1. Background
Today, home care is becoming the most common model of providing health care services. Services provided at home include different types of treatments, follow-up visits to assess postoperative recovery, routine visits to the elderly, and even complex therapies such as dialysis and intravenous therapies (1).
One of the emerging technological solutions is telehomecare (THC), which refers to a model of care using information, communication, measurement, and monitoring technologies that enable healthcare providers to communicate with patients at home (2).
Telehomecare is a new way to provide home care to patients (3). This type of providing health service is a branch of telemedicine that with the application of technology can provide health services in patients ‘homes and helps patients’ self-care and self-management (4). Telehomecare can be used from the beginning of a person’s life, such as breastfeeding care to hospice care (5).
The main reason for investing in THC is to reduce waste of time and increase access to care, as well as to promote preventive measures, as these can prevent costly emergencies (6). Stanimirovic believes that THC can have positive effects on patients’ self-care and self-management and may lead to cost savings, better access to care, and improved outcomes (7). The Liang study showed that although THC did not have a significant effect on the readmission of chronic patients, it did significantly reduce mortality and emergency visits, and significantly improved their quality of life (3). Another study of gestational diabetes patients found that the use of THC reduced visits by 56 percent, increased remote nursing supervision tenfold, and increased patient satisfaction; Patients using this technology had 16 percent financial savings compared to other similar patients (8).
Chronic diseases such as heart disease and diabetes are on the rise among the elderly, accounting for two-thirds of all deaths from these diseases (9). Iran also faces problems related to chronic patients (10) and the number of patients with chronic diseases in this country is increasing for various reasons such as lifestyle (11). In addition to increasing the number of chronic patients, the health care system is also facing an aging population (12, 13). In the near future, some countries will face an elderly community that has various problems, including chronic diseases and related complications (14, 15).
Given the benefits of home care, future health services should be provided to the community in this way (16). Due to problems such as lack of effective standards, inefficient interactions, inadequate cultural/social and professional issues that exist for the provision of home care services in Iran (17) and the growth of the number of elderly people, and the shortage of nurses (18), it is better to provide these services by THC to the people in the future according to the conditions of Iran.
2. Objectives
To prevent the possible failure of projects THC as well as to prepare the infrastructure and provide the environment, the researchers sought to identify the challenges of implementation and development of THC in Iran.
3. Methods
3.1. Study Design
This qualitative study was conducted to identify barriers to the implementation and development of THC in 2022. Due to the different conditions in Iran and the lack of information in this study, a qualitative method was used to show the experiences, knowledge, and implicit information of the participants also in this study, due to the lack of a complete theory, the content analysis was used (19).
3.2. Environment Study and Sampling
The study environment was five medical universities in Iran, and tree hospitals clinics for chronic patients Mazandaran university of medical since. In order to collect information from different dimensions and attitudes, interviews were conducted with different people. Participants in this study included managers, faculty members, physicians, nurses, patient companions, and patients. Inclusion criteria for administrators, physicians, nurses, and faculty members were familiarity with telehealth [To ensure the participants’ familiarity with telehealth, five questions were asked about their knowledge and experience in this matter. If they answered three or more questions, they were included in this study.], and for patients and companions, familiarity with basic IT concepts such as the Internet, smartphones, and applications. Participants were selected by the purposive sampling method. In other words, people who had useful information and provided their information correctly were selected as participants. The interview with the participants continued until the saturation of information, this stage ended with 23 participants. In the sampling, age diversity, job status, work experience, degree, and job position were observed.
3.3. Data Collection
After selecting the participants in the study, they were spoken to by telephone and the time of the interview and the purpose of the study were explained to them. In this telephone conversation, for the acquaintance and readiness of the interviewees, interview questions were said to them and if they wished, the interview questions were sent to them via email or messenger. In addition, the time and place of the interview were chosen by the interviewee. For the convenience of the participants, semi-structured interviews were conducted in Persian. Interview questions were compiled using literature review and expert opinions.
