1. Background
Hard of Hearing is a prevalent and intricate sensory impairment influencing a significant number of individuals (1). The prevalence of hard of hearing individuals at birth is estimated to be approximately one to six individuals per thousand live births (2, 3). Deaf and hard of hearing individuals require additional healthcare and mental health support compared to individuals with normal hearing. If their caregivers are unable to meet their needs, their lives can become challenging. The ability of a mother to cope with her child’s hard of hearing condition affects her life in various ways. Mothers who possess greater self-confidence also contribute to better emotional and psychological adjustment (4). Some major difficulties including education about risk avoidance, overcoming despair, coping with negative emotions, and supporting their child’s development of communication skills have been reported among parents who have children with hearing difficulties. These challenges serve as the sources of problems related to mothers of hard of hearing children (5).
If mothers of children who are hard of hearing do not employ essential strategies, they may encounter emotional challenges and heightened distress, which can adversely affect both the child and the parents. To address these challenges, integrated interventions based on mindfulness and spiritual therapy deserve attention, as they can help alleviate distress and enhance the psychological hardiness of both the child and the parent. Mindfulness entails a state of conscious awareness characterized by being fully present in the moment, purposeful, non-judgmental, and encompassing various aspects of mental health and well-being (6). Moreover, mindfulness involves paying attention to and verbally articulating emotions, enabling emotional purification and fostering emotional sharing. Research suggests that emotional sharing diminishes negative and enhance positive emotions (7).
Mindfulness-based interventions are recognized as a prominent component of the third-wave or third-generation cognitive-behavioral therapies. Through the application of these techniques, individuals can disengage from automatic patterns and modify their responses to thoughts, emotions, and bodily sensations (8). Over the past two decades, a plethora of mindfulness-based interventions and treatments have emerged including mindfulness-based anxiety reduction and mindfulness-based cognitive therapy (9). These interventions entail focused attention exercises, where individuals deliberately direct their attention to a specific stimulus, such as the breath or bodily sensations, for a designated period (10).
Mindfulness techniques have demonstrated their efficacy in facilitating muscular relaxation and alleviating concerns, stress, and anxiety (10, 11). Mindfulness seems to lie in attentional self-regulation, whereby repetitive concentration on a neutral stimulus, such as the breath, establishes an optimal attentional setting (12). Within the Western framework of mindfulness, acceptance constitutes a fundamental principle (13).
The integration of mindfulness and spiritual therapy appears to hold promise in benefiting mothers of hard of hearing children. To develop such an approach, it is advisable to leverage the shared principles between Western mindfulness concepts and Islamic spiritual teachings. Numerous theoretical and empirical articles have demonstrated that the inclusion of religion and spirituality in conjunction with other treatments can enhance their effectiveness (14-16). Some research supported the notion that spiritual interventions can amplify the effects of other treatments (17). Furthermore, a mindfulness integrated with spiritual therapy has consistently exhibited effectiveness in previous research studies (18). These integrative mindfulness-based therapies draw upon Eastern Buddhist psychology to address psychological problems and mental illnesses (19). Mindfulness-based approaches have demonstrated effectiveness in reducing anxiety, depression, and substance abuse (20, 21), improving psychological symptoms, enhancing quality of life (22), and promoting mental and physical well-being (23).
Studies have indicated that individuals with increased psychological hardiness experience lower levels of anxiety related to treatment (24). The psychological hardiness and distress tolerance of mothers who have hard of hearing children, combined with the multitude of behavioral challenges they face, the lack of social, educational, and financial resources, and the psychological pressures they encounter, give rise to numerous risk factors for both the parents and the children. Therefore, there is a need to explore integrative intervention approaches that mindfulness integrated with spiritual therapy to facilitate and support parents in addressing these challenges.
2. Objectives
The present study aims to investigate the effectiveness of mindfulness integrated with spiritual therapy in enhancing distress tolerance and psychological hardiness among mothers of hard of hearing children.
