HL was also examined in a number of studies. The test of functional HL in adult (TOFHLA) was the most common used questionnaire in many studies (31, 32, 35, 36, 39, 41, 42). According to these studies, the prevalence of low HL ranged from 19.2% to 61%. This indicates that majority of these patients has inadequate HL. Moreover, another study (37) showed 47.9% had low levels of HL, using TOFHLA. The study by Jovanic et al. (23) reported the highest prevalence of poor HL, which assessed its patients via the European Health Literacy Questionnaire. This questionnaire examines the perception, availability, evaluation and implementation of health information in patients. Tung et al. (28) also found a high prevalence of inadequate HL. Their results obtained from Taiwan Health Literacy Scale (THLS) questionnaire showed that 60% of HF patients in Taiwan had poor HL.
In general, all studies have shown that HF patients with adequate HL and self-care have a positive effect on medication adherence. In a study by Murray et al. (31), it was found that poor HL tripled the risk of the non-adherence. Murray et al. reported that their HF patients with low levels of HL had been correlated with poor quality of life (31). Improved medication adherence in relation to sufficient HL was further observed in other studies (30, 33, 40, 41). The study by Como (40) stated that adequate HL has a bilateral positive effect on self-efficacy and mental health of individuals, and this improvement in mental health increases the adherence to treatment in patients with HF. Another study (33) found that higher literacy levels had reduced the likelihood of non-adherence to treatment in patients with HF (OR, 0.84; 95% CI, 0.74-0.9).
Good HL also enhances the quality of life of people with HF. The report obtained from RCT studies indicates that interventions of teaching health principles and self-care to patients has improved patients’ quality of life (38, 42). DeWalt et al. (38) stated that increasing the number of training sessions increases the patients’ knowledge over hear failure, which finally improves the quality of life. Other studies (36, 39, 41) also confirmed these findings and disclosed the positive and significant correlation between self-care and HF knowledge, that ultimately led to improvements in patients’ quality of life. Another study (24) showed the effect of high levels of HL on seeking social supports and practicing self-care. A positive effect was observed in all aspects of quality of life. High levels of HL were found to improve mental and physical states in these patients (23).
The impact of HL on mortality and hospitalization of HF patients was also assessed. In fact, patients with poor HL have higher mortality rates. Peterson et al. (29) reported a significant increase in risk of mortality in patients with inadequate HL. This result was also supported in another study (5). The length of hospital stay tend to prolong and recovery is less expected in patients with poor HL (28, 34).
The present review also examined the role of self-efficacy in quality of life and adherence to treatment. Overall, self-efficacy has a significant prediction from quality of life and medication adherence. Several studies in this area (27, 43, 45) have shown that enhancements in self-efficacy made patients to more willingly follow their treatment, and lead to experience of higher quality of life, and lower hospitalization rates among the HF population. An association between higher rates comorbidity has been found with low self-efficacy in patients (26). Diabetes patients with comorbid HF have also confirmed the effective and positive role of self-efficacy in their quality of life (46). Only one study did not find a statistical significance effect of self-efficacy on improved health status (17). But other studies emphasized the positive and significant effect of self-efficacy on the lives of patients with HF (19, 25, 27, 44).
4. Discussion
Readmission and mortality rates in patients with HF may be only expected when adequate health education programs are available for growing number of HF patients. Improving drug adherence in patients with chronic disease, especially HF, demands a variety of interventions (30). To offer an individualized treatment plan with best efficacy, each patient’s literacy about his/her health should be assessed carefully, and then strategies of health education should be adjusted based on patients’ levels of HL (5). Heart failure is not the only disease in which patients’ knowledge about the disease has positively correlated with HL, and a positive correlation between these two has been also addressed for many other diseases as well (41).
High self-confidence plays an important role in managing symptoms and maintaining individual functioning. Studies show that quality of life can be predicted by the level of self-efficacy. It is found that patients who took care of themselves alone had a better quality of life than patients who are dependent to their families or guardians. In fact, the ability of a person to perform his personal duties increases the patient’s sense of control over life and affects its quality (47).
It can also be said that since self-efficacy determines how a person responds to life’s challenges; the higher the levels of self-efficacy, the greater ability to adapt and the higher medication adherence (48). On the other hand, self-efficacy is known as a mediator between motivation and physical activity. Hence, it can act as an effective factor to motivate the HF patients for more physical activities, and thus induce a positive effect on the quality of life in these patients (49).
There is a link between HL and drug adherence (30, 36). Adherence rate varies based on the level of HL (30). In a study population of young African-American patients suffering from HF, Kumar et al. revealed 2 different aspects of HL: A direct positive relationship between patients’ education level with HL, and an inverse relationship between age and HL (36). Health literacy can also determine the beliefs of patients with a certain disease (23). Also, social support that an elderly patient receives and one’s HL positively have positively correlated with self-care behaviors that one practiced (24). In line with previous studies, study of older adults having education levels less than high school by Dennison et al. showed that practice of self-care behaviors and their knowledge about HF can be promoted by enhancing HL among these patients (39).
Nevertheless, individuals with low levels of education may not perceive the urgency for prompt medical at the early signs of the disease and delay the treatment, albeit no direct association was found between education level and the incidence of disease (5). The level of academic education of people and the years of their education can predict the level of HL, and the results shows that people with adequate literacy has studied more years in academic education (between 9 and 12 years) (5). This study showed (5) that the majority of members (68.0%) lacked sufficient HL. Inadequate HL is concerned to affect one’s health care measures in prevention of illnesses and in promotion of self-care. Also, inadequate HL is directly associated to one’s knowledge about disease and infection control (5). Health literacy education can have a positive impact on patients’ adherence to HF treatment, and it is better to use appropriate lexicon according to patients’ education level, visual communication and regular interactive sessions with patients with low HL (5). The highest percentage of drug adherence in previous study was attributed to adequacy of literacy, in which patients with sufficient levels of literacy had more adherence to drug therapy (88.1%) (5). On the other hand, patients with inadequate HL had more barriers to drug adherence, such as improper regimen (63.2%), wrong beliefs (22.1%) and grim reminders (52.9%) (5).
Nurses play an inevitable role in promoting the level of HL, particularly when patients are suffering from chronic disease including HF. Health literacy is closely bound with health status, and it improves the adherence to treatment and reduces the incidence of readmission and death in patients with HF (5). In addition to nurses, pharmacist intervention also contributes to promote the HL level and subsequently improves the drug adherence (30). This review acknowledged the significance of HL in fundamental knowledge of HF patients, and how HL alters the patients’ perception about their disease. Also, we tried out best to clarify the implication of educational programs designed to improve HL targeting HF patients in the clinical setting. We emphasize the implementation of these HL-sensitive interventions and their promising effects on drug adherence (30, 42, 50, 51). To improve patients’ HL and enhance social support, the instructions collected in systematic review can enlighten clinicians and health professionals to construct their own care interventions when dealing with HF cases.
4.1. Limitations
The primary limitation of this review is the widely-dispersed statistics, which made it impossible to perform a statistical meta-analysis. In another aspect, a large number of studies were cross-sectional, which makes it difficult to investigate the causality. Because the health systems in different countries differ in quality and strategy, it is not possible to generalize the results of this review to many countries. Also, only a few articles specifically studied self-care and the way it affects the HF patients’ quality of life, which limited us to provide a comprehensive and detailed explanations on this issue.