The interview had five questions. The interviewee was first asked to introduce himself/herself and give his/her general opinion about the use of THC. In the second question, the interviewee was asked to describe his/her experience or that of other relatives using any kind of telehealth. The next question was about the situation in Iran and its challenges to use THC. In this question, the interviewee was asked to predict what problems the situation in Iran, such as geographical conditions, people’s culture, and the dispersion of villages, might create for the implementation of THC. In the fourth question, the interviewees were asked what problems Iran might face in implementing the THC, such as laws, information and communication technology infrastructure, and the economic situation. In the last question, the interviewee was asked to state if they think there is another obstacle to the implementation of THC.
S-Recorder version 10 was used to record the interviews along with taking notes. Thirty-eight interviews were conducted and the interviews lasted between 23 to 42 minutes.
3.4. Qualitative Analysis
Respondents responses were transcribed immediately and read and listened to several times. The conventional content analysis and MaxQDA-10 software were used for data analysis. The conventional method for identifying, analyzing, and reporting patterns (themes) is very useful in qualitative studies (20, 21). Response validity, immersion, expertise, and peer check were used for the reliability of the data (22).
It should be noted that to comply with ethical considerations, after the informed consent procedures, the study participants were given a brief oral explanation of the study and were told that they could leave the study at any time. Participant code is used to report their statements to keep the information confidential. This study was approved by the Ethics Committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1400.300).
4. Results
In this study, 23 people participated, including six faculty members, three physicians, four nurses, and three manage seven patients or patient companions (Table 1).
| Job | Frequency | Age Average | Work Experience |
|---|---|---|---|
| Faculty members | 53.25 ± 12.24 | 14.37 ± 3.84 | |
| Health information managers | 3 | ||
| Medical informatics specialists | 2 | ||
| Nurses | 1 | ||
| Physicians | 47.25 ± 10.38 | 17.23 ± 5.12 | |
| Specialists | 1 | ||
| Generals | 2 | ||
| Nurses | 49.62 ± 11.24 | 21.32 ± 14.36 | |
| PhDs | 1 | ||
| Masters | 2 | ||
| Bachelors | 1 | ||
| Managers | 51.08 ± 18.44 | 18.36 ± 7.56 | |
| Physicians | 1 | ||
| Health service managers | 2 | ||
| Patients and patients’ companions | 68.24 ± 28.44 | - | |
| Patients | 3 | ||
| Patients’ companions | 4 |
Demographic Information of Study Participants
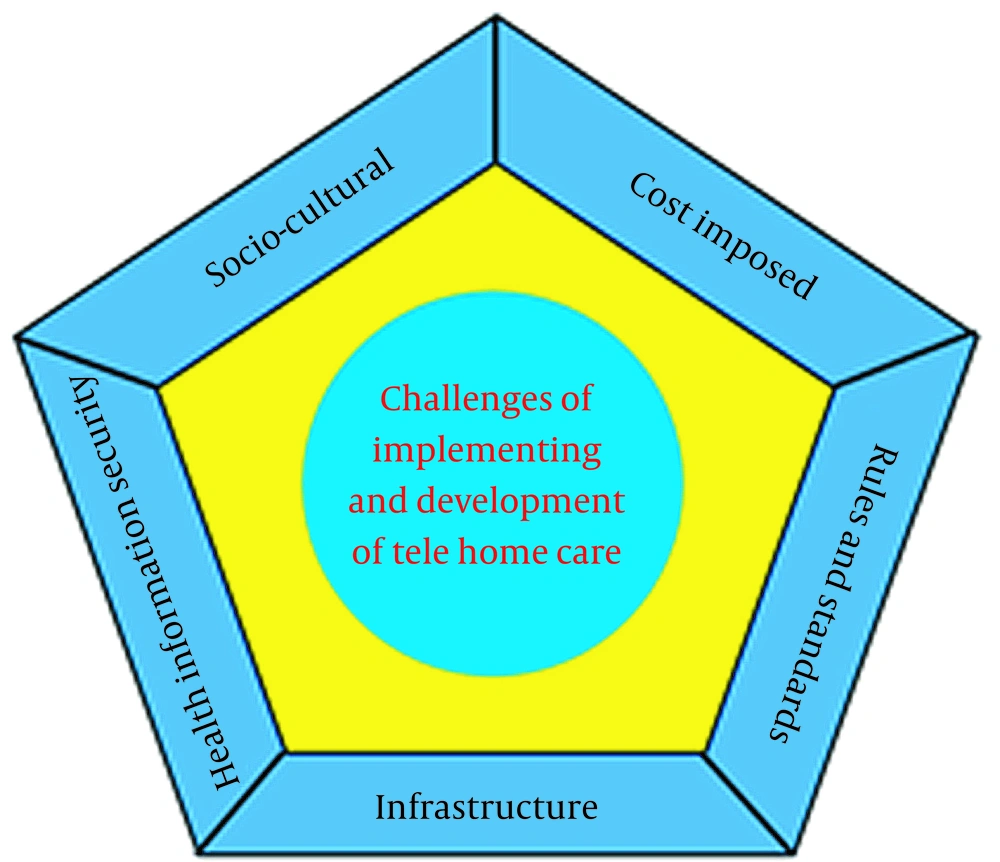
After categorizing the interviews, 5 main groups and 19 subgroups were identified as implementation and development of THC challenges (Figure 1).