3. Methods
The present quasi-experimental research study incorporates a pretest-posttest with a two follow-up stages and a control group. The implementation of the program consists of several stages: (1) random selection of participants from the research population, (2) random assignment of participants to groups, (3) administration of a pretest and data collection, (4) intervention including mindfulness and spiritual therapy for the experimental group, (5) administration of a posttest and data collection, and (6) conducting a follow-up test and data collection after one- and two-month intervals (Table 1).
| Sampling | Groups | Pretest | Intervention | Posttest | One Month Follow-up | Two Months Follow-up |
|---|---|---|---|---|---|---|
| R | Experimental | T1 | Mindfulness integrated with spiritual therapy | T2 | T2 | T2 |
| R | Control | T1 | No intervention. Waiting list | T2 | T2 | T2 |
Study Design Protocol
The statistical population of this research comprises all parents of hard of hearing children attending family centers, centers for hard of hearing children, and audiology clinics in Kermanshah during 2020 to 2021. A total of 60 mothers were selected using convenience sampling method. The inclusion criteria entailed having a child with hard of hearing that was not amenable to treatment through medication or surgery, necessitating specialized rehabilitation services for educational and social development. The children had to be between the ages of three and five, only one child with hard of hearing in the family, diagnosed prior to the language acquisition critical period and having received appropriate auditory training for at least two years. Moreover, the parents were required to have effective communication with the family centers and their hard of hearing child, demonstrating good cooperation in this context. The exclusion criteria involved emotional issues between parents based on their reports and complaints, and the presence of another physical disabilities in the child. Subsequently, the participants were randomly assigned to either an experimental group receiving mindfulness integrated with spiritual therapy (n = 30) or a control group (n = 30). Participants assigned to the control group, as well as mothers who demonstrated low distress tolerance and psychological hardiness but were unable to attend the therapy sessions due to limitations in the sample size, were placed on a waiting list for treatment. Before the treatment, participants performed two questionnaires which measured distress tolerance and psychological hardiness. This research consisted of conducting eight sessions of mindfulness, which adhered to the Kabat-Zinn protocol and the group spiritual therapy protocol. These sessions encompassed eight psychological-spiritual components, namely reliance and surrender to God, supplication and prayer, gratitude, patience and tolerance, forgiveness and letting go of anger, connecting with God and engaging in innerdialogue, self-awareness and attuning to inner calling, reading sacred texts, and utilizing spiritual and religious literature. Following the completion of the therapy sessions, a posttest was administered to the experimental group to assess the sustainability of treatment effects. The first follow-up stage was conducted one month after the treatment, with the second follow-up stage taking place two months later.
3.1. Measures
The Distress Tolerance Scale (DTS) is a 15-item scale developed by Simmons and Gaher to assess an individual’s ability to tolerate emotional distress. It evaluates various aspects such as the individual’s cognitive appraisal of distress, their level of attention to negative emotions when they occur, and the strategies they employ to regulate and alleviate distress. The scale utilizes a five-point Likert scale for scoring, with a score of one indicating complete agreement with the item and a score of five indicating complete disagreement. Based on confirmatory factor analysis, the researchers confirmed the existence of four primary factors: Tolerance (reflecting an individual’s inability to effectively cope with their distress), Absorption (referring to the tendency of constantly thinking about one’s negative emotions when feeling distressed and upset), Appraisal (capturing the perception of distress and upset as highly challenging), and Regulation (indicating the willingness to employvarious strategies to prevent the emergence of intense emotions). The Cronbach’s alpha reliability estimate for the DTS was 0.672, indicating good internal consistency. The test-retest reliability coefficient for the overall scale was 0.810, and for the subscales of Tolerance, Absorption, Appraisal, and Regulation, the coefficients were 0.710, 0.690, 0.770, and 0.730, respectively.
The Ahvaz Hardiness Inventory (AHI) is a self-report pencil-and-paper inventory comprising 27 items. It was developed by Kiyamarsi, Najarian, and Mehrabizadeh, 1998. The inventory provides a total score representing individuals’ hardiness and does not include components of commitment, control, and challenge. Scoring for the 27-item inventory involves respondents selecting one of four options (Never, Rarely, Sometimes, and Often), which are assigned scores ranging from 0 to 3, respectively. Notably, items 21, 17, 13, 10, 7, and 6 in this inventory indicate high psychological hardiness in individuals. To assess the reliability of the AHI scale, Najarian and colleagues employed the test-retest and internal consistency methods. The correlation coefficient between the test and retest, with a six-week interval, was reported as 0.84 for female participants and 0.85 for male participants in a sample of 119 individuals. For internal consistency, the Cronbach’s alpha coefficient was calculated for the psychological hardiness inventory, resulting in a value of 0.76, indicating a highly acceptable coefficient.
