1. Background
The world has experienced outbreaks of SARS-CoV in 2002 - 2003 and MERS-CoV in 2011, both of which, are related to the causal agents from the coronavirus family (1). At the end of 2019, another novel coronavirus, SARS-CoV2 (causing COVID-19), emerged from Wuhan, China and spread to other countries which led to the global crisis in health care systems and many aspects of human life (2). Although many COVID-19-related clinical features including transmission rate, mortality, and clinical symptoms have been largely determined by now, more time is still needed to elucidate the unknown clinical characteristics of the disease, particularly the immune response against the infection (3). The clinical course of COVID-19 varies depending on individuals’ characteristics and medical status (4). The spectrum of clinical manifestations can be seen in COVID-19 patients ranging from mild symptoms (e.g., cough, fever, headache, sore throat, malaise, muscle pain, loss of taste and smell, nausea, vomiting, and diarrhea) resolving in a few days to critical illness with acute respiratory distress syndrome (ARDS), and multiple organ failure, which may even cause the death of affected individuals (5). It is not clear why the disease can lead to fatal pneumonia in some adults while others experience mild symptoms, however, older age, male gender and underlying disorders, such as diabetes, hypertension, malignancy, chronic obstructive pulmonary disease, obesity and inflammatory diseases have been identified as risk factors for the occurrence of severe infections (6, 7). Many studies have focused on the early identification of severe cases of COVID-19 which may require hospitalization and intensive care (8). In this respect, some pivotal tests, such as high-resolution computed tomography of the lung and nucleic acid amplification techniques have been suggested for early diagnosis as well as prediction of COVID-19 disease severity (9, 10). However, most of these tests are expensive and they may not be available to all patients during an outbreak with an explosive increase in the number of patients or in places where medical facilities are limited (11). On the other hand, the role of laboratory medicine is essential in early diagnosis, prognosis and management of COVID-19 disease (12). Investigation of medical laboratory parameters which serve as possible predictive markers for COVID-19 disease progression and mortality risk, can increase clinical awareness, guide therapeutic interventions and manage human and medical resources in an efficient way (13). A complete blood count (CBC) analysis is one of the most common laboratory tests measuring the count of red blood cells (RBC), white blood cells (WBC), platelets (PLT) and other related factors (14). Each of these types of blood cells performs critical functions, so measuring their levels can provide important information on the individual’s health (5). Complete blood count is a simple and very informative test, readily available in areas with limited health care facilities and also at the peak of the disease when access to paraclinical facilities is limited (3, 11). Therefore, it may provide a valuable tool for risk assessment of COVID-19 disease.
2. Objectives
In this study, we assessed the differences in CBC parameters between 4 groups of COVID-19 patients and healthy individuals.
3. Methods
3.1. Study Population
This study was conducted between January and March 2022 at Golestan Hospital of Kermanshah University of Medical Sciences in the west of Iran. The hospital information system was reviewed and 147 patients referred to the emergency department of the hospital with COVID-19 infection confirmed by real-time polymerase chain reaction on nasopharyngeal swab samples, were included in the study. In addition, 95 COVID-19 negative individuals without diseases affecting CBC results were randomly selected as the control group. The hospital laboratory software was used to retrieve the results of gender, age and CBC test upon admission. The outcome of hospitalization (discharge or death) were also recorded for the participants. All the patients were divided into 4 groups based on the presenting symptoms including fever, cough, fatigue, anorexia, myalgia, sore throat, nasal congestion, headache, diarrhea, vomiting nausea, low oxygen saturation, radiological pneumonia, shock and any kind of organ failure. The assigned groups were as follow: Mild (no need for hospitalization); moderate (hospitalization in the general ward), severe (required hospitalization in the intensive care unit (ICU)) and deceased (occurring death as a result of disease complications). The CBC parameters that were examined included: WBC (× 109/L), neutrophil (%), lymphocyte (%), neutrophil-to-lymphocyte ratio (NLR), monocyte (%), eosinophil (%), basophil (%), RBC (× 1012/L), hemoglobin (Hb) (g/dL), hematocrit (Hct) (%), mean corpuscular volume (MCV) (fL), red cell distribution width (RDW) (%), PLT (×109/L) mean platelet volume (MPV) (fL), platelet distribution width (PDW) (fL) and platelet large cell ratio (PLCR) (%). The reference ranges were WBC: 4 - 10 × 109/L; RBC: 4.5 - 6.3 × 1012/L in males and 4.2 - 5.4 × 1012/L in females: PLT: 140 - 400 × 109/L (15).
