1. Background
The first case of COVID-19 occurred in 2019 in Wuhan, China (1, 2). At first, due to the unknown and emerging nature of the disease (3), various measures were taken to control and manage the epidemic (4). Different institutions such as the World Health Organization (WHO) (5-8), the Centers for Disease Control and Prevention (CDC) (9), and the Food and Drug Administration (FDA) (10) sought to control the disease and provide accurate and timely information to people. Health-related institutions and the MOH of different countries also took different steps in this regard (11-13). Inspired by the emergent conditions of the disease, the recommended public isolation and quarantine, and the need for keeping a social distance (14-16), health institutions used e-health services.
E-health entails the use of information and communication technology (ICT) in multiple ways to affect health (17). Information and communication technology is an umbrella term that encompasses all communication technology devices such as cell phones, personal computers, social media applications, the Internet, wireless networks, software, and video conferencing, and enables people to interact with each other in the digital world (18-20).
Different countries have used e-health to take different measures against the COVID-19 virus. For one, a mobile application (corona data donation) was developed by the Robert Koch Institute. The application continuously tracks data related to a user's health and daily activities (21). In the Ugandan government, telemedicine methods have also increased, including tele-counseling, telepsychiatry, call centers, and health information dissemination using mobile phones (22). The Ministries of Health of Kenya, China, and Taiwan have also used this platform to convey the required information to the public about COVID-19 (23-25).
The Iranian health system has also taken preventive measures to control the pandemic, including using ICT for public awareness-raising, public education, social participation, and initiating communication systems to deal with the pandemic (26). Examples of measures are using communication systems such as 4030 and 190 call centers, the http://www.salamat.gov.ir self-screening system, sending awareness-raising text messages, and launching a website to share information and instructions about COVID-19 (27, 28).
Among the factors that need to be examined is the extent to which people in society use and benefit from the services, find them useful, and feel satisfied. A body of research examined the usage, usefulness, and satisfaction variables as perceived by people using technologies in the COVID-19 pandemic (29-33). However, few studies have examined the usefulness, satisfaction, and effectiveness of e-health services provided by healthcare providers. Some of these studies have only examined public perceptions, acceptance, and effectiveness of digital contact tracking applications in France, Australia, and Ireland (34-37).
Health institutions provide services on a large scale and address a wide range of people in society. Moreover, the level of satisfaction, usefulness and use of e-health services are among the factors that can, by measuring them, their maximum advantage can be achieved. Therefore, the present study explored the usage of e-health services and the public’s perceived usefulness and satisfaction with these services in Iran during the pandemic. This study can help e-health technology developers and policymakers to implement these services better.
1.1. E-health Services of Iran MOH at the Outset of the Pandemic
The measures taken include sending text messages, assigning phone numbers 4030 and 190 to answer people's questions, launching the Salamat.gov system for screening people, MASK application, SAMANE application, publishing information about COVID-19 on the MOH website, mass media, especially television and radio, and groups and channels on social networks. The text messages sent by the MOH contained educational information about COVID-19, including the use of masks, keeping a social distance, and so on. The screening system worked by entering a national id number, asking simple questions for self-assessment of COVID-19, and providing the necessary instructions according to the latest instructions of the ministry. Upon entering the system, the symptoms of the disease were enquired, such as a fever, chills, dry cough, sore throat, and shortness of breath. Then the system asked about the presence of a family member suspected of the disease. If the person's answers were positive, health recommendations were made, and for more detailed guidance, the visitor was referred to the relevant healthcare provider (e.g., the nearest healthcare center). At the same time, the relevant healthcare provider received a text message in this regard and was made responsible for the subsequent follow-up of the suspect and those around him/her. Also, after screening and suspecting the person, the healthcare provider would contact the suspects registered in the system by calling 4030 and would provide the necessary consultation and follow-up.
SALAMAT and MASK applications have also been developed to prevent people and others from COVID-19 infection. People can see a map of high-risk areas and, by entering daily information related to their health condition, assess the chances of family members and their own infection with the disease. The information provided on the ministry website, networks, and social media has also been to raise awareness of the features and symptoms of the disease and the related health issues.
