1. Background
Occupations are one of the main causes of psychological vulnerability (1). They form people's social identity, meet their needs, establish social relations, and are key sources of stress. There is more stress in jobs that involve human communication (2). Excessive work-related psychological pressures can endanger health by causing physical, mental, and behavioral complications (3). These pressures can also diminish the quality of work by threatening organizational goals (4). Emergency medicine physicians face stressful settings which are very difficult to work in as they are full of injured and critically ill patients (5). An important criterion for evaluating the health of society is its level of mental health, and the higher this level of mental health is, the more dynamic and efficient the society will be (6). Vulnerability is defined as congenital or acquired readiness for mental disorders and maladjustments, consisting of biological, cognitive, emotional, and social components known as vulnerability markers (7). One's inability to adapt to stressors and stressful situations leads to vulnerability. In fact, vulnerability is the risk of the occurrence of maladaptive responses in certain situations (8). According to some studies, the prevalence of mental harm in different societies ranges from 17.5 to 21.9% (9).
A variable that seems to contribute to psychological vulnerability among emergency medicine physicians is defense styles, i.e., the unconscious reactions of the ego, as a part of the personality, to reduce anxiety by changing the direction of perception of reality. These psychological defense states develop early in life. Through these processes, the ego attempts to get rid of anxiety caused by the conflict between the id and the superego (10, 11). Most scholars including Hsieh et al. (12) divide defense mechanisms into the three categories of mature, neurotic, and immature defense styles. Based on this classification, defense styles are arranged hierarchically, from very immature to very mature or from very maladaptive to very adaptive. The choice of defense styles plays an important role in understanding different responses to environmental stress and is the key to the conceptualization and treatment of mental disorders from a psychodynamic perspective (13). Many studies have supported the hypothesis that physical and mental health is significantly associated with their defense styles (14). Granieri et al. (15) reported that every mental disorder is associated with specific defense styles. Jiang and Qian (16) also found that defense styles are immature and maladaptive in people with mental disorders, while in the non-clinical population, defense styles are far more mature. According to Dimitrijevic (17), immature defense styles pose an obstacle to the perception of reality in people, deprive them of the possibility of rational and effective defense, and reduce their capacity for insight and self-exploration. Cavalera et al. (18) found a significant negative relationship between the degree of maturity of defense styles and psychopathology.
Studies show that some emergency medicine physicians have trouble identifying and integrating their emotions due to occupational pressures and stress (19). Consequently, instead of effective behaviors or coping techniques, they fall back on a wide spectrum of desperate escapes, e.g., impulsive or self-destructive measures (20). Emotion regulation is an inherent aspect of tendencies related to emotional responses. In fact, emotion regulation involves measures taken to alter or modify an emotional state (21). According to the literature, aggressive people suppress many of their emotional experiences and display higher levels of negative affectivity and social inhibition (22). Emotional inhibition and negative affectivity increase cortisol secretion and the activity of the hypothalamus-pituitary-adrenal axis, and disrupt the regulation of physiological responses to stress, all of which trigger anger and aggression (23). Studies show that adaptive emotion regulation is related to self-esteem and positive social interactions, and increased positive emotional experiences lead to effective coping with stressful situations and appropriate responses to social situations (24). Furthermore, cognitive emotion regulation has been shown to predict positive adjustment, and reappraisal, as an emotion regulation strategy, is associated with high levels of well-being and mental health (25).
Physicians working in high-risk hospital wards are exposed to mental pressure (26). When emergency medicine physicians are exposed to risky situations in the hospital setting, they experience extensive psychological pressure and physical, emotional, and social changes. Therefore, they become physically prone to heart diseases, emotionally prone to higher sensitivity in interpersonal relationships, aggression, anxiety, and depression, and socially and occupationally prone to frequent absenteeism. Moreover, the medical profession requires them to be patient and trustworthy and avoid expressing their disturbing feelings, which causes psychological problems.
2. Objectives
Accordingly, the present study aimed to investigate the mediating role of emotion regulation in the relationship between defense styles and psychological vulnerability among emergency medicine physicians.