3.2. Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki and approved by the Ethics Committee of Kurdistan University of Medical Sciences with the ethics ID IR.MUK.REC.1401.030. Due to the retrospective nature of the study, informed consent of the patients was not required by the ethics committee.
3.3. Statistical Analysis
The obtained data were analyzed using a chi-square test at the significance level of P < 0.05 (SPSS software, version 23) to examine the differences between patient groups and control individuals.
4. Results
In our study, 147 patients and 96 healthy individuals of Kurdish ethnicity were included. The distribution of disease severity among the patients were as follow: 55 (37.41%) patients had mild symptoms, 35 (23.8%) patients showed moderate disease, 39 (26.53%) patients developed a severe form of the disease and were hospitalized in ICU and finally 12 (12.24%) patients died while hospitalized. The median age of patients in different groups significantly increased in proportion to the severity of the disease. The frequency of male gender was more common among the patients, especially in those with decease outcomes, however, it was not statistically significant (P = 0.053) (Table 1).
| Variables | Controls (n = 95) | Patients (n = 147) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild (n = 55) | P-Value | Moderate (n = 35) | P-Value | Severe (n = 39) | P-Value | Deceased (n = 18) | P-Value | ||
| Gender (No. (%)) | 0.288 | 0.647 | 0.503 | 0.053 | |||||
| Male | 45 (47.4) | 31 (56.4) | 15 (42.9) | 16 (41) | 13 (72.2) | ||||
| Female | 50 (52.6) | 24 (43.6) | 20 (57.1) | 23 (59) | 5 (27.8) | ||||
| Age (Median ± IQR) | 61 ± 17 | 66.5 ± 26 | 1.00 | 60.5 ± 12 | 0.966 | 72 ± 13 | 0.024 | 78.5 ± 10 | 0.005 |
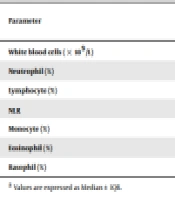
Our findings showed that WBC count in mild COVID-19 patients was slightly lower than the other groups (P = 0.264). It was also shown that WBC count in patients placed in moderate, severe and deceased groups significantly increased compared to the control group. However, this increase was more apparent in moderate COVID-19 patients than on the other 2 groups. The number of neutrophils was significantly higher in all groups of patients and increased proportionally with the severity of the disease. Lymphocyte count was also significantly lower in all groups of patients which was accompanied by significant increases in neutrophils. Neutrophil, lymphocyte and NLR parameters an, were shown to have the strongest correlation among the studied parameters in CBC test (P = 0.000) (Table 2).
| Parameter | Controls | Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild (n = 55) | P-Value | Moderate (n = 35) | P-Value | Severe (n = 39) | P-Value | Deceased (n = 18) | P-Value | ||
| White blood cells (× 109/L) | 6.92 ± 2.04 | 6.83 ± 3.8 | 0.264 | 12.14 ± 10.89 | 0.004 | 7.9 ± 6.6 | 0.006 | 7.61 ± 10.4 | < 0.001 |
| Neutrophil (%) | 56.25 ± 11.7 | 77.2 ± 15.1 | < 0.001 | 79.85 ± 9.9 | < 0.001 | 84.45 ± 8.8 | < 0.001 | 82.35 ± 13.8 | < 0.001 |
| Lymphocyte (%) | 32.95 ± 9.7 | 13.4 ± 9 | < 0.001 | 10.35 ± 9.3 | < 0.001 | 10.75 ± 8.7 | < 0.001 | 11.65 ± 10.8 | < 0.001 |
| NLR | 1.85 ± 0.86 | 5.81 ± 4.92 | < 0.001 | 7.93 ± 5.27 | < 0.001 | 8.05 ± 6.64 | < 0.001 | 7.32 ± 5.72 | < 0.001 |
| Monocyte (%) | 8.2 ± 2.5 | 4 ± 4 | < 0.001 | 6.25 ± 4.4 | < 0.001 | 3.6 ± 2.5 | < 0.001 | 2.65 ± 2.2 | < 0.001 |
| Eosinophil (%) | 2.2 ± 1.4 | 1.85 ± 2.2 | 0.053 | 0.9 ± 2.2 | 0.016 | 1.75 ± 2 | 0.078 | 2.35 ± 3.2 | 1.000 |
| Basophil (%) | 0.4 ± 0.3 | 0.3 ± 0.4 | 1.000 | 0.4 ± 0.4 | 0.845 | 0.3 ± 0.4 | 0.608 | 0.4 ± 0.4 | 1.000 |
a Values are expressed as Median ± IQR.