4.1. Costs Imposed
Despite the savings made on the development of THC, costs are implicitly imposed on patients, healthcare providers, and healthcare organizations.
4.1.1. Costs Imposed on the Patient
When using THC certain costs such as the purchase of biosensors or digital devices to measure vital signs are imposed on the patient. In addition, patients may incur intangible costs such as spending time training or updating their smartphones. In this regard (I3) said: “It is good if it is done with common and available equipment like WhatsApp, but if other equipment is to be purchased, it is not cheap at all, how much is the equipment like that at all?”
4.1.2. Costs Imposed on the Medical Staff
One of the most important costs imposed on the medical staff, in addition to purchasing new equipment (private offices), is to spend more time, increase the risk of error, and reduce the number of patients visited. (i7): “I can examine more patients in my office. You think about it: When it takes time for the device to be ready, the patient comes, and the internet is connected. To make this happen, I examined four patients in my office.”
4.1.3. Costs Imposed on the Health Care Organization
According to the study participants, the highest cost imposed is on health care organizations. The costs of purchasing equipment, creating a standard space, hiring additional staff to be accountable, training staff, updating the network, purchasing standard software, and providing cyber security are among the costs imposed. (I4): “Please notice, if I want to implement telehealth in the hospital I need a staff on this side, one on the other side, a specialist doctor in the hospital, a general practitioner in the village, we have to pay them both, so Telemedicine is not always cheaper.” (I18): “Our workload increases. We cannot perform our routine tasks at this time. They have to hire new staff.”
4.2. Rules and Standards
Lack of rules and standards or their non-compliance and conflict with each other is one of the most important challenges to implementing and developing THC. The lack of a responsible organization to create standards, laws, and licenses can be the main cause of this problem.
4.2.1. Repayment Rules
The most important challenge in the field is repayment laws. Lack of laws related to telemedicine costs and lack of transparency also the non-acceptance of insurance for payment of THC costs is one of the problems in this area. (I18): “If it starts, they do not give us the right; all the money goes to the doctor’s pockets”. (I11): “Do you think the insurance pays for it? What about the hospital? I think the patient also likes to pay only when she/he comes to the office.”
4.2.2. Legal Rules
When using new technologies such as THC, new legal events may occur that have not yet taken root in Iran. These rules should specify the responsibilities, and consequences of non-performance of duties for each of the stakeholders, including medical staff, patients, health care organizations, Internet service providers, electronics manufacturers, application designers, and programmers.
(I 14): “Now, if something happens to the patient, who is responsible? ... Who wants to prove who’s the fault, all person says is the nurses’ fault!” (I17): “Home care is a private business, now we do not even have a law for telemedicine, let alone for home care.”
4.2.3. Obtaining a License and the Responsible Organization
At the time of interviewing the participants, none of them knew the THC licensing organization and did not envisage any process to start obtaining the license.