2. Methods
2.1. Design and Sample Size
The present cross-sectional descriptive study was conducted through an online questionnaire survey in Kerman in November 2021. The study population included all people in Kerman province, not restricted to a particular ethnicity and region. The inclusion criteria were the age over 16 years, living in Kerman and providing informed consent at the beginning of the study, having internet access to complete the online survey, and being literate. The sample size was estimated at 384 using the Cochrane formula. The estimated error (d) was 5%. Due to the possibility of sample attrition (for non-responded or incomplete questionnaires) and increasing accuracy in the study, the sample size was finally decided to be 500.
2.2. Study Instrument
The data collection instrument was a researcher-made questionnaire with four sections and 33 questions overall. The first section contained nine questions to explore demographic information (i.e., age, sex, education, family history of infection with COVID-19, and history of exposure to or suspicion of COVID-19). The second section included eight questions about the rate of use. The third section had eight questions about the usefulness of e-health measures, and the fourth section consisted of eight questions exploring people's satisfaction with the e-health services. The questions of the second, third and fourth sections were rated on a 5-point Likert scale ranging from 0 (minimum rating) to 4 (maximum rating).
Before the primary data collection phase, to check the readability of the questionnaire content, we evaluated the face validity. Validation was done by five medical informatics specialists (with a background in medicine and health information management). Their comments were used to make the required adaptations and prepare the final version of the questionnaire. Then the questionnaire was piloted on 20 participants to test its reliability. These participants were then excluded from the final analysis. The reliability of the questionnaire was confirmed using Cronbach's alpha (0.87). The online version of the questionnaire was developed in Google Form. The link was shared with the contacts on different social networks (WhatsApp, Telegram, LinkedIn, and Iranian social networks such as Soroush, GAP, and Bale).
2.3. Statistical Analysis
The data were finally analyzed in SPSS 24. Logistic regression analysis was used to test the relationship between demographic variables and the usage, usefulness, and satisfaction variables. Pearson correlation coefficient was used to test the association between the three sections.
3. Results
Out of 540 questionnaires, 15 were discarded because the participants were under 16 years of age. Finally, 527 questionnaires were retained for analysis. Table 1 summarizes the demographic information. The participants’ age ranged from 16 and 61 years (mean = 27). The majority of participants (76.5%) were women. About half of the participants (49.5%) had associate and bachelor's degrees. More than half of the participants (63.8%) were single. Less than 10% (i.e., 6.5%) had a comorbidity disease, mostly in the heart, kidney, bile, hypertension, asthma, multiple sclerosis, and thyroid problems. 82.2% of participants had no history of COVID-19, and 60.9% reported that none of their family members had a history of the disease.
| Demographic Variable and Levels | No. (%) |
|---|---|
| Age (y) | |
| < 20 | 78 (14.8) |
| 20 - 40 | 417 (79.1) |
| 40 - 60 | 30 (5.7) |
| 60 < | 2 (0.4) |
| Gender | |
| Male | 124 (23.5) |
| Female | 403 (76.5) |
| Education | |
| High school | 36 (6.8) |
| Diploma | 78 (14.8) |
| Associate and bachelor’s degrees | 261 (49.5) |
| Master’s and higher | 152 (28.8) |
| Marital status | |
| Single | 336 (63.8) |
| Married | 191 (36.2) |
| Background disease | |
| Yes | 34 (6.5) |
| No | 493 (93.5) |
| History of COVID-19 | |
| Yes | 94 (17.8) |
| No | 433 (82.2) |
| Family history of COVID-19 | |
| Yes | 206 (39.1) |
| No | 321 (60.9) |
3.1. The Usage Rate, Perceived Usefulness, and Satisfaction with E-health Services
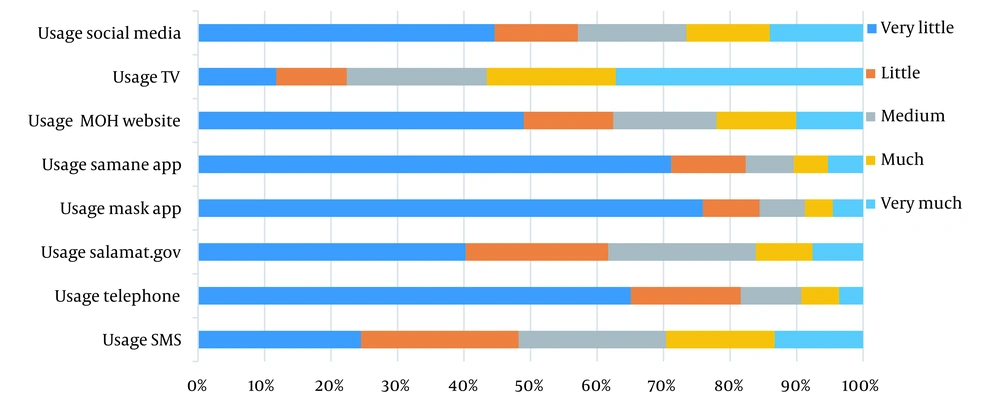
Figure 1 shows the extent to which the participants used the e-health services. The most frequent use was to acquire information about COVID-19 from mass media such as television, and after that, from the MOH social networks as well as the awareness-raising text messages sent by the ministry.