The number of monocytes also significantly decreased in all groups of patients, but it was statistically less significant than the correlation found in lymphocytes. The eosinophil count was significantly lower in mild, moderate and severe COVID-19 patients, but insignificantly higher in deceased patients (P > 0.05). The basophil count was the only parameter in CBC test that was not correlated with COVID-19 infection in all 4 patient groups. The RBC, Hb and Hct parameters significantly decreased with aggravation of disease severity. The MCV significantly reduced only in moderate COVID-19 patients group compared to control individuals (P = 0.015); and insignificantly increased in other groups of patients (P > 0.05) (Table 3). The RDW increased in all groups of patients.
| Parameter | Controls | Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild | P-Value | Moderate | P-Value | Severe | P-Value | Deceased | P-Value | ||
| Red blood cells (× 1012/L) | 4.77 ± 0.6 | 4.78 ± 0.78 | 0.932 | 3.83 ± 0.77 | < 0.001 | 4.12 ± 1.2 | 0.042 | 4.47 ± 2.11 | < 0.001 |
| Hemoglobin (g/dL) | 13.9 ± 1.9 | 13.25 ± 3.3 | 0.709 | 10.8 ± 1.8 | < 0.001 | 12.1 ± 3.1 | 0.044 | 12.65 ± 3.6 | < 0.001 |
| Hematocrit (%) | 40.3 ± 4.9 | 40.25 ± 6.2 | 0.908 | 32.5 ± 5.6 | 0< 0.001 | 36.75 ± 10.4 | 0.020 | 37.55 ± 14.1 | < 0.001 |
| Mean corpuscular volume (fL) | 84.75 ± 6.3 | 85.90 ± 8.8 | 0.988 | 81.75 ± 12.6 | 0.015 | 88.10 ± 7.9 | 0.247 | 85.25 ± 7 | 0.649 |
| Red cell distribution width (%) | 13.90 ± 1.3 | 13.95 ± 1.8 | 0.971 | 15.50 ± 2.4 | < 0.001 | 14.15 ± 2.2 | 0.781 | 15.65 ± 5 | < 0.001 |
a Values are expressed as Median ± IQR.
In addition, PLT parameter was shown to be generally reduced in patient groups, particularly in deceased patients (P < 0.001) (Table 4). The two parameters of MPV and PDW significantly increased only in the moderate COVID-19 patients. This study showed that WBC, monocyte and PLT parameters show an increasing peak; while eosinophil, RBC, Hb, Hct and MCV parameters display a decreasing peak in the moderate COVID-19 patients group compared to other groups of patients.