3. Methods
The statistical population of this descriptive-correlational study comprised all emergency medicine physicians working in Tehran hospitals in 2021 - 2022. The population size was 950 according to the statistics, of which a sample of 380 was selected by cluster sampling. After checking the indicators and characteristics of the emergency departments of the hospitals, nine homogeneous hospitals were selected from 47 teaching hospitals affiliated with Shahid Beheshti, Tehran, and Iran Universities of Medical Sciences. Eighteen parameters were measured in the hypothesized model for the present research. According to Kline (27), a sample of 360 is sufficient for achieving acceptable results (using the 20 to1 rule); however, since some questionnaires were likely to be incompletely filled out, it was decided to include 420 participants. After examining the questionnaires that were completed by the participants, 380 of them were analyzed. The inclusion criteria were having at least one year of work experience in the emergency departments and no current or previous mental or physical disorders, and being willing to participate in the research. The exclusion criteria were unwillingness to participate in the study and incompletely filled-out questionnaires.
3.1. Study Instruments
Symptom checklist-25 (SCL-25): This 25-item checklist was administered to measure psychological vulnerability. It measures eight main factors (anxiety, obsessive-compulsive disorder, interpersonal sensitivity, somatization, psychosis, paranoid ideation, depression, and phobia) and another factor that includes additional items. The 25 items in this checklist are scored on a five-point Likert scale from not at all (0) to very high (4). The checklist evaluates the respondent's states during the last week. The total score is the sum of the scores of the nine factors and ranges from 0 to 100 (28). The reliability of this tool in the present study was confirmed using Cronbach's alpha (α = 0.86).
The Defense Style Questionnaire (DSQ): The DSQ was developed by Andrews et al. (29) based on the hierarchical order of defense mechanisms. Its 40 items are scored on a nine-point Likert scale (from strongly disagree to strongly agree) and evaluate 20 defense mechanisms at three levels of mature, neurotic, and immature. The mature style involves suppression, sublimation, humor, and anticipation; the neurotic style involves pseudo-altruism, reaction formation, idealization, and undoing; and the immature style involves rationalization, projection, denial, devaluation, acting out, somatization, autistic fantasy, splitting, passive aggression, displacement, and isolation. The reliability of the DSQ in the present study was confirmed using Cronbach's alpha (α = 0.79).
Cognitive Emotion Regulation Questionnaire (CERQ): Garnefski and Kraaij (30) developed the CERQ. It is an 18-item questionnaire evaluating cognitive emotion regulation strategies in response to threatening and stressful events on a five-point Likert scale from 1 (never) to 5 (always) based on the following four sub-scales for maladaptive strategies: Self-blame, other-blame, rumination, catastrophizing, and five subscales for adaptive strategies: Positive refocusing, planning, positive reappraisal, putting into perspective, and acceptance. Higher scores indicate greater use of that particular cognitive strategy by the individual. The reliability of the CERQ in the present study was confirmed using Cronbach's alpha (α = 0.90).
3.2. Statistical Analysis
The data were analyzed in SPSS 24 and Lisrel 7.80. Structural equation modeling (SEM) was performed to test the research hypotheses.
4. Results
Table 1 presents the descriptive characteristics of the variables in the research. As the values of skewness and kurtosis were in the range of (-1.96 to +1.96), the assumption of normality of the data distribution was confirmed.
| Variables | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|
| Psychological vulnerability | 56.47 ± 15.41 | -0.33 | -0.17 |
| Mature defense styles | 28.98 ± 8.56 | 0.59 | 0.46 |
| Neurotic defense styles | 39.18 ± 13.79 | 0.76 | 0.69 |
| Immature defense styles | 97.01 ± 31.33 | -0.27 | -0.14 |
| Positive cognitive strategies | 32.06 ± 9.51 | -0.17 | -0.43 |
| Negative cognitive strategies | 25.82 ± 7.21 | 0.22 | -0.30 |
Abbreviation: SD, standard deviation.
Table 2 demonstrates the correlations between research variables. Evidently, there were significant correlations between them (P < 0.001).
a P < 0.001.