Table 2 shows the usefulness of e-health services. Thirty-two percentage of the participants perceived the information acquired from mass media such as television to be more useful. The content presented on social networks (15.0%) and the website of the MOH (14.6%) ranked next. From the participants' point of view, the least useful of the e-health services were from MASK and SAMANE applications.
| SMS | Telephone | Salamat.gov | MASK App | SAMANE App | MOH Website | TV | Social Media | |
|---|---|---|---|---|---|---|---|---|
| Very Little | 126 (23.9) | 204 (38.7) | 199 (37.8) | 400 (75.9) | 304 (57.7) | 207 (39.3) | 63 (12.0) | 201 (38.1) |
| Little | 123 (23.3) | 91 (17.3) | 100 (19.0) | 45 (8.5) | 75 (14.2) | 73 (13.9) | 72 (13.7) | 70 (13.3) |
| Medium | 118 (22.4) | 107 (20.3) | 117 (22.2) | 36 (6.8) | 79 (15.0) | 106 (20.1) | 106 (20.1) | 98 (18.6) |
| Much | 93 (17.6) | 78 (14.8) | 64 (12.1) | 22 (4.2) | 32 (6.1) | 64 (12.1) | 127 (24.1) | 79 (15.0) |
| Very Much | 67 (12.7) | 47 (8.9) | 47 (8.9) | 24 (4.6) | 37 (7.0) | 77 (14.6) | 159 (30.2) | 79 (15.0) |
According to the results summarized in Table 3, 28.8% of the participants were more satisfied with the content through mass media such as television. The level of people's satisfaction with the content provided on social networks (15.4%) and the MOH website (13.3%) ranked next. The lowest level of participants' satisfaction was with MASK and SAMANE applications.
| SMS | Telephone | Salamat.gov | MASK App | SAMANE App | MOH Website | TV | Social Media | |
|---|---|---|---|---|---|---|---|---|
| Very Little | 132 (25.0) | 220 (41.7) | 201 (38.1) | 327 (62.0) | 311 (59.0) | 211 (40.0) | 69 (13.1) | 209 (39.7) |
| Little | 111 (21.1) | 94 (17.8) | 105 (19.9) | 64(12.1) | 73 (13.9) | 77 (14.6) | 77 (14.6) | 75 (14.2) |
| Medium | 130 (24.7) | 104 (19.7) | 111 (21.1) | 71 (13.5) | 74 (14.0) | 104 (1907) | 113 (21.4) | 95 (18.0) |
| Much | 86 (16.3) | 70 (13.3) | 60 (11.4) | 32 (6.1) | 37 (7.0) | 65 (12.3) | 116 (22.0) | 67 (12.7) |
| Very Much | 68 (12.9) | 39 (7.4) | 50 (9.5) | 33 (6.3) | 32 (6.1) | 70 (13.3) | 152 (28.8) | 81 (15.4) |
The logistic regression analysis showed that single participants’ satisfaction with text messages was 0.39 less (than that of married) (95% CI (0.13 to 0.64), P = 0.003). Participants with a history of COVID-19 were 0.44 less satisfied with the screening system of the ministry (95% CI (0.11 to 0.78), P = 0.009) than those without a history of COVID-19. Those with a master's degree or higher, using MASK application (95% CI (0.24 to 1.32), P = 0.004) were 0.87 less satisfied with e-health services than those with a diploma. The level of satisfaction in married participants with the information provided on the Ministry website was 0.40 higher than the single (95% CI (0.13 to 0.68), P = 0.004). There was no statistically significant relationship between other demographic variables and satisfaction with the e-health services.