| Parameter | Controls | Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild | P-Value | Moderate | P-Value | Severe | P-Value | Deceased | P-Value | ||
| Platelet (× 109/L) | 225.5 ± 64 | 202 ± 88 | 0.368 | 237.5 ± 184 | 0.790 | 187 ± 138 | 0.992 | 146 ± 73 | < 0.001 |
| Mean platelet volume (fL) | 10.2 ± 1.1 | 9.95 ± 1.8 | 0.710 | 10.4 ± 0.9 | 0.038 | 10.3 ± 0.7 | 0.962 | 10.3 ± 1.5 | 0.998 |
| Platelet distribution width (%) | 12.4 ± 2 | 11.9 ± 4 | 1.00 | 13.3 ± 2.7 | 0.003 | 12.8 ± 1.8 | 0.945 | 14.1 ± 3.9 | 0.79 |
| Platelet large cell ratio (%) | 26.65 ± 8.4 | 23.55 ± 12 | 0.553 | 28.7 ± 4.7 | 0.054 | 27.4 ± 4.9 | 0.989 | 28.45 ± 10.9 | 0.278 |
a Values are expressed as Median ± IQR.
Table 5 shows the frequency of WBC, RBC, and PLT abnormalities in patients and controls. Leukocytosis was at least 5 times as high as leukopenia in all groups of patients (P < 0.001). Also, the rates of anemia and thrombocytopenia were significantly higher than polycythemia and thrombocytosis, respectively (P < 0.001).
| Variables | Controls | Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild | P-Value | Moderate | P-Value | Severe | P-Value | Deceased | P-Value | ||
| Normal white blood cells | 95 (100) | 38 (69.1) | < 0.001 | 20 (57.1) | < 0.001 | 21 (53.8) | < 0.001 | 9 (50) | < 0.001 |
| Leukopenia | 0 (0) | 2 (3.6) | 2 (5.7) | 3 (7.7) | 0 (0) | ||||
| Leukocytosis | 0 (0) | 15 (27.3) | 13 (37.1) | 15 (38.5) | 9 (50) | ||||
| Normal red blood cells | 88 (93.6) | 37 (67.3) | < 0.001 | 8 (23.5) | < 0.001 | 20 (51.3) | < 0.001 | 6 (33.3) | < 0.001 |
| Anemia | 6 (6.4) | 16 (29.1) | 23 (67.6) | 17 (43.6) | 12 (66.7) | ||||
| Polycythemia | 0 (0) | 2 (3.6) | 3 (8.8) | 2 (5.1) | 0 (0) | ||||
| Normal platelets | 94 (98.9) | 42 (76.4) | < 0.001 | 21 (61.8) | < 0.001 | 31 (79.5) | < 0.001 | 8 (44.4) | < 0.001 |
| Thrombocytopenia | 0 (0) | 11 (20) | 11 (32.4) | 6 (15.4) | 10 (55.6) | ||||
| Thrombocytosis | 1 (1.1) | 2 (3.6) | 2 (5.9) | 2 (5.1) | 0 (0) | ||||
a Values are expressed as No. (%).
5. Discussion
COVID-19 caused a severe pandemic rapidly spreading all over the world and affected individuals of all ages (1). However, many studies have demonstrated that elderly patients with COVID-19 showed higher mortality rates compared with younger patients (16, 17). Our results showed that the median age of controls was 61 years compared to 78.5 years in patients who died of the disease. Also, we noticed that 53.1% of all patients and 72.2% of deceased patients were male individuals. Consistently, many similar studies have also reported that the disease is more severe in older subjects and men are more likely to contract the disease (13, 14, 16). A possible explanation for this finding may be due to the biological diversity of the immune system and genetic factors, making men more vulnerable to COVID-19 infection than women (17). In addition, characteristic male-type lifestyle including less activity, more smoking and drinking habits as well as less commitment to social distance increases the risk of infection in men (17, 18). Bwire reported that women were more responsible than men for the COVID-19 crisis (19). Since the COVID-19 disease is associated with high hospitalization rates, respiratory failure, and death especially in older patients, many efforts have been made to early prediction of severe and critical conditions in COVID-19 patients (12, 13).
In order to improve the quality of our study, the patients were classified into 4 groups according to the severity of the disease. Our findings indicated that almost all CBC parameters, except for basophils and PLT, changed significantly in the group of moderate COVID-19 patients. On the other hand, in the group of patients admitted to the ICU and deceased patients, PLT parameters did not show a statistically significant difference from the control group. These findings imply that in moderate COVID-19 infection, the body completely fights against the disease. In this study, among the nine parameters that are routinely tested in a CBC analysis, neutrophils, lymphocytes and monocytes displayed the most drastic changes in patients compared to the controls whereas basophil count was the only parameter that was not correlated with COVID-19 infection in all 4 patient groups.
