1. Context
People suffering from chronic conditions have little choice but to care for their health and discipline their lives permanently to minimize the risks of their illness. Activities such as diet monitoring and regular exercise could help such patients over the long term. Diabetes -including type 1 and type 2 diabetes- is among such chronic conditions, with over 90% of the patients suffering from the second type. Global estimates suggest a 50% growth in the prevalence of this disease between 2017 and 2045, resulting in a total of 693 diabetic patients worldwide (1).
Getting type 2 diabetes (T2D) is associated with one's lifestyle, family history, etc. In terms of genome-wide association (GWAS), over 400 genes have been detected to be associated with this disease. However, genetics play a minuscule role (less than 20%) in developing this condition. Studies suggest that self-management and lifestyle change are crucial in treating type 2 diabetes (1).
Self-management helps retain health and reduce risks such as retinal damage, amputation, and cardiovascular diseases (2, 3). Self-management is defined as one's capability in managing symptoms, treatment, physical and socio-psychological consequences, and lifestyle changes associated with the chronic illness they live with (4). Another definition of self-management refers to it as the measures taken by the patient to restore their stable and normal state, returning from a biologically uncertain state to normal life (5). Most definitions of self-management are consistent with Fox and Ward (6) assuming that healthcare users are equipped as "expert patients" by social and healthcare providers to manage their illnesses (7). Others have expanded this notion to "expert families," referring to the family's capability to care for its members in case of vulnerability (8). Some others believe a wider range to be in place at the community scale. Whitehead suggests that a paradigm shift is being made from the hierarchical healthcare model with a biological and medical approach to a more comprehensive and freer model of self-care cooperation by individuals, families, and the community (9).
The present study seeks to identify the social factors affecting type 2 diabetes self-management and discuss how they influence it. The contributed knowledge can help healthcare policymakers increase effectiveness and efficiency when designing and implementing relevant interventions. The impact of one community -i.e., “others” or “people”- can create self-management incentives and help healthcare managers take advantage of this capacity to improve health at the community scale. Recognizing the role of social factors affecting patients as the intermediate between them and the market would enhance self-management (10). The micro-scale social environment of the patient requires rehabilitation, which would not only influence the healthcare process but also support and facilitate health-oriented behaviors of the patient as the patient learns how to correct their consumption. As long as a patient’s family and those around them are at a lower level of the learning process, their activities on the market can challenge the patient’s self-management.
2. Evidence Acquisition
The present study is a review article adopting a narrative approach and was performed in 2022. To conduct the study, the appropriate keywords given the research objective (investigating the influence of social factors on diabetes self-management) including self-management, diabetes, and social factor were first selected using MeSH.
Then, relevant studies were retrieved from reputable databases including Google Scholar, PubMed, Emerald, ScienceDirect and Iran Doc. through a web search (with no temporal limitations). Out of the 18,082 retrieved articles, non-scientific and non-English studies, replications, and studies irrelevant to the research objective were excluded and 68 studies eventually remained. After the collection and analysis of the selected studies, four categories of social factors affecting T2D self-management including family, diabetes educators, peers, and diabetes online communities were identified, which will be further discussed separately as follows.
3. Results
A total of four categories of social factors were identified in the 68 relevant studies retrieved to find the articles relevant to the research objective as mentioned earlier. Out of 68 articles, 19 were focused on the family and how it affected diabetes self-management. Moreover, 15 articles investigated the influences of diabetes educators on diabetes self-management. A total of 20 studies were concerned with the peers and their impact on diabetes self-management. Eventually, the influence of online networks and diabetes online communities took up a considerable portion of the studies with 14 articles.
3.1. The Family
Previous research indicates that adults with type 2 diabetes reported getting support from their families in managing diabetes (11, 12). Further, the diabetic patient’s family members are reported to have actively supported and participated in many diabetes educational interventions (13, 14). The Lorig and Holman model for chronic illness self-management (15) and WHO’s framework for innovative care in chronic diseases (16) both account for families and other social networks as valuable factors in promoting health-oriented behavior, although neither offers any clear definition of how family members provide effective support. Theoretical models used in family-oriented interventions typically include the socio-cognitive model (17) and the family systems theory model (18), both focusing on the interactions between children and parents or students and teachers and overlooking the interactions between adults and their families (19, 20).
A total of ten studies were specifically concerned with the experiences of adults suffering from type 2 diabetes and how their family members affected their diabetes management. Several studies that had not examined the impact of family members directly also contributed to developing the classification of family behaviors.
Family member behaviors from a T2D patient’s perspective are categorized into the three groups of diabetes self-management facilitators, diabetes self-management obstacles, and neutral behaviors with the potential to support or challenge diabetes self-management. Seven subgroups were identified including four facilitators (cooperation in positive care, family's careful conversance, family as an external motivator, and family independence), two obstacles (restraining behaviors and limited family support), and one neutral behavior (regular reminding or nagging).