3.2. The Relationship Between the Rate of Usage, Perceived Usefulness, and Satisfaction
There was a positive correlation between the usage rate and satisfaction with each e-health service. The relationship was stronger between the usage rate and satisfaction with social networks than with other services (r = 0.87, P < 0.0001). The correlation between the use of exclusive phone numbers for public questions about COVID-19 and perceived satisfaction was weaker (r = 0.58, P < 0.0001). In other cases, there were also significant positive correlations. In all cases, the estimated p-value was below 0.0001 (Table 4).
| r (Correlation Between the Rate of Use and Perceived Satisfaction) | r (Correlation Between Usefulness and Perceived Satisfaction) | r (Correlation Between the Rate of Use and Perceived Usefulness) | |
|---|---|---|---|
| SMS | 0.78 | 0.88 | 0.81 |
| Telephone | 0.58 | 0.89 | 0.53 |
| Salamat.gov | 0.74 | 0.92 | 0.71 |
| MASK app | 0.75 | 0.75 | 1 |
| SAMANE app | 0.77 | 0.92 | 0.77 |
| MOH website | 0.81 | 0.94 | 0.80 |
| TV | 0.81 | 0.94 | 0.85 |
| Social media | 0.87 | 0.95 | 0.88 |
a Correlation is significant at the 0.01 level (2-tailed).
A positive correlation was found between the usefulness and satisfaction of each e-health service. The relationship between the usefulness of social networks and satisfaction with them was stronger than other services (r = 0.95, P < 0.0001). The relationship was weaker in the perceived usefulness of MASK with perceived satisfaction (r = 0.58, P < 0.0001). In all cases, the estimated P-value was below 0.0001 (Table 4).
There was also a positive relationship between perceived usefulness and the rate of using each e-health service. The relationship between the perceived usefulness of MASK and its rate of use was stronger than other measures (r = 1, P < 0.0001). The relationship between the usefulness of the phone and the rate of using it was weaker (r = 0.53, P < 0.0001). In all cases, the estimated P-value was below 0.0001 (Table 4).
4. Discussion
The present findings showed that among the e-health services, providing information through mass media, television, and then social networks had the highest rate of use, usefulness, and satisfaction. The newly introduced applications had the least rate of use, usefulness, and satisfaction. Also, the present findings showed that the correlation between the rate of using e-health services and their perceived usefulness and satisfaction was positive. There was also a positive association between these services' usage rate and usefulness.
The present participants maintained they mostly used mass media such as television and then social networks. Mobile health applications were used less frequently. One reason for the higher rate of using TV was the public’s perceived authenticity of this source. Also, in Casero-Ripolles’ study (38) in North America and Moreno et al.’s study (39) in Spain, mass media such as television and social networks were used most frequently. Lau et al. (40) in the Philippines conducted a study on the low-income population. They reported that more conventional mass media, such as television and radio, were the main sources of information about the COVID-19 virus. In their study, Kakemam et al. (41) found mass media and the internet as the main sources used by Iranian people to acquire information about the coronavirus.
Inadequate introduction of applications developed by Iran MOH and unawareness of the existing applications can be one reason for the less frequent use. Besides, different studies (34, 37, 42, 43) on mobile applications during the pandemic showed that privacy and expected usefulness were among the reasons for not using mobile applications. Users preferred programs with higher usefulness.