(I16): “Now you go and see where we can get a license for telemedicine or telehomecare.”
4.2.4. Differences in Standards
The use of different standards has sometimes hampered the exchange of information between different medical software and equipment.
(I19): “Unfortunately, because the designers of the hospital information system use different standards, we still cannot exchange information between these systems, now you know there must be a personal electronic file of the patient in this work (telehomecare).”
4.3. Infrastructure
According to the participant’s view in the study, the existing infrastructure in Iran for the implementation of THC should be upgraded.
4.3.1. Lack of Trained Staff
One of the most important infrastructures required for the implementation of THC is trained human resources. In addition to clinical expertise and familiarity with telecommunications laws, these individuals must be highly IT-literate and have a thorough knowledge of telemedicine and medical informatics.
(I5): “There was no talk of this during university and we did not take any courses in this field. Why do they expect us to do this (telehomecare)?”
4.3.2. Communication Equipment
Communication equipment in this section is the tools needed to create effective communication. These tools can vary from ordinary phones to smart biosensors depending on the type of service provided.
(I3): “If you want to do this work with a mobile phone, it is good, but if you want to connect a biosensor and things like that to the patient, this is very difficult because we do not have such facilities.”
4.3.3. Location and Space
In health care organizations, there should be an environment equipped with standards of privacy and confidentiality to provide telehealth services.
(I11): “Telehealth requires a separate room, computer, webcam, and all other things, we do not have these facilities in the hospital, we do not have basic facilities at all, let alone these facilities with a high standard.”
4.3.4. Internet and Network
Currently, the only way to communicate THC is the Internet, which is low in terms of bandwidth and speed, although these problems in Iran are to be eliminated by creating a national information network.
(I21): “You know that we do not have high-speed internet, and this inefficient internet has not spread all over the country, which means that many places do not have access to the internet.”
(I6): “Internet in our villages is weak so that we can only audio call by WhatsApp and we cannot video call”.
4.4. Information Security
Information security in the will of telehealth services includes privacy, confidentiality, and storage of information.
4.4.1. Privacy
In this study, it was found that the most important concern of patients in the use of THC is privacy.
(I23): “How to make sure that beyond Telemedicine only your doctor sees and has access to your information, you know that smartphones are hacked very quickly, the risk of hacking is higher when you use them for this purpose.”
4.4.2. Confidentiality
A clear example of this challenge was the possibility of network intrusion and hacking of THC delivery systems and software.
(I17): “Did you know that providing telehealth services with WhatsApp is prohibited in the United States? Do you know why? It is for their security because it is possible to hack them.”
4.4.3. Storage
When providing services THC, all events, consultations, telemetry data must be stored, and because the space required to store videos and images is very large. Using this technology requires a lot of space to store information and personal records of the patient.
(I16): “We have a medical record here (telehomecare) you know how the documents of these visits are stored and whether it has a legal aspect or not.”
4.5. Socio-Cultural
Problems related to the culture of communities and the characteristics of communities can be one of the most important challenges in using this technology.
4.5.1. Information Technology Literacy
One of the requirements of using THC is to have sufficient technological literacy, this challenge becomes more complicated when providing this service for the elderly or providing these services with new technologies. At the lowest level, it seems that the patient should be able to use a smartphone.
(I1): “Young people accept telehomecare, but those who are older, I am not sure. I think the home care only benefits from counseling and training.”
4.5.2. Health Literacy
Health literacy is a key component that facilitates service delivery through THC. The lower the health literacy of service recipients, the more time the treatment team spends and the greater the risk.
(I5): “My patient doesn’t know how to take their medicine. I do not think they can work with such things (telehomecare) unless someone helps them.”
4.5.3. Religion
Different societies in the Middle East have different religions, each of which has its laws, in which Muslims are required to observe the hijab and other points.
(I 22): “My religious mother wears a headscarf when we talk on WhatsApp, I think it is not comfortable for my mother.”
4.5.4. Lack of Effective Communication
Some members of the care team and even patients believe that the use of communication technologies reduces the quality of communication compared to face-to-face communication.