Family behaviors facilitating diabetes self-management include the following four subgroups:
1. Cooperation in positive care: This refers to behaviors that contribute positively to self-management including a range of shared health-related activities such as doctor’s appointments, exercising, or cooking together (21). This subgroup also includes supporting daily life activities such as driving running errands (22), and financial support (23, 24).
2. Family's careful conversance: Participants in the examined studies held a significant value for family members' help in following up on their medical state, specifically if they suffered from severe hypoglycemia requiring immediate attention. They also cared greatly for the role of family members in diagnosis and helping prevent health decline (25).
3. Family as an external motivator: Participants revealed that the family's external motivation could influence their self-management experience. The willingness to engage in future family events could be a strong incentive encouraging participants to maintain their health and diabetes self-management. The participant may also learn from other family members with the same conditions, be it their positive behaviors or mistakes they could learn from to minimize their risks (22, 26).
4. Family independence: Participants defined the need to grow independent from their families as a means of enhancing their self-management capabilities (27).
Diabetes self-management obstacles are as follows:
1. Restrictive behaviors: Many participants reported the restrictive behaviors of their family members as the primary barrier to their diabetes self-management. Such behavior included manipulating their diet, family members' unhealthy behaviors, or routines that prevented the patient from being consistent in their self-management plan (28). Moreover, participants reported difficulties in self-management when they had to undertake other members'' duties or prepare non-diabetic meals (29).
2. Limited family support: Participants reported inadequate family support including emotional, physical, and financial forms of inadequacy. Limited family support could be due to their busy schedule (30). This can sometimes stem from the family members' low motivation or their lack of understanding of how important such support is. The result of such feelings would be a lack of empathy and understanding between family members regarding the challenges of living with diabetes (31).
Neutral behaviors are as follows:
These behaviors could facilitate or restrict diabetes self-management. Regular reminders from family members could be perceived as helpful or annoying. These reminders are acceptable and valuable as long as they are perceived to be a facilitator by the participants (32). Otherwise, they would be perceived as nagging or even threatening (29, 33).
3.2. Diabetes Educators
Diabetes educators play a prominent part in managing and educating for diabetes. Many educators' primary capabilities are associated with diabetes self-management skills and knowledge, pathophysiology and epidemiology, teaching skills, clinical skills, and cultural capabilities. Research suggests a list of 13 primary capabilities, out of which six items are concerned with diabetes self-management education, accentuating its importance (34). Diabetes self-management education was revealed to encourage self-care, improve clinical results, and reduce hospitalization rates and disease complications (35). Studies indicated that diabetes educators needed a comprehensive understanding of diabetes pathophysiology and epidemiology (36-39). Such knowledge would empower them to establish the necessary sensitivity to diabetes in the community and offer advice to prevent it (39, 40). Diabetes educators need to adopt the capabilities required to design and implement teaching programs. The lack of such abilities would be the main barrier to their effectiveness (41). Moreover, educators need to develop the skills required to connect with patients suffering from mental or physical disabilities (38, 42, 43). Further, they need to reckon whether the educated patient can comprehend the educational material, whether their beliefs contradict the material, or whether they have the ability or determination to make a change. The educators must teach the material in an appropriate language, refrain from complex and scientific terminology, and offer convenient cultural behaviors and nutritional advice (40, 44).
Diabetes educators should also have a wide range of clinical skills (45). One study even pointed out oral health skills (46). The guideline to assess diabetes educators’ capabilities for diabetes nurses published in the UK (47) suggests that this assessment must incorporate a combination of several methods including exams, questionnaires, oral evaluation, practical observation, and care plan revision (48). Diabetes education is considered an imperative component of diabetes management strategies, so diabetes educators play a crucial part in caring for diabetic patients although their effectiveness depends on their diabetes education capabilities.
3.3. Peers
Peer support is a promising strategy to enhance self-management in patients with chronic illnesses such as type 2 diabetes (49-51). Peer support is defined as receiving support from an individual with similar characteristics or similar experience of the disease (52, 53). Diabetic patients and community health workers (CHWs) models are known as two face-to-face peer support models (54). The theoretical context of the peer support models is based on an Integrative model of behavioral prediction due to its potential to alter behavior (55). IMBP is created by developing the theory of planned behavior (55). Selecting diabetic patients as supportive peers (57-62) is focused on patients that control their blood sugar well and possess leading skills, who are selected and recommended by health workers. The choice of community health workers as supportive peers (57, 62-66) is made out of the medical community infrastructure, but the relevant studies have not discussed the criteria for such a choice (62, 63, 65, 66). Educating supportive peers is a vital component in which the educator, training time, and educational material are of extreme significance (57, 58, 61, 63-67). Motivational interview is the most conventional theory to base education on, which is used in interventions considering community health workers as supportive peers (63, 64, 66). Face-to-face groups or supportive peers often use methods such as phone call interventions (60, 62, 66, 67). Supportive peers can be implemented with innovative techniques as a self-management strategy for T2D patients to improve their quality of life (60, 61, 63, 65).