As the participants perceived, the most useful services were provided first on television and then on social networks, respectively. A review by Gunasekeran et al. (44) showed that social networks have potentially useful applications for public health communication, monitoring, and predicting values due to their key properties. The results of a study by Leong et al. (45) also showed that a social media-based program was effective in increasing the knowledge, attitude, and self-care activities among diabetic patients. This application was a potentially useful means of providing diabetes education to patients through mass media, especially during the COVID-19 pandemic. Studies (46-48) found telephone counseling, and Middleton et al. (49) found short text messages as the most useful means of informing, keeping in touch, and as a result preventing the risk of COVID-19 infection.
In the present study, the highest level of participants' satisfaction was with television and then with social networks. In their study, Alanzi et al. (50) evaluated the MAWID mobile application used by the Saudi MOH to manage primary care appointments. Most participants were truly satisfied with the program, and mobile applications showed to be very effective in providing healthcare services during the pandemic. In their study, Timmers et al. (51) explored people’s satisfaction with the applications used during the COVID-19 pandemic. Their study showed the successful implementation and use of the program in COVID-19 education. People also expressed a high level of satisfaction with the information provided by these applications.
The present study showed that the relationship between the rate of usage and the perceived usefulness of e-health services was positive. There was also a positive correlation between the rate of use and the perceived usefulness of these services. A study conducted by Ohk et al. (52) showed that usefulness positively affects user satisfaction with mobile applications. Also, user satisfaction was effective in the intention to use mobile applications continuously. Park and Ohm (53) showed there was a positive correlation between satisfaction and continued intention to use health services. In a study by Koo et al. (54), usefulness was one factor that significantly affected the target user satisfaction. Our findings are in line with the technology acceptance model (TAM) (55). In this model, one factor accounting for the acceptance and use of technology is the perceived usefulness. In other words, people's perception of the usefulness of technology will translate into its use. Similarly, the present findings showed a positive relationship between usefulness and satisfaction, which is in line with the technology acceptance model and user satisfaction by Wixom and Todd (56). According to this model, satisfaction with the information produced by the system and satisfaction with the system affect the perceived usefulness. In other words, the greater the overall satisfaction with the information and system, the more likely that the use of that information and system will be useful in improving work performance.
The studies by Velicia-Martin et al. (42) and Palos-Sanchez et al. (57) showed that if applications were designed based on the technology acceptance model, they could be better accepted and used by individuals. Future investigations, especially during pandemics such as COVID-19, which need a rapid design and implementation of technologies, can use technology acceptance models to make more publicly acceptable products. The results of this research help developers and health policymakers to find out which technologies are used more and are more satisfying to people. These technologies can be used in health planning. Future research can also explore the reasons for the non-use of and dissatisfaction with technologies and, according to the research findings, develop effective and efficient methods well received by the public.
4.1. Limitations of the Study
The present study used social networks to collect research data due to Corvid’s disease 19 and the impossibility of attending communities. Therefore, there is a possibility of bias in the study population. Because not everyone has access to cell phones and the Internet, another limitation was that the data were collected mainly through self-reports, and people’s perceptions of usefulness and satisfaction were widely divergent. During the pandemic marked by the rapid use of e-health services to control the disease at the community level, there was no other way to measure the usefulness of services. Another limitation of the study was that most participants were female and those within the age range of 20 - 40, which can affect the study results. A more balanced sample of men and women and a larger variety of ages is required.
4.2. Conclusions
The present study showed that among the e-health services, in general, mass media such as television were used more than others. The participants perceived this medium as the most useful (means of communicating health-related information), and they were more satisfied with the information they acquired from television. Newly developed applications were used less frequently, and people were less satisfied with them. These findings showed a positive relationship between the rate of using e-health services and their perceived usefulness with satisfaction and a positive relationship between the rate of use and the perceived usefulness of these services. Our findings can be useful for healthcare policymakers and developers of e-health technologies. Due to the potential benefits of e-health services, their maximum efficiency can be achieved with a proper design and implementation of these services. E-health can be used appropriately during the COVID-19 pandemic with the least waste of time and money. We also suggest that technology acceptance models be used to implement e-health technologies.