3.2. Statistical Analysis
For the purpose of data analysis and hypothesis testing in this study, two statistical methods were employed. At the descriptive level of the initial sample, various measures including frequency and percentage, mean and standard deviation, as well as minimum and maximum values were utilized. Furthermore, at the inferential level, the statistical technique of repeated measures analysis of variance (ANOVA) was applied using the SPSS version 23 software.
4. Results
Sixty mothers with the age range of 19 to 48 years (Mean; 36.65, Standard deviation; 4.12) were participated in the study.
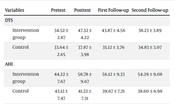
Descriptive data including the means and standard deviations of both DTS and AHI in the experimental and control groups at the pre-test, post-test, first follow-up, and second follow-up stage is presented in Table 2.
| Variables | Pretest | Posttest | First Follow-up | Second Follow-up |
|---|---|---|---|---|
| DTS | ||||
| Intervention group | 34.52 ± 2.87 | 47.32 ± 4.22 | 43.87 ± 4.56 | 38.23 ± 3.89 |
| Control | 33.64 ± 2.65 | 37.87 ± 3.98 | 35.12 ± 3.76 | 34.83 ± 3.07 |
| AHI | ||||
| Intervention group | 44.22 ± 7.67 | 58.78 ± 9.67 | 56.12 ± 9.33 | 54.29 ± 9.08 |
| Control | 43.12 ± 7.47 | 41.22 ± 7.31 | 39.67 ± 7.21 | 38.60 ± 6.98 |
Mean and Standard Deviation of DTS and AHI Scores During Different Stages of the Study
The assumption of homogeneity of variance/covariance matrices was checked using Levene’s test. The results indicated that Levene’s test was non-significant for all DTS and AHI scores in the four pre-test, post-test, first follow-up, and second follow-up stages. Result indicates a significant difference in the overall scores of DTS between the experimental and control groups. Moreover, there is a significant difference in the stages (post-test and follow-up) (Table 3).
| Test | Value of Test Statistics | F | Degrees of Freedom | Degrees of Freedom for Error | Eta-Squared | P-Value |
|---|---|---|---|---|---|---|
| Pillai’s Trace | 0.93 | 216.78 | 3 | 36 | 0.936 | 0.001 |
| Wilks Lambda | 0.058 | 216.78 | 3 | 36 | 0.936 | 0.001 |
| Hotelling’s Trace | 18.43 | 216.78 | 3 | 36 | 0.936 | 0.001 |
| Roy’s Largest Root | 18.43 | 216.78 | 3 | 36 | 0.936 | 0.001 |
Result of Mixed Analysis of Variance with Repeated Measures on DTS Scores in Different Stages of the Study
Considering the significant difference in the overall scores between the experimental and control groups, Bonferroni Post-Hoc analysis was conducted to examine the point of difference. The results indicate a significant difference in the mean scores of the DTS between the pre-test and post-test stages, suggesting the impact of the intervention. Additionally, there is a significant difference in the mean scores of DTS between the post-test stage and the first and second follow-up stages, indicating that the magnitude of the intervention’s effect has changed over time (Table 4).
