1. Background
Laryngoscopy, known as an invasive procedure in the anesthesia process, that by sympathetic nervous system stimulation causes an increase in the release of catecholamines and increase in blood pressure and heart rate, and arrhythmia, which can have dangerous consequences in patients with a history of cardiovascular diseases (1-3). A safe anesthesia for the patient and less stress for anesthesiologists is obtained due to interventions to reduce anesthesia complications. Performing laryngoscopy is one of the first invasive stresses in patients’ anesthesia, which is associated with increased sympathetic activity and occurrence of cardiovascular and hemodynamic pressor responses.
Researchers are still looking at various procedures of attenuation of response to laryngoscopy. Currently, local anesthetics, opioids (especially fentanyl), beta receptor blockers, and calcium channel blockers have been used to manage and reduce hemodynamic complications during tracheal intubation and anesthesia with varying degrees of success (4, 5). Fentanyl is one of the drugs that is usually used together with primary anesthesia for analgesia and suppress reflex response (6). But studies have stated that fentanyl administration alone is not enough to reduce unwanted response (7). Therefore, efforts and clinical research continue to identify more effective drug combinations and protocols to reduce the hemodynamic pressor response caused by laryngoscopy with less risk for the patient.
Nitroglycerin (TNG) is a vasodilator drug that acts on vascular smooth muscle and is rapidly metabolized (8). It also has beneficial effects on reducing preload and afterload in patients with congestive heart failure (9). It has been reported that TNG effectively diminishes the blood pressure in activated sympathetic states and crisis (8). Also, TNG has been introduced as an agent to increase the level of nitric oxide (NO) and cyclic-guanosine monophosphate (cGMP) pathway, which can enhance the effectiveness of fentanyl by the same mechanism mentioned in reducing hemodynamic responses (9, 10). On the other hand, administration of NTG alone before laryngoscopy seems insufficient to reduce hemodynamic responses due to reflex tachycardia effects (11). Therefore, it seems necessary to identify methods and drug compounds with the characteristics of synergistic effects in this field, and as a result, it can be more effectively expected to reduce these responses.
2. Objectives
The present study aimed to compare the efficacy of the combination of fentanyl and TNG versus fentanyl alone on hemodynamic responses induced by laryngoscopy procedure.
3. Methods
This study was conducted as a double-blind randomized clinical trial during the years 2018 - 2019 in Imam Reza Hospital in Kermanshah, Iran. All stages of this research were approved and supervised by the Ethics Committee of Kermanshah University of Medical Sciences (ethics code: IR.KUMS.REC.1398.1202). After presenting the aims and explanations of the study, informed written consent was obtained from the patients. The study information was registered in the Iranian Clinical Trials Registry (IRCT20130812014333N142).
The sample size of the study was forty patients who were candidates for elective surgery in the operating room which requires general anesthesia and airway management. Inclusion criteria include age between 20 and 50 years, no history of underlying diseases such as blood pressure, diabetes, systolic blood pressure above 100 mm Hg, heart and lung disease, no history of smoking and addiction, patients with American Society of Anesthesiologists (ASA) 1 and 2 classification, grade 1 airway. Exclusion criteria include patient bleeding, laryngoscopy for more than 20 seconds or the number of laryngoscopies attempts more than three times, sudden exit of the tracheal tube, occurrence of hypoxia and any heart arrhythmia.
Patients were randomly divided into control and intervention groups, using block number randomization method with concealment of random assignment. Induction anesthesia was done the same in both groups. Ringer serum (7 cc/kg) was given as pre-hydration before induction of anesthesia. Induction of anesthesia by propofol (2.5 mg/kg, intravenously) and muscle relaxation by atracurium (0.5 mg/kg, intravenously) was performed, three minutes before laryngoscopy.
In the control group, a single bolus of fentanyl (2 µg/kg, intravenously) (10) was injected intravenously over a period of 30 seconds, five minutes before laryngoscopy.
In the intervention group, in addition to fentanyl, two puffs of TNG (800 µg) (10) spray were given sublingually, 2 minutes before laryngoscopy.