According to the chi-square and root mean square error of approximation (RMSEA) criteria, the model provided a good fit to the data. Table 3 gives the most important fit indices. Since all the indices had statistical adequacy, it is certain that the model had a good fit to the data.
| Fit Indicators | χ2 | GFI | AGFI | CFI | RMSEA |
|---|---|---|---|---|---|
| Research model | 1328.20 | 0.98 | 0.95 | 0.96 | 0.058 |
Abbreviation: RMSEA, root mean square error of approximation.
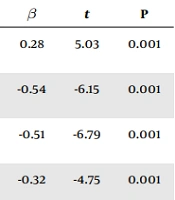
Table 4 lists the path coefficients along with the t-values for the direct relationships between the variables. Evidently, the direct relationships between research variables were significant (P < 0.001).
| Paths | β | t | P |
|---|---|---|---|
| Mature defense styles → positive cognitive strategies | 0.28 | 5.03 | 0.001 |
| Mature defense styles → psychological vulnerability | -0.54 | -6.15 | 0.001 |
| Mature defense styles → negative cognitive strategies | -0.51 | -6.79 | 0.001 |
| Neurotic defense styles → positive cognitive strategies | -0.32 | -4.75 | 0.001 |
| Neurotic defense styles → psychological vulnerability | 0.35 | 6.27 | 0.001 |
| Neurotic defense styles → negative cognitive strategies | 0.33 | 6.54 | 0.001 |
| Immature defense styles → positive cognitive strategies | -0.62 | -7.29 | 0.001 |
| Immature defense styles → psychological vulnerability | 0.56 | 8.24 | 0.001 |
| Immature defense styles → negative cognitive strategies | 0.49 | 7.11 | 0.001 |
| Positive cognitive strategies → psychological vulnerability | -0.42 | -5.50 | 0.001 |
| Negative cognitive strategies → psychological vulnerability | 0.37 | 4.82 | 0.001 |
There was an indirect relationship between the defense styles of emergency medicine physicians and psychological vulnerability, mediated by emotion regulation (P < 0.001). According to Table 5, the mature defense style indirectly affected psychological vulnerability through positive cognitive strategies. The mature style indirectly affected psychological vulnerability through negative cognitive strategies. The neurotic style had an indirect effect on psychological vulnerability through positive cognitive strategies. It also had an indirect effect on psychological vulnerability through negative cognitive strategies. The immature style indirectly affected psychological vulnerability through positive cognitive strategies. Finally, the immature style indirectly affected psychological vulnerability through negative cognitive strategies.
| Predictor Variables | Mediator Variables | Criterion Variables | β | P | Total Effect |
|---|---|---|---|---|---|
| Mature defense styles | Positive cognitive strategies | Psychological vulnerability | -0.12 | 0.001 | -0.66 |
| Mature defense styles | Negative cognitive strategies | Psychological vulnerability | -0.54 | 0.001 | 0.73 |
| Neurotic defense styles | Positive cognitive strategies | Psychological vulnerability | 0.35 | 0.001 | 0.48 |
| Neurotic defense styles | Negative cognitive strategies | Psychological vulnerability | 0.35 | 0.001 | 0.47 |
| Immature defense styles | Positive cognitive strategies | Psychological vulnerability | 0.56 | 0.001 | 0.82 |
| Immature defense styles | Negative cognitive strategies | Psychological vulnerability | 0.56 | 0.001 | 0.74 |
5. Discussion
This study aimed to investigate the mediating role of emotion regulation in the relationship between defense styles and psychological vulnerability among emergency medicine physicians. An indirect relationship was found between the defense styles of the emergency medicine physicians and psychological vulnerability, mediated by emotion regulation. The immature defense style had a positive (direct) relationship with psychological vulnerability; this means that the psychological vulnerability of emergency medicine physicians increased when they used immature defense styles, whereas their psychological vulnerability decreased when they used mature defense styles. These results are in line with the findings of Abolghasemi et al. (31) who showed that, compared to other people, people with psychological vulnerability and those with poor mental health used more immature and neurotic defense mechanisms to deal with threats. Everyone may sometimes use a variety of defense mechanisms to deal with psychological vulnerability and stressful situations; still, excessive use of immature and neurotic defense mechanisms can cause different mental disorders, including anxiety.