| Stages and Group Comparison | Mean Difference | Standard Error | P-Value |
|---|---|---|---|
| Pretest | |||
| Posttest | - 1.59 | 0.082 | 0.001 |
| First follow-up | - 1.48 | 0.14 | 0.001 |
| Second follow up | - 1.32 | 0.12 | 0.001 |
| Posttest | |||
| Pretest | 1.89 | 0.082 | 0.002 |
| First follow-up | 0.24 | 0.099 | 0.02 |
| Second follow up | 0.32 | 0.096 | 0.002 |
| First follow up | |||
| Pretest | 1.56 | 0.13 | 0.001 |
| Posttest | - 0.19 | 0.096 | 0.023 |
| Second follow up | 0.078 | 0.045 | 0.07 |
| Second follow up | |||
| Pretest | 1.37 | 0.12 | 0.001 |
| Posttest | - 0.98 | 0.093 | 0.002 |
| First follow up | - 0.079 | 0.045 | 0.07 |
Bonferroni Post-hoc Analysis for Between Stages Comparisons of DTS Scores
Results indicates a significant difference in the total scores of AHI between the groups (experimental and control). Furthermore, there is a significant difference between the stages (post-test and follow-up). A mixed analysis of variance (ANOVA) was conducted to examine the point of difference. Table 5 presents the results of the mixed ANOVA with repeated measures on the total scores of AHI in the experimental and control groups, focusing on the pre-test, post-test, first follow-up, and second follow-up stages (Table 5).
| Test | Value of Test Statistics | F | Degrees of Freedom | Degrees of Freedom for Error | Eta-Squared | P-Value |
|---|---|---|---|---|---|---|
| Pillai’s Trace | 0.88 | 226.87 | 3 | 36 | 0.912 | 0.001 |
| Wilks Lambda | 0.049 | 226.87 | 3 | 36 | 0.912 | 0.001 |
| Hotelling’s Trace | 15.13 | 226.87 | 3 | 36 | 0.912 | 0.001 |
| Roy’s Largest Root | 15.13 | 226.87 | 3 | 36 | 0.912 | 0.001 |
Result of Mixed Analysis of Variance with Repeated Measures on AHI Scores in Different Stages of the Study
Abbreviation: AHI, the Ahvaz hardiness inventory.
The results of the Bonferroni post hoc analysis indicate a significant difference in the mean scores of AHI between the pre-test and post-test stages, suggesting the impact of the intervention. Additionally, there is a significant difference in the mean scores of psychological hardiness between the post-test and first follow-up, as well as the second follow-up stages, indicating that the effect of the intervention has changed over time (Table 6).
| Stages and Group Comparison | Mean Difference | Standard Error | P-Value |
|---|---|---|---|
| Pretest | |||
| Posttest | - 1.78 | 0.05 | 0.001 |
| First follow-up | - 1.44 | 0.11 | 0.002 |
| Second follow up | - 1.59 | 0.16 | 0.001 |
| Posttest | |||
| Pretest | 1.56 | 0.087 | 0.001 |
| First follow-up | 0.36 | 0.16 | 0.004 |
| Second follow up | 0.41 | 0.10 | 0.005 |
| First follow up | |||
| Pretest | 1.44 | 0.12 | 0.001 |
| Posttest | - 0.38 | 0.14 | 0.002 |
| Second follow up | 0.021 | 0.04 | 0.027 |
| Second follow up | |||
| Pretest | 0.03 | 0.021 | 0.032 |
| Posttest | - 0.43 | 0.13 | 0.002 |
| First follow up | - 0.34 | 0.12 | 0.01 |
Bonferroni Post-hoc Analysis for Between Stages Comparisons of AHI Scores
5. Discussion
The aim of the present study was to investigate the effectiveness of integrated mindfulness and spiritual therapy on distress tolerance and psychological hardiness among mothers of hard of hearing children. The results of the multivariate analysis of covariance revealed a significant difference in post-test scores of distress tolerance between the experimental and control groups receiving integrated mindfulness and spiritual therapy. Significant differences were also observed in the pre-test, post-test, and follow-up stages. Therefore, it can be concluded that integrated mindfulness and spiritual therapy is effective in enhancing distress tolerance among mothers of hard of hearing children.
This finding suggests that mindfulness, through awareness-raising exercises and focusing techniques tailored to individuals, helps them distance themselves from negative emotions and thoughts, thereby enhancing their distress tolerance.
