1. Background
In December 2019, a highly contagious disease caused by the new coronavirus appeared in Wuhan, China (1). On January 7, 2020, the coronavirus was identified as an emerging virus by the Chinese Center for Disease Control and Prevention (CDC) of a patient's throat swap sample by sequencing the whole genome, and on February 11, 2020, the WHO named it nCoV-2019 (1, 2). The WHO classified the disease a pandemic on March 11, 2020. The virus is the third epidemic of beta-coronavirus in the twenty-first century, resulting in a public health disaster and widespread alarm (3). SARS-CoV-2, like SARS-CoV and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV), is the seventh coronavirus with the ability to induce human infection. It attacks the lower respiratory tract. Other human coronaviruses (HCoV 229E, NL63, OC43, and HKU1), on the other hand, are responsible for colds and upper respiratory infections (4). The new coronavirus has a very high transmission capacity and varied mortality. Although all age groups were susceptible to the disease, some groups such as the elderly, people with an underlying health condition, chronic health conditions or weakened immune systems and pregnant women at greater risk of serious COVID-19 illness (5).
At the beginning of the COVID-19 pandemic in the world, the most common symptoms included fever, headache, lethargy, dry cough, and shortness of breath. A runny nose, sore throat, nasal congestion, and gastrointestinal pain or diarrhea may also be present in some patients. Although fever has been reported as the most common symptom of the disease, some patients with severe forms may also have low or even no fever (6).
Later, loss of olfactory was introduced as other symptoms of the disease. When compared to other symptoms in a logistic regression analysis, olfactory dysfunction is the most definitive indicator for predicting COVID-19 positivity, as Rocke acknowledged in a systematic review study (7). Some literatures have been reported upper airway involvement symptoms such as sore throat, nasal congestion and rhinorrhea (6, 8, 9).
Different respiratory viruses can cause infection simultaneously. Also the condition can be made worse by affecting some bacteria, especially in patients with immune system defects or chronic respiratory disease (10). More than 80% of COVID-19 patients had minor symptoms (11) or a fair prognosis, but some persons developed more serious problems, including as sepsis followed by multiple organ failure, acute respiratory distress syndrome, pulmonary edema, pneumonia, heart failure, and septic shock (8, 12).
On the other hand, about 18% of people, regardless of laboratory findings and CT scan, were asymptomatic but have the potential to transmit the virus (13, 14). Bilateral pulmonary parenchymal ground-glass and consolidative pulmonary opacities, occasionally with round morphology and peripheral lung distribution, were the most common radiographic symptoms of this disease (15-18). RT-PCR was the safest way to diagnose COVID-19 by sampling the nasal or pharyngeal mucosa, although its false-negative rate was high (19). If the test is negative, experts were recommended two RT-PCRs 3 days apart for a definitive diagnosis. However, limited test kits during the epidemic did not allow this. Chest CT scans were usually recommended in these cases.
Although CT had less specificity, it was more sensitive to RT-PCR (98% vs. 71%) (20, 21). However, using CT as the only diagnostic tool was not acceptable. Because, first, CT was not able to differentiate the symptoms of various viruses (22), second, about half of the patients in the early stages of the disease had normal CT (20). However, the benefits of using CT from the beginning were undeniable. Because it provides the possibility to assess the extent of the disease. So, helps to predict the need for ventilation and the diagnosis of pulmonary embolism, pulmonary edema and myocarditis in the advanced stages (23).
2. Objectives
Although months have passed since the end of the corona pandemic in most countries, the emergence of new strains from time to time in some parts of the world has not completely eliminated the danger of COVID-19 (10). Our purpose was to analyze the epidemiological, clinical and imaging features of patients with COVID-19 in Ahvaz, Khuzestan Province southern Iran.
3. Methods
This descriptive study took place in Ahvaz, the capital of Khuzestan province in southeastern Iran, from June to August 2020 (the first wave of the COVID-19 epidemic in Iran). The samples were collected from two hospitals Razi with of 200 beds and Sina with 250 beds in Ahvaz. Both hospitals were considered as reference hospitals for COVID-19 patients in Khuzestan province from the beginning of the outbreak of COVID-19. Both hospitals were affiliated with Ahvaz Jundishapur University of Medical Sciences (AJUMS). To collect data, first, study checklist was prepared based on the review of published articles about COVID-19, the guide of the Iranian Association of Radiologists on CT-scan reports of COVID-19 patients, COVID-19 registry system forms in Khuzestan province and consulting clinical specialists. The study checklist included patient demographics, referral date, abnormal chest X-ray and CT-scan findings, and imaging diagnosis. Second, the Health Information Management Department of Sina and Razi Hospitals obtained a list of all COVID-19 approved patients from March to May who underwent CT-scan and chest X-ray.
