1. Context
The information showed that even after the production of the SARS-CoV-2 vaccine and the decreasing trend of the disease, on November 2021, South Africa scientists have announced the worrying new variant of Omicron to the World Health Organization (WHO) (1). Then one week later, in all six WHO regions, the WHO reported Omicron in 38 countries (2). On November 13 and 18, 2021, two patients became infected with Omicron while traveling (3). The Islamic Republic of Iran reported its first Omicron case in February 19, 2020 in the city of Qom (4). Therefore, studies and reports show that Omicron is spreading worldwide, highlighting the need for immediate action.
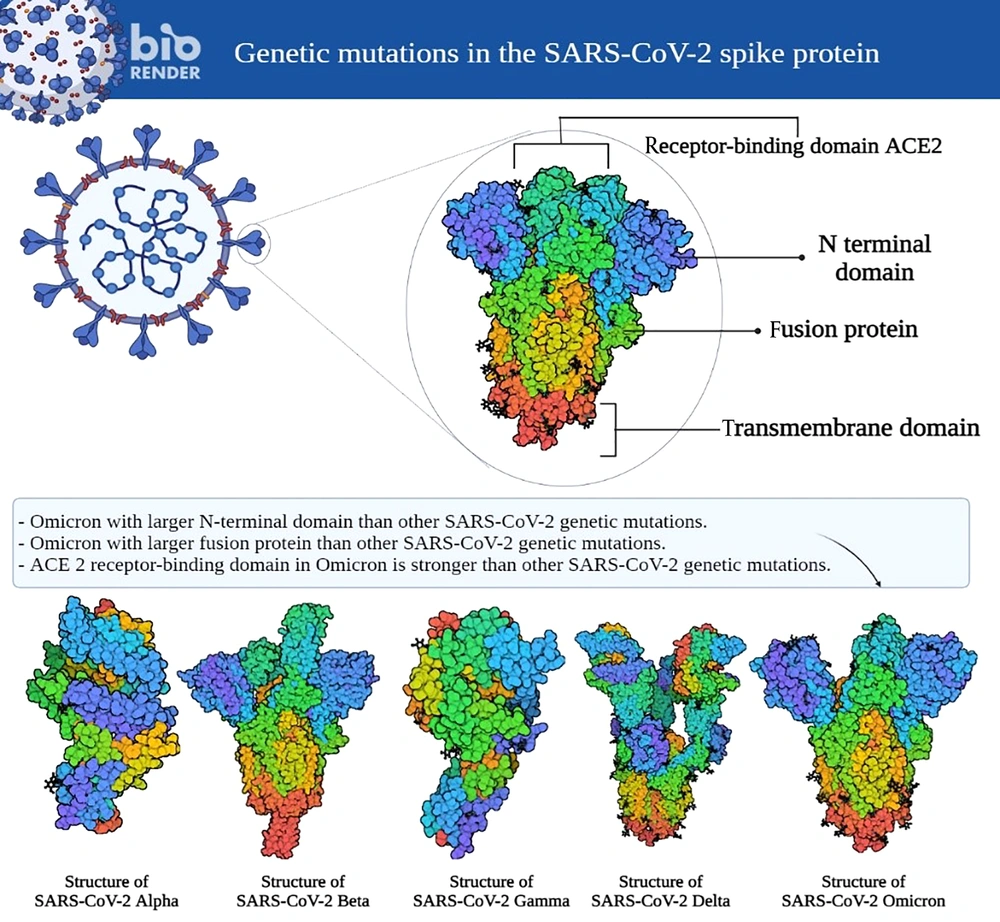
Omicron has 50 genetic mutations, of which about 26 to 36 are related to COVID-19 spike protein (5). These mutations increase the virus transmission, disease severity, and immune escape (5). Another reason why Omicron could be a dangerous virus is the receptor-binding domain (RBD) (5). RBD is a validated viral entity that detects Angiotensin-converting enzyme 2 (ACE2) receptors as a virus entry mediator (5). Notably, RBD is the main target for neutralizing antibodies (5). Mutations in the coronavirus at the 484 and 417 spike positions are associated with immune escape (6, 7). Since the Omicron type contains the E484A and K417N mutations, it could also resist antibodies and have a robust immune escape property (7) (Figure 1).
New findings have shown that vaccinated people are about three to four times more likely to get the virus if a family member becomes infected with Omicron (8). Studies reported that Omicron can be an indicator of SARS-CoV-2 virus (9). Mutations in the Omicron make it more infectious than previous nasopharynx and upper respiratory tract variants (10). Conversely, it is less likely to penetrate deep into the lungs (11). Protection against Omicron is less than other variants in affected and vaccinated individuals (12). Recent data suggest that re-infections are more likely to occur in the Omicron type (13). The latest COVID-19 strain, appears to be a potentially serious threat, and so far, no new and more dangerous strain than Omicron has been reported (14). Hence, developing the necessary strategies during this disease can be very effective. It has been reported that the Omicron can pass just in first line of defense in body (15); thus, T cells have been emphasized in the fight against this new variant (12). In line with this, T cell responses are associated with reduced disease symptoms (16, 17). Two primary interventions can increase T cells without side effects: regular physical activity practice and good diet (12, 18).