Spiritual therapy operates by engaging individuals’ beliefs, recognizing that beliefs serve as the bedrock for transforming attitudes and, consequently, behavior. By effecting changes in behavior, more efficacious and sustainable treatments can be achieved. Such beliefs may encompass the recognition of a higher power, faith in an afterlife, and contemplation of existence beyond death, all of which awaken human consciousness and facilitate personal growth. Within this therapeutic framework, it is postulated that the integration of divine and spiritual teachings, particularly the fundamental tenet of monotheism and a profound and sincere connection with the Almighty, along with the insights gleaned from psychological therapy, significantly augment the effectiveness and durability of treatment. Furthermore, the results of the multivariate analysis of covariance indicated a significant difference in post-test scores of psychological hardiness, measured by subscales and total scores, between the experimental and control groups receiving integrated mindfulness and spiritual therapy. Significant differences were also observed in the pre-test, post-test, and follow-up stages. Therefore, it can be concluded that the mindfulness integrated with spiritual therapy is effective in enhancing psychological hardiness among mothers of hard of hearing children. These findings are consistent with the results of the study conducted previous literature (1, 25, 26).
To explain this finding, it can be argued that psychological hardiness is a positive characteristic that allows individuals, through the three components of commitment, challenge, and control, to engage in cognitive coping and problem solving to overcome the difficulties they face. In this approach, individuals reduce the magnification of problems by focusing on reality, being present in the here and now, Running Head: Mindfulness and Spiritual Therapy on Hardiness and Distress Tolerance and dismissing or denying various concerns (such as worries about a child with a learning disorder), perceiving issues as they are rather than as they are perceived to be. As a result, a state of awareness and acceptance is fostered in the individual, leading to resilience and psychological hardiness. This type of training is perceived as a psychological need for all individuals, particularly for mothers with students with learning disabilities. Mothers who can confront challenges and exert control over them have cultivated this conscious and positive belief that they can handle major issues and overcome challenges. However, mindfulness does not solely involve awareness of thoughts; rather, it is an experiential approach to being present in the moment and events without judgment or evaluation.
The practice of mindfulness, in conjunction with the reinforcement of cognitive coping mechanisms such as positive reappraisal and the enhancement of emotion regulation skills like hardiness and distress tolerance, empowers individuals to navigate challenges with psychological hardiness. Specifically, individuals who embrace mindfulness exhibit stability and confidence when confronted with stressful circumstances, and they tend to envision positive possibilities for the future. Moreover, they are inclined to employ problem-focused coping strategies in the face of adversity. Mindfulness techniques activate specific regions of the brain that influence variables including distress tolerance, life management, coping strategies, hardiness, belief systems, and factors contributing to distress. By incorporating attentional self-regulation and present-focused event recognition, mindfulness equips individuals with effective coping strategies to navigate demanding situations. The integration of mindfulness with the cultivation of cognitive coping mechanisms and spiritual practices presents a comprehensive approach to augmenting psychological hardiness. This integration enhances individuals’ ability to manage stress and promote overall well-being. It is evident that religion and spirituality play a significant role in individuals’ psychological well-being by providing cognitive and insight-related strategies. By acknowledging the influence of mindfulness and spirituality, individuals can develop alternative perspectives when evaluating negative events, leading to an increase in psychological hardiness and adaptive coping.
5.1. Conclusions
In conclusion, this study provides compelling evidence that the presence of a healthy child brings joy and energy to life, while caring for a child with disabilities presents unique challenges for the family system. Some previous research demonstrated the efficacy of a combined cognitive-behavioral therapy and spiritual therapy in enhancing coping skills among individuals with anxiety disorders, our findings align with existing literature regarding certain aspects under investigation. Importantly, this study represents a pioneering contribution to the field, as no prior research has specifically explored the mindfulness integrated with spiritual therapy for enhancing psychological hardiness in mothers of hard of hearing children in Iran.
Despite the valuable insights gained from this study, it is essential to acknowledge its limitations. Firstly, our reliance on self-report measures introduces inherent problems, including potential measurement errors and limited self-awareness. Secondly, due to the inability to control for contextual and individual factors, there is a possibility that participants may have overestimated the program’s effectiveness due to various background factors. Additionally, personal inclination and optimism might have influenced participants’ perception of the program’s effectiveness. To address these limitations, we recommend that future studies incorporate placebo-like programs within the control group to control for the influence of expectations and minimize bias.