The inclusion criteria for the research samples included the following:
• Hospital admission (inpatient or outpatient)
• Positive PCR test
• CT scan procedure
• The presence of complete clinical information of the patient in the COVID-19 registry system
Therefore, non-hospital patients, suspected cases of COVID-19, patients without CT scans, and patients with incomplete clinical data were excluded from the study.
Third, the list of patients and the study checklist were given to two specialists (including a pulmonologist and a radiologist). All AJUMS affiliated hospitals in Ahvaz were linked to the integrated PACS system.
The relevant specialists were asked to retrieve images of patients and complete study checklists. Fourth, the signs and symptoms of the disease, underlying diseases and comorbidities, and treatment outcomes of the investigated patients were retrieved using data from the COVID-19 registration system in Khuzestan province. Then, these data were entered into SPSS statistical software version 22. Descriptive statistics including average, mean, in, max and frequency were used to analyze the data.
4. Results
This study included 375 approved COVID-19 patients with a mean age of 55.5 ± 18.6 with an age range of 11 to 94 years. Patients included 50.9% male and 49.1% female. The mean duration of stay in the hospital was 7.6 days. Due to the severity of the disease, 14.4% of patients were hospitalized to Intensive Care Units. 13.6 percent (51 individuals) of all hospitalized patients died. Diabetes (23.2 percent) and cardiovascular disease were the most common underlying diseases (21.9 percent). Cough (62.4 percent), dyspnea (57.1 percent), and fever were the most prevalent early symptoms among hospitalized patients (48.8 percent). Abdominal pain (0.3 percent) and hemoptysis were the most uncommon symptoms (1.1 percent). The oxygen saturation of the patients was also measured, and the results revealed that 18.9% (71 patients) had an oxygen saturation of less than 93 percent. Table 1 contains further information about the patients' epidemiological and clinical characteristics.
| Variables | No. (%) |
|---|---|
| Age, y | |
| ≤ 39 | 74 (19.7) |
| 40 - 49 | 64 (17.1) |
| 50 - 59 | 70 (18.7) |
| 60 - 69 | 74 (19.7) |
| ≥ 70 | 93 (24.8) |
| Sex | |
| Male | 191 (50.9) |
| Female | 184 (49.1) |
| Comorbid disease | |
| Hypertension | 8 (2.1) |
| Diabetes | 87 (23.2) |
| Cardiovascular disease | 82 (21.9) |
| Liver diseases | 5 (1.3) |
| Chronic obstructive pulmonary disease | 19 (5.1) |
| Chronic kidney disease | 22 (5.9) |
| Chronic neurological diseases | 10 (2.7) |
| Pregnancy | 5 (1.3) |
| Symptoms at onset of illness | |
| Fever | 183 (48.8) |
| Cough | 234 (62.4) |
| Dyspnea | 214 (57.1) |
| Chest pain | 19 (5.1) |
| Confusion | 19 (5.1) |
| Hemoptysis | 4 (1.1) |
| Sore throat | 29 (7.7) |
| Abdominal pain | 1 (0.3) |
| Diarrhea | 16 (4.3) |