Based on studies, it seems that in addition to regular physical activities, a proper diet has a favorable effect on the management of COVID-19. So that a proper diet can help improve immune system by increasing the level of proteins, vitamins, and gut microbiota (19). Also, diverse and especially Mediterranean diets can lead to a reduction of free radicals. These researchers stated that diets containing antioxidants are associated with improving the function of the immune system, reducing inflammatory factors, and reducing oxidative stress (20). In another study, researchers reported that receiving a diet containing various vitamins such as C, E, D, zinc and the B family can inhibit TLR toll-like receptor, nuclear factor kappa-light-chain-enhancer of activated B cells. NFκB), tumor necrosis factor (TNF) and in this way inhibit the inflammatory pathways of viruses and especially COVID-19 (21).
Although exercise and proper diet have favorable effects on the immune system and health; But in the conditions of the Corona pandemic, which plunged the world into a deep dilemma. It is necessary to provide practical and non-invasive solutions for the prevention and treatment of this disease. Therefore, the current study was conducted with the aim of investigating the effect of exercise and diet on health in the conditions of the COVID-19 pandemic.
2. Evidence Acquisition
2.1. Increase Physical Activity to Counteract Omicron Dissemination
Several studies were published emphasizing staying active to improve the immune system (18, 22-24). Further studies reported low intensity training (LIT) to moderate intensity training (MIT) home-based exercise can improve the functioning of the antioxidant system and the immune system (18, 25, 26). Despite the recommendations for the population to remain physically active, the level of physical activity decreased significantly in the coronavirus outbreak (27). After the rules of social distance were relaxed, the level of physical activity did not return to pre-pandemic levels (28). However, new variants made the situation worse because they have been more resistant to immunization and can escape the immune system (29). These properties reach the highest levels in the Omicron, making it the most dangerous variant (4). Studies have shown that exercise training such as MIT home-based exercise could increase T cells, the essential part of the immune system in fighting against the Omicron (30). Doing this could bring two advantages together: First, social distancing, and second, boosting T cells (31). Physical exercise depended on type, intensity and frequency can improve the immune system in COVID-19 disease (32). It seems that low- and moderate-intensity sports activities have favorable effects on the immune system in dealing with COVID-19 by modulating the lymphocytes, pro-inflammatory and inflammatory cytokines, and regulating the expression of interferon 1 (33). So physical exercise should be commensurate with the nature of COVID-19 to prevent recurrence of infection or impaired immune function (26, 30, 34). It is recommended that children and adolescents between 5 and 17 years perform MIT (60 minutes, about 70% of heart rate maximum, three sessions per week) (35). For adults over 17 years, MIT (75 minutes of twice a week) can be effective as well. These exercises can include dancing, Zumba, stationary bike, treadmill ruining and rope (36). The latest update of physical activity recommendations for COVID-19 states that 3 - 5 sessions per week MIT for COVID-19 states that performing 3 - 5 sessions per week MIT for 150 minutes is needed in the COVID-19 situation (37). Also, resistance training could bring extra advantages. Thus, we suggest doing the following: Box squat, hip bridge, push-up, handstands, tight hang, mountain climbers, split squat, floor push-up, and Bulgarian split squat (38). To maintain the intensity of the exercise with bodyweight, use the Borg Scale of 5 and the repetitions between 10 to 20 and 2 - 3 sets. With the increase in the prevalence of Omicron, the outdoor environment cannot be safe (39). Therefore, we suggest exercising at home by combining aerobic and resistance training.
Table 1 summarized our sessions for exercise training during Omicron outbreak. Also, Table 2 provides an overview of studies related to physical activity and the immune system.
| Exercise Type a | Age, y | Volume | Intensity |
|---|---|---|---|
| Cycling | 40 - 59 | 2 sessions per week | 45 - 55 of VO2max |
| Run | 40 - 59 | 3 sessions per week | 45 - 55 of VO2max |
| Yoga | 40 - 59 and more than 60 | 3 sessions per week | N/A (unknown) |
| Elastic bands | More than 60 | 2 sessions per week | Borg scale 2 - 5 (scale 1 to 10) |
| Resistance training | 40 - 59 people without heart disease | 3 sessions per week | 40 - 60 of 1RM |
| Walking | 40 - 59 and more than 60 | 3 sessions per week | 35 - 45 of VO2max |
a Before exercising, make sure you do not have a cold or an infectious disease.