(I11): “I am not sure it is possible to interact with the patient; you cannot see her body language or their stress, I think it increase the s risk to diagnose and treat these conditions.”
4.5.5. Resistance of the Treatment Staff
The health care team is opposed for a variety of reasons, including concerns about declining incomes, increased workload, and increased risk of using and employing THC.
(I4): “Doctors who are busy do not do this, because of financial loss, they can easily see their patients in the office, their patients are just queuing behind the valley of their office.”
Based on the views of study participants; Security, privacy and problems of communication infrastructure were among the most important challenges (Table 2).
| Theme and Subtheme | Description | Faculty | Doctor | Nurse | The Manager | Patient | Total |
|---|---|---|---|---|---|---|---|
| Costs imposed | |||||||
| Costs imposed on the patient | Patient-imposed costs such as internet access, smartphones, purchase of biosensors and related equipment | 1 | 1 | 2 | 1 | 4 | 9 |
| Costs imposed on medical staff | Tangible and intangible costs such as wasted time and increased workload | 2 | 3 | 2 | 2 | 0 | 9 |
| Costs imposed on health care organizations | Costs of building infrastructure and staffing, training, and supervision | 1 | 2 | 3 | 3 | 0 | 9 |
| Rules and standards | |||||||
| Repayment rules | Lack of payment rules and how to repay by insurers | 4 | 3 | 3 | 3 | 0 | 13 |
| Laws | Lack of legal laws and lawsuits related to remote health | 3 | 2 | 1 | 2 | 1 | 9 |
| Permissions | Uncertainty of organizations and processes related to licensing | 6 | 3 | 2 | 3 | 0 | 14 |
| Differences in standards | Use of various standards, platforms, programming languages, and software | 4 | 2 | 0 | 2 | 0 | 8 |
| Infrastructure | |||||||
| Lack of trained personnel | Lack of distance health education in the training curriculum of health care personnel and shortage of trained personnel | 5 | 0 | 3 | 1 | 1 | 10 |
| Communication equipment | Lack of facilities such as video conferencing and examination and monitoring devices | 4 | 3 | 3 | 2 | 4 | 16 |
| Location and space | Lack of space and rooms for providing remote care services in hospitals | 2 | 1 | 2 | 2 | 0 | 7 |
| Internet network | Internet and national internet infrastructure | 5 | 3 | 4 | 2 | 5 | 19 |
| Information security | |||||||
| Privacy | Patients are concerned about publishing their information in cyberspace | 4 | 2 | 3 | 2 | 6 | 17 |
| Confidentiality | Concerns about hacking and publishing information due to security vulnerabilities | 4 | 2 | 2 | 2 | 6 | 16 |
| Information storage | Lack of proper servers to store information | 4 | 1 | 0 | 1 | 0 | 6 |
| Socio-cultural | |||||||
| Technology literacy | The inability of patients and the elderly to use new information technologies | 3 | 2 | 2 | 2 | 5 | 14 |
| Health literacy | Low level of health literacy of the elderly and patients | 3 | 2 | 4 | 1 | 5 | 15 |
| Religion | Religious attitudes about connecting with other people | 1 | 1 | 0 | 0 | 3 | 5 |
| Lack of effective communication | Lack of recognition of body language, stress, and moods through THC | 3 | 1 | 2 | 1 | 6 | 13 |
| Resistance treatment staff | Non-acceptance of THC by the treatment staff | 4 | 2 | 3 | 2 | 0 | 11 |
Barriers to Implementing and Developing Telehomecare
5. Discussion
This study aimed to investigate the challenges of implementation and development of THC in Iran. Based on the findings of this study, five challenges in this field were identified. One of the most important challenges in the implementation of n THC is the financial costs imposed on patients, healthcare providers, and healthcare organizations.
Akiyama and Abraham’s study in Japan also showed that THC is somewhat cost-effective for the elderly, but in some cases, the cost is way more than a face-to-face visit (6). In line with the results of the present study, Guillen also points to the high cost of THC technology for patients (23). In another study, it was acknowledged that when providing services THC, medical staff should be responsive to patients or their companions on a 24 - 7 basis, which can increase the costs of health care organizations (3).