3.4. Diabetes Online Communities and Social Networks
Diabetes online communities are growing quickly as the problems and patients and their need for socio-psychological support remain unresolved. The complex living conditions of the patients and their access to new communicational media (social networks such as Instagram, Twitter, Facebook, Etc.) are contributing to this growth. Peer communities are growingly communicating to gain the necessary support in terms of diabetic lifestyle and valuable health information, which diabetic patients and their families can take advantage of. Furthermore, an analysis of the diabetes online communities reveals valuable information about patients and their families, which has the potential to enhance socio-psychological care (68, 69). Some studies suggested that the use of social networks improved diabetes self-management results (70, 71).
A 2013 study on Facebook posts of diabetic patients found that most individuals sought peer support, information, and emotional support (72). A 2019 study performed diabetes-specific content analysis on several social networks including Instagram, YouTube, and Twitter, and revealed that patients used social networks to gain approval and positive support and build an online community they could use whenever they feel the need to be heard or empathized with (73). Another study found that socio-psychological needs such as the need to belong, loyalty, and being understood led to the use of social networks (74). Another study revealed that patients received emotional support from social networks and thus felt the urge to help others the way they have been helped (70, 75). Participants in another study reported that diabetes online communities helped them feel more understood (79.3%), less alone (75.7%), more empowered (73.1%), and supported through hard times (57.9%) (76). Figure 1 demonstrates a scheme of diabetes online communities' functions in the studies.
Ultimately, research suggests that a study of online social media data would yield a valuable set of individuals information created in a raw and unstandardized manner, which is both the strength of diabetes online communities and their weakness since individuals' information is available in their form of expression rather than from reliable questionnaires (77-79). Still, there would appear to be a significant capability to research diabetes online communities seeking to examine and uncover the psychological needs of the participants, such as the need for peer support and emotional support rarely met by healthcare providers (80). Still, some studies indicated the negative impacts of social networks including misuse, overuse, or false information (81).
4. Discuss
The present review article investigated the social factors affecting self-management in T2D patients. Studies indicated that the four groups of patients’ social interaction included those with family, peers, diabetes educators, and diabetes online communities. Table 1 demonstrates a summary of studies conducted on social factors influencing type 2 diabetes self-management.
| Social Factors | Reference | Influence of Self-management |
|---|---|---|
| Family | (21-24, 26, 27) | Self-management facilitators include cooperation in positive care, family's careful conversance, family as an external motivator, and family-independence |
| (28-31) | Self-management obstacles including restraining behaviors and limited family support | |
| (29, 32, 33) | neutral behavior with the potential to facilitate or challenge diabetes self-management including regular reminding or nagging | |
| Diabetes educators (capabilities) | (34, 35) | Helping the effectiveness of diabetes self-management through diabetes educators’ capabilities inducing: Diabetes self-management knowledge and skills |
| (36-40) | Pathobiology and epidemiology | |
| (41) | Teaching skills | |
| (45, 46) | Clinical skills | |
| (40, 45) | Cultural capabilities | |
| (47, 48) | Educator assessment through exams, questionnaires, oral evaluation, practical observation, and care plan revision | |
| Supportive peers | (38, 49-53, 55-67, 82) | A diabetes self-management strategy seeking to improve self-management in patients, including two models: |
| (57-63) | Diabetic patients’ model: Diabetic patients with good control over their blood sugar and leadership skills are selected as supportive peers | |
| (57, 62-66) | Community health worker model: Uses the medical community infrastructure | |
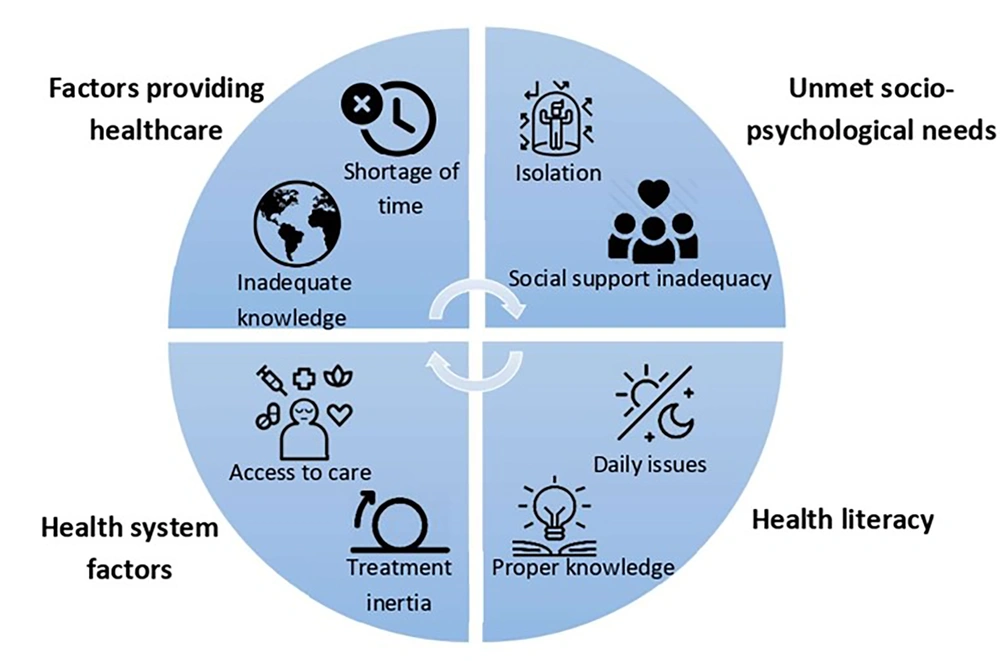
| Diabetes online communities and social networks | (68-71) | Improved self-management results due to functions of diabetes online communities including the four following items: |