| Nausea/vomiting | 57 (15.2) |
| Headache | 42 (11.2) |
| Anorexia | 23 (6.1) |
| Myalgia | 98 (26.1) |
| Pain joint | 20 (5.3) |
| General weakness | 12 (3.2) |
| Saturation of O2 < 93 | 71 (18.9) |
| Hospitalized in ICU | 54 (14.4) |
| Mechanical ventilation | 39 (10.4) |
| Final outcome | |
| Discharge | 324 (86.4) |
| Death | 51 (13.6) |
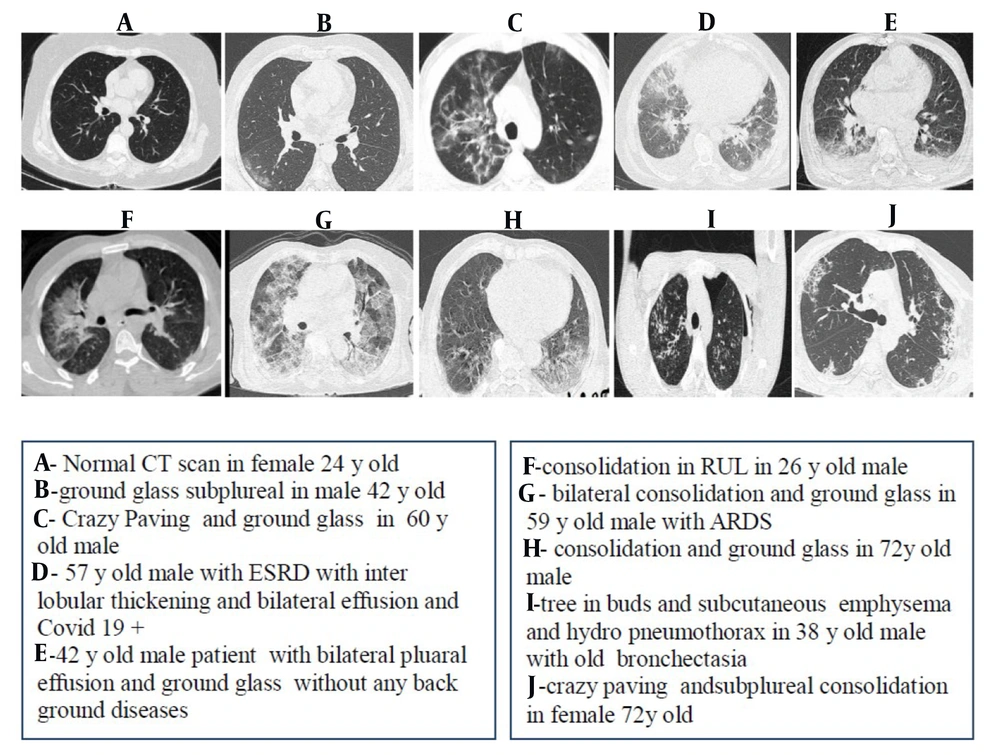
Radiological evaluations showed that 81.1% (304 patients) of CT scan patients were abnormal and 18.9% were normal. The most common pulmonary involvement manifestations were Ground-glass opacity (67.5%), Consolidation (47.5%), Crazy-paving (25.6%) and Pleural effusion (20.3%). Therarest pulmonary manifestations were Cavitation (2.1%) and Pneumothorax (2.1%). Also Sub pleural involvement was observed in 45.6% of patients. In terms of involvement, the majority of individuals had both lungs engaged (86.9 percent). In terms of Lobes involvement, most of the Lower Lobes (61.1%) were involved. Posterobasal engagement was the most common type of involvement (35.5 percent). Table 2 has further radiological information. Figure 1 also shows the CT findings of ten patients.
| Variables | No. (%) |
|---|---|
| Final results of CT scan | |
| Normal | 71 (18.9) |
| Non-normal | 304 (81.1) |
| Pulmonary involvement manifestation | |
| Ground-glass opacity (GGO) | 253 (67.5) |
| Branching nodular and linear opacities (Tree-in-bud sign) | 21 (5.6) |
| Crazy-paving | 96 (25.6) |
| Cavitation | 8 (2.1) |
| Pneumothorax | 8 (2.1) |
| Cardiomegaly | 42 (11.2) |
| Adenopathy | 4 (1.1) |
| Pleural effusion | 76 (20.3) |
| Atelectasis | 38 (10.1) |
| Consolidation | 58 (15.5) |
| Patchy | 106 (28.3) |
| Extension of involvement | |
| Right lung alone | 32 (8.5) |
| Left lung alone | 17 (4.5) |
| Both lungs | 326 (86.9) |
| Zonal involvement | |
| Upper lobes | 207 (55.2) |
| Middle lobes | 200 (53.3) |
| Lower lobes | 229 (61.1) |
| Site of involvement | |
| Sub pleural | 171 (45.6) |
| Anteroventral | 133 (35.5) |
| Central | 78 (20.8) |
| Posterobasal | 51 (13.6) |
5. Discussion
The spread of SARS-CoV-2 continues. In the last few months, significant progress has been made in monitoring the pathogen, accurately identifying, defining the various symptoms and clinical treatment. The number of sick men and women in this study was roughly equal, and the average age of the patients was 55 years. A diabetic diagnosis was found in 23.2 percent of patients, while cardiovascular disease was found in 21.9 percent. Other underlying diseases with a much lower percentage included chronic renal failure, hypertension, liver disease, and chronic nervous system disease. Most of the initial symptoms of patients including cough, shortness of breath and fever were estimated. Other clinical symptoms were myalgia, nausea and vomiting, headache, sore throat, anorexia, joint pain, chest pain, confusion, diarrhea, and Hemoptysis.