Data gathered from extensive studies on the COVID-19 outbreak supports that increased neutrophils, combined with decreased lymphocytes are associated with an increase in disease severity and poor prognosis (3, 12, 14, 18). It is still unclear whether neutrophils count is just a biomarker of disease severity or has a particular pathogenic role. It is thought that COVID-19 mortality rate is often associated with thromboembolic complications and systemic inflammation. Neutrophilia is a marker of venous thrombosis and holds a role in necrotic inflammatory response (6, 13). In addition to phagocytosis, neutrophils exert their protective roles through the formation of extracellular traps (NETs) (20). Neutrophil extracellular traps are useful in host defense against pathogens but may cause side effects during infection (21). Improper phagocytosis and excessive formation of extracellular traps during COVID-19 infection may play a role in the development of cytokine storms during infection (20).
Cytokine storm is known as the cause of ARDS and severe inflammatory response syndrome (SIRS) (9). Chen et al. analyzed laboratory data in 29 COVID-19 patients noting lymphopenia in 20 patients which is in consistent with our results (22). Lymphocytes are crucial in maintaining the immune homeostasis and inflammatory responses (5). Some mechanisms have been reported for reduction of lymphocyte count at COVID-19 patients, including the direct virus attack and killing lymphocytes or virus-mediated destroying lymphatic organs such as thymus and spleen (3). Another possible mechanism is the disruption of inflammatory cytokines which in turn results in lymphocyte apoptosis during the disease course (22). Among the studies conducted in this regard, the study by Qin et al. was most consistent with our data (23). They performed a study on laboratory data from 452 COVID-19 patients, and concluded that the patients showed higher WBC count and lower lymphocytes, monocytes, basophils and eosinophils compared to the control group (23). Our findings with respect to the monocytes decrease observed in severe and deceased groups, may be the result of widespread tissue inflammation and staying of monocytes at the site of inflammation. It was suggested that eosinophil play beneficial roles in COVID-19 patients and reduce the inflammation caused by neutrophils (6). Studies demonstrated that normal eosinophil count has been associated with more favorable results (14).
In our study, RBC, Hb and Hct, were significantly decreased only in hospitalized patients groups (moderate, severe and dead) and not in outpatients (mild). These findings are consistent with many studies such as Yuan et al. which found that severe and critical COVID-19 patients had significantly reduced Hb and RBC counts (18). Although the exact mechanism of anemia in COVID-19 patients is not known, it is suggested that the cause lies in inhibition of erythropoiesis in the bone marrow (13). However, we suggest that this may also be caused by blood dilution following the application of large amounts of injection solutions in hospitalized patients.
We noticed the proportional decrease of PLT with aggravation of disease severity, however, this observation was only significant in the deceased patients compared to the controls (P < 0.001) which was in line with the results of Yang et al., showing that a decrease in PLT count was associated with an increased risk of mortality in hospitalized patients (17). The mechanism of PLT depletion in COVID-19, especially in severe and deceased patients is yet to be uncovered. Platelets are probably aggregated and consumed during diffuse thrombosis or pulmonary blood vessel thrombosis (17). Many studies have focused on different blood cell ratios and biochemistry tests to predict the consequences of COVID-19 infection (3, 5, 22). However, our study was conducted based only on CBC parameters and did not include any other laboratory tests. This was partly because CBC test is simple and easy to perform even in emergency situations (12). The limitations of our study included the relatively small sample size as well as the retrospective nature of the analysis. Furthermore, we did not consider the peripheral blood smear results. Despite these limitations, we demonstrated that the CBC parameters especially neutrophils and lymphocytes can be used to determine the COVID-19 disease prognosis and identify those patients who are at higher risk of mortality while hospitalized. Confirmation of these findings may help provide new useful tools or clinical determinants for classifying COVID-19 patients based on their prognosis.