| (68-70, 72-76, 80) | Unmet socio-psychological needs: Isolation and inadequate social support | |
| (76-79) | Health literacy: Daily issues and the required knowledge | |
| (68, 69) | Factors providing healthcare: Inadequate time and knowledge | |
| (76-79) | Healthcare system factors: Access to care and treatment inertia | |
| (81) | Negative impacts on diabetes self-management: Misuse, overuse, or misinformation |
A summary of Studies Conducted on Social Factors Influencing Type 2 Diabetes Self-management
Research conducted so far suggests that the family factor influences the consumption behaviors of patients' behaviors facilitating or restricting self-management. This factor may also facilitate or challenge self-management through neutral behaviors. However, this phenomenon has only been investigated from the patients' perspective, leaving the family's viewpoint unexplored. Moreover, previous studies have merely investigated the apparent and overall effects, overlooking the power dynamics, family roles, and other complexities under the surface of these interactions. There is therefore a need for closer inspections adopting a qualitative approach such as the grounded theory to achieve a more comprehensive understanding of this phenomenon, investigate the impact of the family factor on T2D self-management more comprehensively and deeply, and contribute to the development of the “expert family” concept.
Articles focused on diabetes educators or health workers were concerned with capabilities that could help improve diabetes self-management effectiveness. Besides diabetes self-management skills and knowledge (33), pathophysiology and epidemiology, teaching skills, clinical skills, and cultural capabilities were among the capabilities most emphasized in these studies. On the other hand, studies suggested that the capabilities of diabetes educators needed to be assessed through exams, questionnaires, oral evaluation, practical observation, and care plan revision to be improved upon.
Peer support was raised as a promising strategy to enhance self-management in patients with chronic illnesses such as type 2 diabetes. Peer support is defined as receiving support from an individual with similar characteristics or similar experience of the disease. Diabetic patients and CHWs models were introduced as two face-to-face peer support models. The adoption of these models is based on an Integrative model of behavioral prediction, which seeks to alter behavior at the level of personal psychology (81). There appears to be a need for research examining interpersonal and group dynamics going beyond the scale of an individual’s psychology to address how this kind of support impacts diabetes self-management from the group interactions perspective.
The last group of studies concerned with diabetes online communities suggested that social networks introduced a new way to assess diabetic patients' psychological needs (82). These studies suggested that diabetes online communities are growing quickly as the problems and patients and their need for socio-psychological support remain unresolved. The complex living conditions of the patients and their access to new communicational media are contributing to this growth. Peer communities are growingly communicating to gain the necessary support in terms of diabetic lifestyle and valuable health information, which diabetic patients and their families can take advantage of. Furthermore, an analysis of the diabetes online communities reveals valuable information on patients and their families, which has the potential to enhance socio-psychological care. The fact that this information is available on social platforms in the raw form suggests a need for further qualitative research to develop a deeper understanding of the needs of patients and their families. The authors recommend further exploration of this field in independent research given its remarkable growth and the gaps in its literature.
4.1. Conclusions
The influence of others on self-management of diabetes and other chronic conditions that need long-term consumption consideration, persistent diet monitoring, and regular exercise requires deeper research. Despite the valuable pieces of work conducted in this field, there is an evident gap in terms of interpersonal dynamics. Health and social marketing researchers can thus further explore this field to change the increasing slope of the affected population, which has been formed due to the lifestyle and consumption behaviors under the influence of patients' communities soon. It is also suggested to create a theoretical model to classify types of consumer discipline that can be used in health interventions and increase their effectiveness.