| Author | Year | Description | Suggested Exercise | References |
|---|---|---|---|---|
| Clemente-Suarez et al. | 2022 | MIT increased T cells and NK-cells Improvement in mental health, metabolic markers and cardiorespiratory fitness in patients Improvement of antibody responses in vaccination | Regular and MIT | (37) |
| Agha-Alinejad et al. | 2022 | Impaired immune function by high intensity training (HIT) Increase T-cells by MIT to fight COVID-19 Less inprovment in immune system function by LIT | Regular and MIT | (34) |
| Jesus et al. | 2021 | Preventing viral respiratory infections (including coronavirus infection). MIT can improve immune system function (increase in T cells), nevertheless HIT can deteriorate the immune system function. | Regular and MIT | (40) |
| Scudiero et al. | 2021 | HIT can destroy immune system (by creating numerous pathologies), nevertheless MIT can help the human body to live better | Regular and MIT | (41) |
| Sacma and Geiger | 2021 | Exercise, by increase in production of immune cells from the bone marrow, the regular trainings can increase the immune system function. | Regular and MIT | (42) |
| Suzuki and Hayashida | 2021 | HIT can increase the systemic inflammation, MIT can reduce the acute upper respiratory infections and enhance immune function. Yoga and walking trainings (as LIT) can relieve stress and are not harmful for immune system. | Regular and MIT | (27) |
| Yoon et al. | 2021 | Regular trainings can improve anti-inflammatory cytokines. Decrease TNF as well as increase NK, B and T cells. | Regular and MIT | (43) |
| Simpson and Pawelec | 2021 | The mechanical load should be adjusted in such a way as to prevent suppression of the immune system, because the decrease in the function of the immune system in the elderly has a significant relationship with T cells. | Regular and MIT | (44) |
| Moghadam et al. | 2021 | Although diet can be one of the most effective and best ways to improve the functioning of the immune system, regular trainings with appropriate intensity can progress the immune system function. | Regular and MIT | (45) |
| Do Brito Valente et al. | 2021 | Trainings can decrease TNF as well as increase NK, B and T cells. Regular trainings by alteration in myokine concentrations and metabolites also modulation of the immune system can directly improve the systemic inflammation. | Regular and MIT | (46) |
| Papp et al. | 2021 | Regular training with the increasing in NKT, NK, B and T lymphocytes is a strong support to prevent viral infections. | Regular and MIT | (47) |
| Suzuki | 2019 | HIT can weaken the immune system and increase inflammation. MIT can improve the immune system. Exercise can be a drug. | Regular and MIT | (48) |
| Baker and Simpson | 2021 | MIT can prevent the spread of viral infections by increasing anti-inflammatory cytokines and T cells, as well as improving immune function. | Regular and MIT | (49) |
| Khoramipour et al. | 2021 | Exercise along with a balanced diet and proper nutrition can be essential factors to be safe in the pandemic. | Regular and MIT | (18) |
| Ahmadi Hekmatikar et al. | 2021 | The breathing trainings and low-intensity resistance training with hand-trainer can progress the strength performance and restore normal blood oxygen levels in patients with COVID-19. | Regular and MIT | (30) |
| Jee | 2021 | MIT can improve immune function, however HIT can suppress immune system, LIT could not improve immune function. | Regular and MIT | (50) |
| Valizadeh et al. | 2021 | In patients with hypertension, the submaximal endurance training lowered blood pressure and improved function of immune system | Regular and MIT | (51) |
| Oh et al. | 2021 | Vitamin D as well as regular MIT by increasing NK cells can improve the immune system function. | Regular and MIT | (52) |
| Córdova Martínez et al. | 2021 | Appropriate training programs can improve quality of life and recovery of patients with COVID-19 disease. | Regular and MIT | (53) |
| Rahayu et al. | 2021 | Regular trainings are more effective. Regarding to safe and positive effects of MIT, they are recommended in COVID-19 pandemic. It is better to increase the duration of trainings from 150 to 300 minutes to 200 to 400 minutes per week. | Regular and MIT | (54) |
| Domin et al. | 2021 | Release of the cytokines can be affected by duration and intensity of trainings so that prolonged trainings and single bout trainings have different effects on cytokines. | Regular and MIT | (55) |
| Fonseca et al | 2021 | MIT can improve cytokines such as leptin, sTNFR1 and IL-6. | Regular LIT and MIT | (56) |
| Scheffer and Latini | 2020 | Regular and MIT have anti-inflammatory properties which decrease TNF and increase B and T cells. | Regular LIT and MIT | (57) |
| Scartoni et al. | 2020 | Performing 150 minutes MIT or 75 minutes HIT per week is recommended to reduce the sedentary lifestyle. | Regular LIT and MIT | (58) |
| Simpson et al. | 2020 | MIT have safe and positive effects in patients who are recovering from COVID-19. | Regular LIT and MIT | (59) |
| Da Silveira et al. | 2020 | regular trainings can improve NK cells, monocytes, immature B cells and lymphocytes in patients with COVID-19. | Regular LIT and MIT | (33) |
| Aktuğ et al. | 2020 | MIT can pervent viral respiratory infections and inflammation in patients wit cardiovascular and T2DM diseases Long and HIT can decrease the immune system function. | Regular LIT and MIT | (60) |
| Wang et al | 2020 | Trainings can decrease TNF as well as increase NK, B and T cells. Regular trainings can improve the immune system. | Regular LIT and MIT | (61) |
| Yildizgoren | 2020 | Combination of balance, stretching, strengthening and walking trainings can be designed as home based trainings. In safe distance situation, the MIT like brisk walking outdoors can be a good alternative. Avoid from HIT in crowded and hall places as it has less benefits than risks. Consumption of vitamin rich fluid and nutrients prior to training along with balanced diet is important. | Regular LIT and MIT | (62) |