For the first time in Iran, on February 7, 2020, a 75-year-old man with symptoms of 38-degree fever, acute cough and shortness of breath, and bilateral lung involvement on CT scan was diagnosed with COVID-19 in the emergency department of a hospital in Qom. On February 10, it was tested positive by RT-PCR method and confirmed on February 19 by gene sequencing (24). Since then, diagnostic and follow-up proceedings have been taken more seriously in Iran. Shahriarirad et al. in a retrospective study by 113 confirmed COVID-19 hospitalized patients between February 20 and March 20 in Shiraz city conducted the first study on clinical data in Iran. Patients were on average 53.8 years old, with 62.8 percent of them being men. Fatigue (66.4 percent), cough (64.6 percent), and fever were the early signs of this illness (59.3 percent) (25). In another city in Iran, Tehran, with a relatively similar period (February 10 to March 30), Homayounieh et al. examined the clinical signs of 90 patients confirmed by RT-PCR in two groups of survivors and deceased. The majority of the patients were men, and the most common symptoms among survivors were fever (73 percent), cough (67 percent), shortness of breath (60 percent), and myalgia (42%), while the most common symptom among the deceased was shortness of breath (72 percent) (26). Our findings are consistent with other studies in Iran and the world. In research conducted by Zhou and colleagues in China on 191 COVID-19 patients aged 18 and older (135 from Jinyintan Hospital and 56 from Wuhan Pulmonary Hospital), 91 (48%) had underlying disease, with hypertension (30%), diabetes (19%), and coronary heart disease (8%) being the most prevalent (12). Similarly, in the Zhang study in Zhejiang Province from January 17 to February 8, the most reported symptoms included 85.9% fever, 68.4% cough, 36.3% Hemoptysis, 14% sore throat, and 11.3% headache, respectively (27). Also, in Europe, in Rome, Italy, in a study from March 4 to 19,2020 with 158 patients, 83 men and 75 women; Average age 57 years; fever in 97 cases (61%), cough and shortness of breath in 88 cases (56%) and 52 cases (33%) were reported as the most common symptoms, respectively (28).
In terms of radiological findings, 81.1 percent of the patients in our study had abnormal CT scan results. Ground-glass opacity, Consolidation, and Crazy-paving were the most prevalent pulmonary involvement manifestations. In 86.9% of patients, both lungs were involved. A very small percentage of patients showed involvement of one side of the lung. Regarding Zonal involvement, in most patients, the lower lobes were involved, and the involvement of the upper and middle lobes were more or less the same. Posterobasal involvement was also relatively significant in terms of site of involvement. Our CT findings are consistent with the findings of another research. In a Caruso's study in Rome, Italy, by analyzing CT scans of 58 patients who had positive RT-PCR results, stated that GGO was present in 100% of patients, with three patterns of crazy paving in 39%, rounded morphology in 32%, and linear opacities in 27% of patients, respectively. Also, 91% of patients had bilateral pneumonia distribution. Multiple lobes (two or more lobes) and anteroventral involvement were present in 93% of participants, and the right lower lobe (93%), left lower lobe and right upper lobe (both 91%) were the most involved lobes (28). CT findings in the quarantine ward of Tongji Hospital in January 2020 were typically single or multiple patchy ground glass shadows with septal thickening, but as the disease progressed and the lesion increased, the range expanded and ground glass shadow appeared simultaneously with solid shadow or stripe shadow (29). In Homayounieh et al.'s study at Firoozgar Hospital in Tehran, pure ground-glass opacities were the most common for all lung lobes (more than 60%) and the left and right lower lobes were more severely involved in the deceased’s than in the survivors (26). In Zhou's study at Jinyintan Hospital and Wuhan Pulmonary Hospital, 88.8% of patients on the chest radiological checkup, showed ground-glass opacities, consolidation or both, and 67% had bilateral lung involvement. The highest incidences were reported in the right lower lobe and left lower lobe (67.1% and 64.7%, respectively). It was also found that people with abnormal radiographs showed clinical features clearer (12). The Shahriarirad research in Shiraz found that ground-glass opacity was the most prevalent abnormality in chest CT scans (93.9%), followed by consolidation (58.5%) (25). The present study, by recording and reviewing clinical findings, can be helpful in comparing the similarities and differences of the results of the disease in Iran with other parts of the world. On the one hand, the results of this study can help prevention and treatment, and on the other hand, it is an opportunity to examine whether there is a difference in the epidemiological features and clinical outcomes of patients with COVID-19 in this region with the rest of the world or not.
The present study had some limitations. The number of study samples is small. Also, in the study, there is no information related to the patient's laboratory findings.
5.1. Conclusions
In general, the current results of this analysis on clinical findings and CT scans of SARS-COV-2 patients are more or less consistent with the rest of the world. The most common clinical symptoms were cough, shortness of breath and fever, respectively. Ground-glass opacity,Consolidation and crazy-paving changes were observed in CT scan of the chest in the majority of patients. It is recommended that more literatures be performed in larger populations according to types of COVID-19 Variants, as well as by examining more risk factors to describe the course and severity of this disease accurately.