Adaptive defense styles are associated with physical and mental health outcomes, whereas maladaptive defense styles are related to negative health indicators such as anxiety and depression. Since, in the mature defense style, the feeling of individual satisfaction and happiness is maximized and the conscious awareness is filled with feelings, ideas, and their outcomes, this style is associated with optimal adaptation in managing stressors and, therefore, in reducing psychological vulnerability. Unlike the other defense styles, the mature defense style does not deny or distort, but rather reduces, the source of conflict (14). As such, the less use of mature defense by people with psychological vulnerability is associated with the feeling of anxiety or fear in stressful situations, e.g., disease and disability. When the dominant defense styles are neurotic and immature, people often face negative emotions and stressful situations through suppression, denial, undoing, and neglecting (10). In the meantime, psychological symptoms such as anxiety and depression are the outcome of suppressing and denying painful and negative emotions and failing to face, identify, perceive, and express them.
The positive relationship between negative emotions and the use of immature and neurotic defense styles can be explained in terms of the relevant concepts. People with a high ability for cognitive emotion regulation can manage their emotions with greater psychological adjustment and use adaptive mechanisms. As such, those who use maladaptive cognitive regulation strategies, e.g., catastrophizing and other blame, are more exposed to emotional problems, e.g., psychological vulnerability (anxiety and depression) (21). On the other hand, people who use adaptive cognitive emotion regulation strategies, e.g., positive reappraisal, putting into perspective, and acceptance, are less vulnerable to emotional problems such as anxiety. Apparently, people who have maladaptive emotion regulation strategies and low emotional distress tolerance are more prone to psychological vulnerability and distress in the face of severe stress. Due to their failure to recognize their emotions and feelings correctly, they lose the ability to adopt accurate, reasonable, and reality-based behaviors to alleviate their psychological vulnerability and stress. These people also have trouble using their emotions correctly (24). Furthermore, since cognition, emotion, and behavior interact, cognitive emotion regulation changes the function of cognitive systems and mitigates psychological vulnerability by controlling attention and cognitive outcomes of emotion.
Based on the results, adaptive emotion regulation strategies had a significant positive relationship with the mature defense style and a significant negative relationship with neurotic and immature defense styles. Maladaptive cognitive emotion regulation strategies also had a significant negative relationship with the mature defense style and significant positive relationships with neurotic and immature defense styles. These findings are consistent with the results of previous studies (32, 33). Overall, emotion regulation strategies and defense mechanisms are both functions of the ego in the integrated structure of personality, and the ego serves as the link in this relationship. Based on Freud's conceptualization, the ego is an organizing structure of personality; with cognitive functions including thinking, memory, and language, the ego communicates with the outside world and regulates internal impulses to respond to external expectations and realities. Thus ego, as the organizer of personality, possesses functions and responsibilities and is considered strong and mature if these functions are carried out optimally and efficiently. The strength of the ego is manifested in the ability to cope with and regulate adaptive emotions. The strength of ego, which needs to be examined in diagnosis and treatment, includes indicators of emotional resilience, impulse control, pain and failure tolerance, abstract and symbolic thought, and use of psychological (instead of physical) pathways for emotional discharge which, together, demonstrate the ability to cope effectively.
The present study had some limitations. The research design was cross-sectional, and the sample was limited to emergency medicine physicians in Tehran. The results should thus be generalized with caution. Moreover, self-reports were used to collect data, which may lead to bias in the results.
5.1. Conclusions
Emotion regulation mediated the relationship between the defense styles of emergency medicine physicians and psychological vulnerability. Therapists should, therefore, teach emotional regulation skills and mature defense styles to people with high psychological vulnerability and focus their treatment on training skills to control and deal with painful and difficult emotions and behaviors. Acquisition of these skills helps people recognize their emotions, realize how these emotions affect their lives, and learn how they can successfully adapt to them. It is also recommended that mental health professionals incorporate the findings of this study into their clinical measures to promote the mental health of emergency medicine physicians.