2.2. Can Diet Be Helpful as Well?
Several papers have highlighted the importance of a healthy diet during COVID-19 outbreak, because of its effects on the immune system (21, 63, 64), the interaction between diet and microbiota (including the gut, saliva, and lung microbiome)-which could affect CD4+ regulatory T cells (63), It has been shown that healthy gut microbiota can control the SARS-CoV-2 induced lung infection via a phenomenon called ‘gut lung axis’ (65). A high-fiber diet can affect the gut and lung microbiotas (66). In contrast, a low fiber, high fat/carbohydrate diet can lead to gut dysbiosis (67), attenuating the immune system. Studies have demonstrated that dietary carbohydrates (68), certain probiotics (69), artificial sweeteners (70), and emulsifiers (71) could weaken immunity responses and cause inflammation in mice. Also, high-sugar diet consumption may rises the pro-inflammatory regulation of body, negatively affects genus Lachnobacterium, disrupting balanced mucosal, and finally resulting in systemic inflammation (72) While a diet rich in saturated fats reduces the beneficial microbes such as Bifidobacterium or Faecalibacterium in the human gastrointestinal tract, unsaturated fats can reduce harmful microbes, including Escherichia and Streptococcus (73).
Probiotics can work with different immune cells and have important role in balance of immunogenic homeostasis of gastrointestinal tract (74). Another function of probiotics includes maintaining intestine pH, which impacts the composition of the microbial communities present in the gastrointestinal tract and lowers the invasion by the pathogens. Furthermore, probiotics act as prophylaxis and have the potential for adjunct therapy in individuals suffering from COVID-19 (75). Consumption of prebiotics such as polydextrose, inulin and maize fiber in elderly individuals can progress the immunity, digestion and gut microbiota diversity (76). It has been reported that dietary fibers and prebiotics may rise the short-chain fatty acids of butyrate, propionate and acetate which can stimulate the growth of bacterial species such as Bifidobacteria and Lactobacilli (77). Furthermore, microbiome composition and immunity are also affected by diet timing (78). Collado et al. concluded that taking meal at 17:30 instead of 14:30 (as late meal) is associated with the presence of pathobiont microbiota (79).
The foods full of probiotics, fruits, vegetables, legumes and grains as anti-inflammatory, balanced and healthy diets are the primary modulators in protecting the immune response and healthy gut microbiome (80). Beside probiotics, it has been reported that anti-inflammatory regimen can improve viral respiratory disease (80). The Mediterranean diet is well known as anti-inflammatory diet. This diet is reduced meat consumption as well as full of legumes, fruit, whole grains, vegetables, olive oil and fish. Indeed essential vitamins and minerals have immunomodulatory and anti-inflammatory property (81). The foods containing of bioactive polyphenols have anti-thrombotic, anti-inflammatory and antioxidant properties. Mediterranean diet has been recommended for treatment of COVID-19 infection (82-84). Also zinc, vitamin D, garlic, omega 3 fatty acids, vitamin C, onion, ginger, and saffron have anti-inflammatory have shown potential in their anti-inflammatory effects (85).
3. Conclusions
While widespread vaccination has been helping to reduce COVID-19 casualties, this new variant seems to pass the immune system making vaccination less effective. After introducing the vaccine, people quit other helpful interventions such as diet and physical activity practice, hoping for the vaccine effectiveness. However, relying on the vaccine alone cannot guarantee immunity. To this end, we highlight the importance of staying active and having a healthy/enriched diet along with vaccination to help us fighting more effectively against Omicron.
3.1. Highlights
Foods with anti-inflammatory properties can be used for treating and preventing viral respiratory disease.
The Mediterranean diet is well known as anti-inflammatory diet.
Moderate intensity training have beneficial effects on immune system in COVID-19.