The costs imposed on patients are mostly due to the purchase of THC equipment. In addition to providing some of these costs by insurance companies, providing these simple services based on smartphones, renting and lending the necessary equipment by starting organizations, and reducing the cost of the Internet for patients can be a good way to reduce the costs imposed on patient. Increasing the amount of reimbursement to the health care team, due to the increase in workload and the need for additional training can be another way to reduce the costs imposed. This funding can come from reducing the number of physicians’ missions or saving on public transportation and air pollution costs, as well as reducing office staff and maintenance costs for health centers.
The second challenge identified is rules and standards, which were divided into four categories: Repayment rules, lawsuits related to lawsuits, licenses, and differences in standards. Burkow et al.’s study also addresses repayment problems as a challenge to providing telecare services (24). Almathami et al. and Benton et al. also cited the lack of distance health legislation as a challenge (25, 26).
It seems that the most important factor in causing these problems is the lack of clear health coverage. Lack of coordination between different organizations and councils on the one hand and the multiplicity and alignment of different organizations has caused problems in this area.
Infrastructure problems were another implementation challenge for THC. In his study, Scott considers employee-related technical challenges to be the most important barrier to the implementation of THC (27). Another study showed that technology infrastructure and its incompleteness is an important challenge to use THC (25). The Ehlers et al. and Green et al. study also found that the lack of a suitable physical environment to provide telehealth services could be a major challenge (28, 29). In other studies, is clear that the internet with low speed is the biggest problem for THC implementation (30-33).
In the field of soft infrastructure, which is related to human resources, the lack of educational content during the university, and also the lack of related workshops during work in the hospitals can be one of the most important reasons. The delay in completing the national information network is the biggest cause of implementation infrastructure problems THC in Iran. It seems that the implementation of this project can solve many infrastructural problems.
The security challenge in this study was divided into three groups: Privacy, confidentiality, quality, and information storage. In studies, patients’ concern for privacy when using THC is very significant (29, 30, 32). Also, the confidentiality of information is a major challenge for providing remote health services (29, 32). Jeddi et al. say for continuity of care in THC gathering data in different forms and sources, and sharing data with registration centers and national banks as well as electronic health records is essential (1).
When designing software and using hardware, care should be taken to ensure that the maintapatientt’s privacy and others used, using new technologies and new encryption methods to ensure the necessary confidentiality and security. Using new storage techniques such as cloud servers and powerful servers can solve these concerns.
Based on the findings of this study, socio-cultural problems were divided into five groups: Technology literacy, health literacy, religion, lack of effective communication, and resistance of treatment staff. In line with the results of this study, Scott acknowledged that the level of education of patients is one of the main challenges in the use of telemedicine (27). Peel also argues that patients need help to use THC because of their low level of health literacy (34).
In addition to the cases mentioned in various studies that it is difficult for them to express their emotions through THC (28, 35). Also, in some studies, it was found that not using body language is considered a challenge for using telehealth (36, 37). In various studies, it was found the beneficiaries of using telehealth in resist the use of technology (26, 28, 38).
Education provided during education, familiarity with telehealth strengthening the IT skills of the community can reduce socio-cultural problems as much as possible and solve them over time. Solving challenges and explaining the benefits and holding training workshops can solve the problems of employee resistance.
It seems that in this study if people who have telehealth-related businesses were interviewed, more accurate and tangible information would be obtained. Also, because this study was conducted at the time of the corona outbreak, it may have an impact on the views of the interviewees.
5.1. Conclusions
This study aimed to identify the challenges of implementing and developing telehomecare. The findings of this study show that the implementation of this technology in Iran can face the five challenges of cost imposed, rules and standards, infrastructure, health information security, and socio-cultural as a. Some of these challenges can be addressed quickly by identifying a responsible organization and the right legislation. The second category of these challenges is related to cultural factors that must be solved with proper educational programs and information.
According to the findings of this study, determining the organization in charge of providing telehealth services and establishing a central council including all effective organizations in this regard can greatly reduce the existing challenges.