Study variables were recorded including, systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) by non-invasive monitoring devices at one minute before and after laryngoscopy. Blood pressure was measured from the right arm. The patient and the researcher who recorded the data were not aware of the grouping. Therefore, the study was double blinded.
3.1. Statistical Analysis
Data analysis was done using SPSS version 19 software. Descriptive statistics (mean, variance, and standard deviation), chi-square test, and independent t-test between groups were used. P-value < 0.05 was considered statistically significant in this research.
4. Results
There was no incidence of side effects and no criteria for patient withdrawal from the study. The analysis of data showed that there are no statistically demographic differences between the two groups of patients in terms of age, height, weight, body mass index (Table 1).
at-test.
b Chi-square.
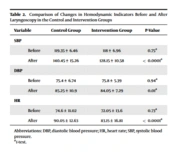
The results of the study showed that there is no statistically significant difference between the study groups in the heart rate, systolic and diastolic blood pressure before laryngoscopy. Data analysis after laryngoscopy using t-test showed that the heart rate, systolic and diastolic blood pressure decreased significantly in the intervention group compared to the control group (Table 2).
Abbreviations: DBP, diastolic blood pressure; HR, heart rate; SBP, systolic blood pressure.
at-test.
5. Discussion
Circulatory and heart system responses related to laryngoscopy can result in morbidity and mortality, particularly in patients with a history of ischemic heart and uncontrolled hypertension (12). Therefore, reducing cardiovascular physiological responses to stress caused by laryngoscopy is one of the important goals and concerns in general anesthesia. The results of our study show that the use of sublingual TNG combined with fentanyl effectively prevented the increase in systolic, diastolic blood pressure and heart rate caused by laryngoscopy stimulation (Table 2). Various previous studies have investigated the effectiveness of techniques and drugs for immediate reduction of laryngoscopy responses. Gupta and Tank demonstrated that fentanyl reduces the hemodynamic response to endotracheal intubation (13). Fentanyl as synthetic narcotic analgesic with a rapid effect onset and short duration of action, has suggested for control of the short lived hemodynamic consequence related to laryngoscopy (14). However, the fear of the side effects of narcotic drugs always limits the variety of their use. Varshney et al. demonstrated the TNG alone was more effective than anesthetic drug in reducing hemodynamic pressor response during intubation (15), which is consistent with the results of our study. Also, the results of the study by Firoozbakhsh et al. have found TNG injection to be effective in preventing unwanted complications of intubation (16). In the study of Channaiah et al. showed that combined using fentanyl and TNG versus fentanyl alone has no significant difference, However, further stated many potentials in the administration of fentanyl and NTG in improving anesthesia complications through prescribing the appropriate dose, anesthesia method, and a combination of these drugs (10).
TNG is used due to less adverse reaction, dilation of coronary vessels, increased myocardial oxygen supply, and also to induce controlled hypotension during some surgeries (17). Fast mucosal absorption, short duration of effect, fast drug clearance and fast therapeutic responses can be considered as a suitable option for modulating hemodynamic responses during laryngoscopy due to its temporary effects. If the patient does not face the risk of bleeding, blood pressure reduction and other causes of prescription contraindications; this drug can be used in the clinical conditions of anesthesia as one of effective attenuators of hemodynamic responses alone or in combination with other interventions. According to the results of various studies, it seems that both drugs can be effective in reducing unwanted hemodynamic changes through different mechanisms. Therefore, exploiting their synergistic effects is a good idea.
5.1. Conclusions
In general, the use of TNG and fentanyl reduced the cardiac and hemodynamic responses caused by invasive laryngoscopy procedure, and the intensity of these reductions was observed more when these drugs were administered in combination. Therefore, it can be suggested that this drug combination be used for safe anesthesia management.
Limitations of the study included the non-assignment of the group without drug intervention because the patients need narcotic drugs in the induction of anesthesia. For the effectiveness of these interventions, more evaluation is needed in patients with high risk of laryngoscopy hemodynamic complications.